Cluster Evaluation of Health Infrastructure Support for First Nations and Inuit
PDF Version (4.1 Mb, 164 pages)
June 28, 2023
Acknowledgements
We wish to honour the traditional territories of the Indigenous Peoples, upon whose land this evaluation has been carried out.
The Algonquin Anishinaabe; The Mississaugas of the Credit; the Anishnabeg; the Chippewa; the Haudenosaunee; the Wendat Peoples; the Huron-Wendat Peoples; the Métis Nation of Ontario; the Métis Nation of Alberta Region 4; the Nehiyaw; the Denesuliné; the Nakota Sioux; Nakota Isga; the Saulteaux; the Anishinaabe and the Niitsitapi.
This evaluation involved engagements which were carried out from coast to coast. We wish to thank the individuals who shared their knowledge, wisdom, and painful truths with us. We thank them for trusting us with their experiences.
Emotional Trigger Warning
This report discusses culturally unsafe experiences in health care, traumatic experiences and health and wellness topics that may trigger memories of personal experiences or the experiences of friends and family. This report also discusses racism, chronic health conditions, and fatality. While the report's intent is to create knowledge and respond to questions about the achievement of outcomes for Cluster programs, the content may trigger difficult feelings or thoughts. Indigenous peoples who require emotional support can contact the 24-hour KUU-US Crisis Line at 1-800-588-8717 to connect with an Indigenous Crisis Responder.
Table of contents
- List of Abbreviations and Acronyms
- Table of Figures
- Table of Tables
- Executive Summary
- Key Findings
- Evaluation Recommendations
- Management Response and Action Plan
- 1. Introduction
- 2. Evaluation Methodology
- 3. Findings
- 3.1 Relevance
- Evaluation Question: What are the needs that this cluster of health programs for First Nations and Inuit should address? Are the needs still relevant and/or have new needs arisen?
- Evaluation Question: Are the objectives of this cluster of programs (i.e., what the programs are designed to do) aligned to the needs of First Nations and Inuit?
- 3.2 Effectiveness
- Evaluation Question: What aspects of the programs are working well and what aspects need improvement?
- Evaluation Question: To what extent has each of the programs included made progress toward the achievement of their respective expected outcomes?
- Evaluation Question: How did the COVID-19 pandemic impact the delivery of the programs and their ability to support First Nations and Inuit?
- Evaluation Question: How effective/productive are the relationships between partners within each of the programs (e.g., between ISC Headquarters and regional offices, First Nations and Inuit, implementing partners, provincial and municipal governments, etc.) and between programs?
- 3.3 Service Transfer
- 3.4 Efficiency
- 3.1 Relevance
- 4. Conclusions
- 5. Recommendations
- Appendices
List of Abbreviations and Acronyms
- AB
- Alberta
- ACCHOs
- Aboriginal Community Controlled Health Organizations
- AFN
- Assembly of First Nations
- ATL
- Atlantic
- BC
- British Columbia
- BCT
- British Columbia Tripartite
- CDC
- Centers for Disease Control and Prevention
- CMA
- Census Metropolitan Area
- CPS&QF
- Canadian Patient Safety & Quality Framework
- CS&H
- British Columbia Declaration on Cultural Safety and Humility
- CSPI
- Canadian Patient Safety Institute
- EAC
- Evaluation Advisory Committee
- eHealth
- eHealth Infostructure Program
- EMR
- Electronic Medical Records
- F – O&M
- Facilities – Operations & Maintenance
- FHQTC
- File Hills Qu'Appelle Tribal Council
- FNHA
- First Nations Health Authority
- FNHMA
- First Nations Health Managers Association
- FNIHB
- First Nations and Inuit Health Branch
- FTE
- Full-Time Equivalent
- GBA Plus
- Gender-Based Analysis Plus
- GCR
- General Condition Rating
- GoC
- Government of Canada
- H&CC
- Home and Community Care
- HFP
- Health Facilities Program
- HHR
- Health Human Resources
- HIV
- Human Immunodeficiency Virus
- HPQM
- Health Planning and Quality Management
- HPQM&SI
- Health Planning, Quality Management and Systems Integration
- HQ
- Headquarters
- HSIF
- Health Services Integration Fund
- HSO
- Health Standards Organization
- HVAC
- Heating, Ventilation, and Air Conditioning
- IELCC
- Indigenous Early Learning and Child Care
- ISC
- Indigenous Services Canada
- ITK
- Inuit Tapiriit Kanatami
- LPN
- Licensed Practical Nurse
- MB
- Manitoba
- MHO
- Ministry of Health and Long-term Care
- MKO
- Manitoba Keewatinowi Okimakanak Inc.
- MMIWG2S
- Missing and Murdered Indigenous Women, Girls, and Two-Spirit People
- MOU
- Memorandum of Understanding
- NATSIHP
- National Aboriginal and Torres Strait Islander Health Plan
- NFR
- New Fiscal Relationship
- NNADAP
- National Native Alcohol and Drug Abuse Program
- NISR
- National Inuit Strategy on Research
- NR
- Northern
- OCAP®
- Ownership, Control, Access, and Possession (referring to First Nations Principles of OCAP®)
- ON
- Ontario
- PIP
- Performance Information Profile
- PT
- Provincial and Territorial
- QC
- Quebec
- QIAP
- Quality Improvement and Accreditation Program
- RMT
- Registered Massage Therapist
- RN
- Registered Nurses
- SCO
- Southern Chiefs Organization
- SK
- Saskatchewan
- SME
- Subject Matter Expert
- STI
- Sexually Transmitted Infection
Table of Figures
- Figure 1 - FNHA depicted the First Nations' perspective of health and wellness (FNHA, n.d.)
- Figure 2 - The Cluster program(s) respect First Nations and Inuit values and rights, including right to access cultural ceremonies, practices, and supports
- Figure 3 - There is an established culture of accountability to advance anti-racism and cultural safety and humility in my organization
- Figure 4 - The Cluster programs allow for services that are safe and free from preventable harm
- Figure 5 - The Cluster programs could be improved for better patient safety and harm prevention
- Figure 6 - Perception of Partners on Overall Effectiveness of Program Delivery
- Figure 7 - First Nation and Inuit Supported by ISC to Develop a Community Health Plan
- Figure 8 - Access to wholistic health services has increased between 2015-2020
- Figure 9 - The quality of care provided is excellent because of HPQM
- Figure 10 - HSIF Projects as of 2022 By Region
- Figure 11 - Sample of HSIF Projects, Types of Integration Covered by Projects Reported
- Figure 12 - HSIF Sample of Projects Focus Areas
- Figure 13 - Access to wholistic health services has increased between 2015-2020
- Figure 14 - The quality of care is excellent because of HSIF
- Figure 15 - There is a high level of satisfaction of services delivered through HSIF
- Figure 16 - Breakdown of Bursary Recipients by Region
- Figure 17 - Breakdown of Bursary Recipients by Programs of Study
- Figure 18 - Annual Percentage Change in Number of Indigenous peoples and Non-Indigenous People Working in Health Care in Canada
- Figure 19 - HFP Program Expenditures
- Figure 20 - Services Enabled by Accreditation
- Figure 21 - Overall Effectiveness of Relationships Between Program Partners
- Figure 22 - Overall Effectiveness of Relationships Between Program Partners
- Figure 23 - Effectiveness of Relationships Between ISC HQ and ISC Regions
- Figure 24 - Effectiveness of Relationships Between ISC Regions and First Nations and Inuit
- Figure 25 - Which relationships need to be strengthened to improve the program's function?
- Figure 26 - Overall Perception of Clarity and Adequacy of the Communication Between Key Program Stakeholders
- Figure 27 - Perception of partners that there is effective communication between program partners
- Figure 28 - The role and responsibilities of this program and its staff are clearly defined, well understood and communicated effectively
- Figure 29 - Information about service transfer is communicated effectively to me and my team
- Figure 30 - Which other health infrastructure support services do you collaborate with to perform your duties?
- Figure 31 - Effectiveness and Productivity of Relationships Between Programs
- Figure 32 - Are there other health infrastructure support services that collaboration with would increase benefits to First Nations and Inuit?
- Figure 33 - First Nations and Inuit who access health infrastructure are equal partners in planning, developing, and monitoring to make sure it meets their needs and to achieve the best outcomes
- Figure 34 - Program Annual Expenditures
- Figure 35 - Number of Program FTEs by Cluster Program Fiscal Year 2015-16 to Fiscal Year 2020-21
- Figure 36 - Staffing is adequate in ISC Regional Offices to support health service(s) delivery
- Figure 37 - Staffing is adequate in First Nations and Inuit communities to support health service(s) delivery
Table of Tables
- Table 1 - Cluster Programs' Expenditure and Full-Time Equivalent
- Table 2 - Evaluation Methodologies
- Table 3 - Limitations
- Table 4 - Self-Reported Health Issues
- Table 5 - Treasury Board Reporting Performance Indicators by Cluster Program
- Table 6 - Number of First Nations Health Facilities and Centres that are Accredited or in Process by Region
- Table 7 - Number of Telehealth Sessions Delivered by Type
- Table 8 - Number of Health Field Bursaries Awarded from Fiscal Year 2015-16 to Fiscal Year 2019-2020
- Table 9 - Number of Award Recipients from Fiscal Year 2015-16 to Fiscal Year 2019-2020, by Indigenous Identity
- Table 10 - Training Provided to Indigenous Community Workers Funded Through HHR from Fiscal Year 2015-16 to Fiscal Year 2020-21
- Table 11 - HFP Progress Against Select Performance Indicators
- Table 12 - Summary of COVID Special Expenditures by Cluster Program
- Table 13 - Summary of FTEs by Cluster Program and Year Over Year Percentage Change
Executive Summary
The Cluster Evaluation of Health Infrastructure Support for First Nations and Inuit was outlined in Indigenous Services Canada's (ISC) Five-Year Evaluation Plan 2020-21 to 2024-25 and conducted in compliance with the Treasury Board of Canada Policy on Results. This Evaluation took the form of a cluster evaluation with six programs in scope from First Nations and Inuit Health Branch (FNIHB). The programs in scope for this evaluation were: Health Planning and Quality Management (HPQM); Health Services Integration Fund (HSIF); Quality Improvement and Accreditation Program (QIAP); Health Facilities Program (HFP); eHealth Infostructure Program (eHealth); and Health Human Resources (HHR). The period covered by the Evaluation was fiscal years 2015 to 2021. In the context of this evaluation, health infrastructure support refers to the various elements of a viable health system, including health planning, accreditation, quality improvement, governance, health facilities, and integration.
The cluster approach allows for a systems perspective, presenting an opportunity to understand how these programs work together and what impacts they collectively contribute. All three streams of enquiry (relevance, effectiveness, and efficiency) were in scope for this Evaluation. Additionally, Service Transfer was evaluated through the lens of all three streams of enquiry.
Several methodologies were used to answer the evaluation questions such as a document and literature review, a survey and a total of 109 interviews made with internal and externals respondents including 6 case studies from across Canada. Evaluation questions that guided the methodology of this evaluation, and associated indicators, can be found in Appendix A – Evaluation Matrix. Limitations occurred in gathering program data and reaching respondents during the 6 months allocated by the study. The tools used to collect data and their limitations are discussed further in the body of this report and in Appendix B – Key Informants and Appendix C – Survey Participants.
Service transferFootnote 1 is defined by ISC as the transfer or shift of control of federally administered programs, policies, and services to First Nations and Inuit-led organizations, supporting self-determination and First Nations and Inuit control in designing, developing, and implementing their own program, services, and policies to address their unique needs and priorities and respect distinct cultural practices. The evaluation recognizes that service transfer is a continuum and can include small "t" transfer (e.g., devolution of single programs to people in First Nations and Inuit communities that may still follow federal government regulations) as well as big "T" transfer (e.g., Health Transformation, where a First Nations or Inuit organization is funded to develop a governance structure and assume full control of the federally funded programs and services). In the context of this evaluation, the findings related to service transfer that are presented are in reference to the full continuum of service transfer to recognize the unique needs of people in First Nations and Inuit communities.
Key Findings
Relevance
First Nation and Inuit have a complex and expansive list of health needs that need to be addressed by the programs in the Cluster and beyond to improve First Nations and Inuit access to quality health care services. People in First Nations and Inuit communities require health services that are identified based on specific community needs, in consideration of social determinants of health, cultural safety and humility, and level of integration across the health services continuum. In order to achieve this, First Nations and Inuit need the resources to overcome externally generated social and policy obstacles that impede access to adequate care.
Both internal and external interviews indicate that the objectives of the Cluster programs are well aligned with the identified health needs of First Nations and Inuit, as well as the Canadian Patient Safety and the Declaration of Cultural Safety and Humility. However, there are significant improvements required in the way the programs in the cluster are designed and delivered to ensure achievement of these objectives through the Cluster programs.
The relevance of the programs, in regard to the needs they were designed to address, is evident. There was a notable trend across the country towards needs for appropriate and adequate health facilities, access to eHealth technologies, trained and educated community-based health care workers, accredited health centres, and improved collaboration between government levels to move towards self-government and autonomy. Yet, the level of need amongst these common areas differed by region and by specific community. Further, First Nations and Inuit have unique needs related to their population demographics and geographical locations. These variations imply that the Cluster programs would be most effective if designed with the appropriate level of flexibility to allow programs to adapt resource allocation to align with local needs.
Relationships
Overall, the relationships between program partners varies significantly between program type and region due to a number of factors such as region-specific agreements as well as program funding levels. Relationships between ISC Headquarters (HQ) and ISC Regional Operations, ISC Regional Operations and First Nations and Inuit, and ISC Regional Operations and Provincial governments were highlighted as the ones most in need of improvement, with partners citing challenges with consistent staff turnover, ineffective communication regarding funding, and lack of engagement. There is a need for increased, intentional collaboration amongst key program partners, with particular attention paid to clarifying roles and responsibilities between ISC HQ and ISC Regional Operations, and improved communications around service transfer (definition and clarity on how to effectively support it). Productive relationships between each Cluster program were noted to be rare, despite a shared ultimate outcome and certain thematic overlaps of services. There is an opportunity to increase the effectiveness and efficiency of the Cluster programs through increased collaboration and knowledge sharing. The importance of relationship building was a consistent trend throughout the evaluation.
Program Outcomes
Program partners noted key challenges that require improvement, particularly around program delivery and administration processes, performance measurement, and reporting. Areas for improvement highlighted included: access to sustainable long-term funding, an improved recognition of local needs, enhanced funding for and focus on training, and First Nations and Inuit awareness of programs. Further, challenges were raised in relation to performance measurement and reporting as a result of data limitations, a misalignment of western data-based reporting approaches to First Nations and Inuit ways of knowing, and the burden of reporting amidst already overcapacity and understaffed health centres in communities.
The value and impact of the Cluster programs, including improving access to and quality of health care for First Nations and Inuit was highlighted by most partners consulted. Interviews indicated that progress has been made towards empowering First Nations to take on the planning and management of health services and building capacity and capabilities within First Nations to prepare for health service transfer.
However, the limited resources, both financial and human, was highlighted as a prominent obstacle impeding the achievement of the Cluster programs' intended outcomes during the evaluation scope period. Additionally, further challenges were highlighted in the impact the pandemic had on timelines and resources, the lack of flexibility of program parameters compared to First Nations' needs, the inability to secure sustainable funding, and the turnover in staff within the Department as an impediment to building lasting relationships and achieving progress towards the Cluster programs' intended outcomes.
Though not initially designed as a Cluster, there is a clear compatibility of the Cluster programs regarding their objectives and desired outcomes. For example, one of the criteria which much be met in order to be accredited, a health centre must put in place a health plan, which is a key output of the HPQM program. Further, to ensure proper physical infrastructure is built in health facilities, eHealth technologies are often required at the onset. Despite the complementarity of program objectives, the programs were found to operate in siloes, with very limited collaboration across the spectrum when delivering programs. This implies an opportunity to improve efficiencies and achievement of progress towards objectives through increased, early collaboration between programs. Consideration should be made to identify points of integration between programs (with each other as well as with other Departmental programming outside of the Cluster) and highlighting opportunities to work together to achieve common goals in shared regions of operation.
The effectiveness of this cluster is dependant on the level of resources invested in actualizing its objectives. There is a disconnect between the scope of the outcomes and the resources available to programs, and in turn First Nations and Inuit, which may be a result of a lack of integrated strategic and operational planning. Consideration should be made to review the priorities of the Cluster programs as a system while aligning with the new Departmental Results Framework put in place starting 2023-24 and assessing the feasibility and identifying opportunities to increase efficiencies within programs.
Best Practices
Based on external research and interviews, the evaluation noted the following best practices and lessons learned, particularly with regards to how the Cluster programs' design and delivery can be improved:
- The importance of data collection was noted as valuable to understand changes over time. In particular, supporting First Nations and Inuit data sovereignty is required to ensure information that is shared truly reflects First Nations and Inuit needs and priorities, including access to culturally safe health care.
- The value of building respectful and longstanding relationships with First Nations was repeatedly emphasized in interviews, along with a clear understanding of the Department's role. It was noted that two-way feedback facilitates an understanding of what aspects are working well for First Nations and what is not.
- Building communication mechanisms and networks for First Nations and ISC staff alike to share knowledge, best practices, and lessons learned was highlighted as valuable in supporting continued progress. Interviews also emphasized the role that effective documentation of knowledge by both ISC staff and people in First Nations communities plays in supporting knowledge transfer and building expertise.
- Breaking down barriers between services, sectors, organizations, and levels of government is key to promoting a more wholistic view of health care service delivery for First Nations and Inuit. There are opportunities for ISC programs to be better integrated to address social determinants of health.
These best practices are aligned to ISC's vision and mandate for health service transfer.
Impacts of COVID-19
The pandemic highlighted the severity of health needs of people in First Nations and Inuit communities as well as shortages and inequities related to access to appropriate health facilities, eHealth technologies, skilled community-based workers, and governance and planning structures to manage public health crises.
The global pandemic had significant impacts in the delivery of health services to First Nations, including limiting both access in and out of communities during lockdown measures and diverting resources towards pandemic response and away from other existing health needs and priorities. However, positive impacts were also noted, including a notable increase in efficiency in both funding releases from the federal government and program delivery, as well as an increase in demand and appreciation of the value of the intended outcomes of programs, particularly eHealth, Accreditation and Health Facilities. It also highlighted opportunities for innovation in program design and application of resources. The Cluster programs spurred the consideration of lessons learned, particularly around emergency preparedness and key priorities in health services delivery.
The COVID-19 pandemic served as the ultimate representation of the value of appropriately governed health facilities with the expertise, capacity, and resources to have emergency preparedness and crisis management plans in place. It also allowed First Nations and Inuit demonstrate what they are capable of when adequately supported. The ability of people in First Nations and Inuit communities, with support from ISC, to pivot and adapt rapidly in order to carry out the pandemic response in addition to meeting regular health needs was commendable. Programs were creative in leveraging new partners to provide added value to the pandemic response. For example, HHR partnered with the Red Cross and the First Nations Health Managers Association (FNHMA) Help Desk for Indigenous Leadership to provide First Nations with a trustworthy communication channel through which they could seek advice or be directed to the necessary resources to help them navigate the pandemic, independent of the government. Prioritization of the pandemic response resulted in increased efficiency and innovations undertaken by people in First Nations and Inuit communities. Moreover, the challenges faced by health services such as the inability to access communities in lockdown, labour shortages, or the lack of connectivity for virtual services, demonstrated the critical value of what the Cluster programs aim to achieve.
Evaluation Recommendations
Therefore, it is recommended that ISC:
- Leveraging existing needs assessments, engagement efforts, and consultations, develop a funding approach that addresses funding gaps and provides flexibility and sustainability to the programs evaluated.
- FNIHB works with First Nation and Inuit partners to co-develop and begin to implement a strategy – including identifying partners, approach and timing – to build capacity among Indigenous health leaders, health service providers, and supporting roles to increase opportunities for training and knowledge sharing between communities.
- To allow for uniform and flexible program application to equitably serve communities, FNIHB must:
- Perform an assessment of internal human resourcing to inform an internal human resources strategy in FNIHB that appropriately staffs and retains employees within the programs evaluated; and
- Create mechanisms to ensure program staff have common knowledge and understanding between and within evaluated programs and foster ongoing opportunities for knowledge exchange.
- In order to achieve a more wholistic and effective approach to service transfer, an alignment and integration between evaluated programs within FNIHB and ISC's broader vision of service transfer is required. It is recommended that FNIHB works with First Nations and Inuit, as well as ISC Strategic Policy Sector and Regional staff, collaborate to:
- Develop a workplan to communicate the evaluated programs' visions of transfer that are aligned with department's service transfer approach and vision; and
- Conduct an assessment that identifies commonality and redundancies between evaluated programs to support integration of programs and gradual transfer of services.
- FNIHB works with partners to develop a meaningful performance measurement strategy with the Chief Finances, Results and Deliver Officer Sector's (CFRDO) Results and Delivery Unit and supporting data collection and management strategy with Chief Data Officer (CDO) and Chief Information Officer (CIO) to support Indigenous data sovereignty in health services.
Management Response and Action Plan
Evaluation Title: Cluster Evaluation of Health Infrastructure Support for First Nations and Inuit
Management Response
This Management Response and Action Plan (MRAP) has been developed to address recommendations resulting from the Cluster Evaluation of Health Infrastructure Support for First Nations and Inuit, which was finalized by ISC Evaluation. This Evaluation took the form of a cluster evaluation, grouping together six programs in scope from First Nations and Inuit Health Branch (FNIHB). The programs in scope for this evaluation were: Health Planning and Quality Management (HPQM); Health Services Integration Fund (HSIF); Quality Improvement and Accreditation Program (QIAP); Health Facilities Program (HFP); eHealth Infostructure Program (eHealth); and Health Human Resources (HHR). Although the British Columbia Tripartite Relations program was not formally evaluated as part of this cluster evaluation, it was included in the scope with the intent to learn from its design and delivery model and glean best practices and lessons learned related to transfer of health services. The period covered by the Evaluation was fiscal years 2015 to 2021.
The cluster approach allows for a systems perspective, providing the opportunity to understand how programs work together and what impacts they collectively contribute. Since the commencement of the evaluation, the Department updated its Departmental Results Framework as of April 1, 2023, realigning its programs inventory, including the creation of the new Health Systems Support Program, aligning the e-Health Infostructure sub-program as part of the Primary Care Program and aligning the Health Facilities sub-Program, as part of the Community Infrastructure Program.
FNIHB recognizes the key findings highlighted by the evaluation related to the following themes: relevance of the programs, program outcomes, relationships, best practices, and impacts of COVID-19.
The evaluation provides five recommendations, all of which are accepted by FNIHB, and the attached Action Plan identifies specific activities to implement these recommendations.
The Department has reviewed and assessed the recommendations and will proceed with their implementation over a two-year period and in the context of Indigenous partners' visions and priorities, expressed during two foundational engagements that are underway –
- engagement with Indigenous partners on the co-development of distinctions-based+ Indigenous health legislation to improve access to high-quality, culturally-relevant and safe health services; and
- engagement on the design and implementation of the Indigenous Health Equity Fund.
An annual review of this Management Response and Action Plan will be conducted by the Departmental Evaluation Committee to monitor progress and activities.
| Recommendations | Actions | Responsible Manager (Title / Sector) |
Planned Start and Completion Dates |
|---|---|---|---|
|
We agree with this recommendation. Equitable, adequate, sustainable, inclusive, and flexible funding that is available to Indigenous Peoples is one of the 9 key themes conveyed by Indigenous Peoples about the state of Indigenous health in Canada and their vision of what to include in distinctions-based+ Indigenous health legislation to improve access to high-quality, culturally-relevant, and safe health services. In particular, Indigenous groups want more direct funding models, fewer reporting burdens, and funding formulas that are holistic and needs-based. While Indigenous health legislation provides the approach to redesign and rethink existing Indigenous health funding models more broadly, as well as to secure funding for Indigenous groups that is equitable, adequate, sustainable, inclusive and flexible, existing needs assessments of program areas within the evaluation provide a basis for initial efforts to address some of these changes. In this regard, the following actions could be taken:
|
|
Start Date: Completion: |
|
We agree with this recommendation. Supporting and building capacity in health human resources is one of the 9 key themes conveyed by Indigenous Peoples about the state of Indigenous health in Canada and their vision of what to include in distinctions-based+ Indigenous health legislation to improve access to high-quality, culturally-relevant, and safe health services. In particular, Indigenous partners identified the need for health care workers to develop locally-based cultural competencies to provide person-centred care and build relationships between providers, clients and communities. Indigenous partners have highlighted the importance of mandatory training in Indigenous cultural competency, anti-racism, anti-oppression and trauma-informed care. FNIHB is committed to continue working with First Nations and Inuit partners to identify and co-develop initiatives that support locally-based cultural competencies, training availability, knowledge sharing and enhancement of capacity among health Indigenous leaders and service providers. In this regard, the following actions could be taken:
|
|
Start Date: Completion: |
|
We agree with this recommendation. FNIHB is continuously exploring new and innovative retention and recruitment strategies, such as the nursing health human resources framework. In addition, together with Regions, FNIHB is implementing human resourcing priorities under Better Together – an organizational culture initiative that aims to foster an environment that supports all FNIHB staff and promotes wellness in our work while also addressing barriers and behaviours that negatively impact wellness. These priorities include:
In this regard, the following actions could be taken:
|
|
Start Date: Completion: |
|
We agree with this recommendation. The Department is committed to working in partnership with Indigenous Peoples to advance the priorities of First Nations and Inuit, including those of intersectional groups (i.e., Indigenous youth, women, urban, and 2SLGBTQQIA+ Peoples), when it comes to healthcare and ensuring improved access to high quality, culturally relevant, safe care. To this end, in 2019, the Government of Canada committed to hearing from Indigenous Peoples to identify those priorities and consider whether and how they might be advanced by means of federal legislation, as well as to working together to co-develop potential legislative options to address them. The co-development of distinctions-based+ Indigenous health legislation is an opportunity to advance the following objectives:
In this regard, the following actions could be taken:
|
|
Start Date: Completion: |
|
We agree with this recommendation. To set the appropriate context for our response, the Department has updated its Departmental Results Framework as of April 1, 2023, realigning its programs inventory, including the creation of the new Health Systems Support Program, the e-Health Infostructure sub-program (as part of the Primary Care Program) and the Health Facilities sub-Program (as part of the Community Infrastructure Program). This work has led to the current review and update of the branch's Performance Information Profiles (PIPs), which encompass performance measurement strategies in collaboration with the CFRDO Results and Delivery Unit. In this regard, the following actions could be taken:
While remaining respectful of partners' own priorities and goals related to Indigenous data sovereignty in health services, over the next 2 years FNIHB will continue to remain abreast of discussions with partners (e.g., First Nations Information Governance Centre (FNIGC) information sharing mechanisms) led by the CDO and CIO through established governance / committees / tables as part of departmental efforts regarding control and transfer of data. In this regard, the following actions could be taken:
|
|
Start Date: Completion: |
1. Introduction
The overall purpose of the evaluation was to examine a set of health infrastructure support programs at Indigenous Services Canada (ISC) (or the 'Cluster') in fulfilment of ISC's Five-Year Evaluation Plan 2020-21 to 2024-25 and Treasury Board of Canada requirements for program evaluations.
This Evaluation is taking the form of a cluster evaluation to determine if ISC's expected outcomes are being met; to support ISC with alleviating a backlog of evaluations due under the Treasury Board Section 42.1(1) of the Financial Administration Act requirements; and to alleviate the burden on program areas by only evaluating programming once in the next five-year period. The cluster approach allows for a systems perspective, allowing for the opportunity to understand how programs work together and what impacts they collectively contribute.
There are six programs that compose this cluster, all delivered by FNHIB. A short profile of these programs objectives and outcomes are presented below. The overarching logic model developed by ISC Evaluation for this cluster of programs (hereinafter referred to as "the Cluster") is outlined in Appendix D – Cluster Logic Model.Footnote 2 All programs noted below, except eHealth Infostructure Program, are delivered to First Nation and Inuit. However, delivery to Inuit is limited to only a few projects in most instances. eHealth Infostructure Program is only delivered to First Nations.
Health Planning, Quality Management and Systems Integration (HPQM&SI) Program: This program administers funding agreements and direct spending to increase the capacity of First Nations and Inuit to design, manage, evaluate, and deliver health programming.Footnote 3 The focus of the program is on health planning by First Nations and Inuit for First Nations and Inuit and thus directly contributes to the overall goal of "increasing the capacity of First Nations and Inuit to design, manage, evaluate, and deliver health programs and services".Footnote 4
The program includes the following three sub-programs:
- Health Planning and Quality Management
- Health Services Integration Fund
- Quality Improvement and Accreditation
-
Health Planning and Quality Management (HPQM)
This program provides guidance to regions, who in turn work directly with First Nations and Inuit on creating health and wellness plans. The program provides funding for these plans through funding agreements. This program collaborates with the First Nations Health Managers Association (FNHMA) to develop tools to support community health and wellness planning and provides national oversight and support to FNIHB regions for funding arrangement management and health and wellness planning. The program also supports improving health services and programming by incorporating quality improvement activities in health programs (e.g., accreditation and evaluation of health programs).Footnote 5
-
Health Services Integration Fund (HSIF)
This fund supports collaborative planning and multi-year projects aimed at better meeting the healthcare needs of First Nations and Inuit by working with provincial and federal levels of government and creating partnerships to integrate federally and provincially/territorially funded health services in First Nations and Inuit communities; improving access to healthcare for First Nations and Inuit; and increasing the participation of First Nations and Inuit in health programming design, delivery, and program evaluation. HSIF is regionally implemented throughout the country with participation and support from the regional advisory committees in some regions.Footnote 6
-
Quality Improvement and Accreditation Program (QIAP)
The program contributes to advancing the self-determination and capacity for health services for people in First Nations and Inuit communities that meet their needs to improve health outcomes. The program accomplishes this by facilitating the uptake of accreditation and recommending Quality Improvement activities to increase community-based health human resource capacity of First Nations and Inuit to design, manage, evaluate, and deliver health programs and services.
Health Facilities Program (HFP)
This program aims to support the delivery of health programs and services through investments in health infrastructure. It provides funding to eligible recipients for: planning, design, construction, acquisition, leasing, expansion, renovation, security services, and/or operation and maintenance of health infrastructure. The program also funds preventative and corrective measures to improve the condition of health infrastructure or to maintain or restore compliance with building codes, environmental legislation, and occupational health and safety standards. These activities aim to provide First Nations and Inuit with the space required to deliver healthcare services safely and efficiently for First Nations and Inuit. Health infrastructure includes health facilities, substance use / addiction treatment centres, Aboriginal Head Start On-Reserve (AHSOR) space, health professional residences / accommodations and support infrastructure. These buildings support the delivery of health programs and services.
eHealth Infostructure Program (eHealth)
The objective of the eHealth Infostructure Program is to provide the "right information to the right people at the right time" to support First Nations in being connected, informed, and healthier, and to enable front-line healthcare workers working in First Nations and Inuit communities to improve First Nations and Inuit health through eHealth programming.Footnote 7
The goal of the activities currently being carried out by the eHealth program is to improve the efficiency of health care delivery to First Nations through the use of eHealth technologies for the purpose of defining, collecting, communicating, managing, disseminating, and using health data.Footnote 8Footnote 9
Health Human Resources (HHR)
This program contributes to the strengthening of Indigenous social services, including healthy living and child development, community care, kindergarten to post-secondary education services, familial support, and communicable disease prevention.Footnote 10
The program's objectives are to increase the number of First Nations, Inuit, and Métis practicing in healthcare, and to increase the number of qualified individuals working in healthcare delivery in First Nations and Inuit communities. The program is delivered through two streams: the first provides scholarships and bursaries for Indigenous students pursuing health careers and is delivered in partnership with Indspire, and the second provides training and certification for community-based workers and health managers to improve the quality and consistency of healthcare services in First Nations and Inuit communities.Footnote 11
In addition to the six programs evaluated as part of this Cluster, the British Columbia Tripartite Relations (BCT) was included in this evaluation, not to evaluate its performance but rather to learn from the model experience. The BC Tripartite Relations program is intended to promote tripartite relationships between the federal and provincial levels of government with First Nations. The objective of this program is to enable the First Nations Health Authority (FNHA) in BC to develop and deliver quality health services to First Nations living in BC that feature closer collaboration and integration with provincial health services. As the BC Tripartite Relations was evaluated recently (in 2019), the Cluster evaluation noted any best practices and/or lessons learned from the BC Tripartite Relations to support the objective of the evaluation. The BCT may serve as a model for new models of health service delivery systems across the country and its impact on systems integration may provide valuable lessons learned on further transfer of other activities.
A summary of the Cluster's programs' expenditure and full-time equivalent (FTE) informationFootnote 12 over the evaluation period is provided in the tables below.
| Cluster Programs | Program Expenditures | |||||
|---|---|---|---|---|---|---|
| Fiscal Year 2015/16 | Fiscal Year 2016/17 | Fiscal Year 2017/18 | Fiscal Year 2018/19 | Fiscal Year 2019/20 | Fiscal Year 2020/21 | |
| Health Planning and Quality Management (HPQM) | $108,307,252 | $111,311,408 | $116,762,360 | $132,531,553 | $125,635,240 | $131,437,339 |
| Health Services Integration Fund (HSIF) | $8,061,749 | $19,586,573 | $14,498,900 | $37,661,337 | $41,355,707 | $40,365,229 |
| Quality Improvement & Accreditation (QIAP) | $5,203,010 | $5,329,828 | $5,598,299 | $6,333,099 | $5,684,666 | $6,143,294 |
| Health Facilities Program (HFP) | $89,444,707 | $167,948,252 | $197,348,222 | $172,439,143 | $148,278,066 | $149,189,768 |
| eHealth Infostructure Program (eHIP) | $24,367,982 | $25,910,204 | $26,874,347 | $25,725,674 | $28,038,393 | $30,889,468 |
| Health Human Resources (HHR) | $5,753,907 | $5,651,730 | $8,796,364 | $5,808,989 | $5,901,977 | $2,722,649 |
| Cluster Programs | Program FTEs | |||||
|---|---|---|---|---|---|---|
| Fiscal Year 2015/16 | Fiscal Year 2016/17 | Fiscal Year 2017/18 | Fiscal Year 2018/19 | Fiscal Year 2019/20 | Fiscal Year 2020/21 | |
| Health Planning and Quality Management (HPQM) | 32.34 | 35.64 | 30.61 | 23.00 | 27.60 | 32.20 |
| Health Services Integration Fund (HSIF) | 7.85 | 5.82 | 5.87 | 3.17 | 2.45 | 2.76 |
| Quality Improvement & Accreditation (QIAP) | 7.09 | 8.36 | 4.00 | 2.35 | 3.22 | 5.00 |
| Health Facilities Program (HFP) | Not applicable | Not applicable | Not applicable | 48.08 | 48.94 | 57.39 |
| eHealth Infostructure Program (eHIP) | 27.66 | 27.58 | 22.88 | 20.69 | 22.21 | 24.46 |
| Health Human Resources (HHR) | 1.60 | 1.50 | 0.02 | 0.31 | 0.00 | 0.00 |
2. Evaluation Methodology
2.1 Scope and Evaluation Issues
All three streams of enquiry (Relevance, Effectiveness, and Efficiency) were in scope for this Evaluation. Additionally, Service Transfer was evaluated through the lens of all three streams of enquiry. The period covered by the Evaluation was fiscal years 2015 to 2021. In the context of this evaluation, health infrastructure support refers to the various elements of a viable health system, including health planning, accreditation, quality improvement, governance, health facilities, eHealth, and integration.
Service transferFootnote 13 is defined by ISC as the transfer or shift of control of federally administered programs, policies, and services to First Nations and Inuit-led organizations, supporting self-determination and First Nations and Inuit control in designing, developing, and implementing their own program, services, and policies to address their unique needs and priorities and respect distinct cultural practices. The evaluation recognizes that service transfer is a continuum and can include small "t" transfer (e.g., devolution of single programs to people in First Nations and Inuit communities that may still follow federal government regulations) as well as big "T" transfer (e.g., Health Transformation, where a First Nations or Inuit organization is funded to develop a governance structure and assume full control of the federally funded programs and services). In the context of this evaluation, the findings related to service transfer that are presented are in reference to the full continuum of service transfer to recognize the unique needs of people in First Nations and Inuit communities.
The following questions guided the methodology of this evaluation. A complete list of questions, indicators and evaluation methods is found in Appendix A – Evaluation Matrix.
Relevance:
- What are the needs that this cluster of health programs for First Nations and Inuit should address? Are the needs still relevant and/or have new needs arisen?
- Are the objectives of this cluster of programs (i.e., what the programs are designed to do) aligned to the needs of First Nations and Inuit?
- Is the departmental goal of service transfer aligned to the needs of First Nations and Inuit?
Effectiveness:
- To what extent has each of the programs included made progress toward the achievement of their expected outcomes?
- How did the COVID-19 pandemic impact the delivery of the programs and their ability to support First Nations and Inuit?
- How have the programs in the Cluster worked towards ensuring the eventual transfer of departmental responsibilities to First Nations and Inuit, as mandated by the department?
- What aspects of the programs are working well and what aspects need improvement?
- How effective/productive are the relationships between partners in each of the programs (e.g., between ISC Headquarters and regional offices, First Nations and Inuit, implementing partners, provincial and municipal governments, etc.) and between programs?
Efficiency:
- How cost effective is the design and delivery of the programs included in this health infrastructure support cluster?
- Are there ways to make them more cost effective?
- Is the allocation of funding to and within each of the programs appropriate to achieve the expected outcomes?
2.2 Design and Methods
The evaluation was led by a team from the Evaluation Directorate within ISC. The Methodology Report was finalized in May 2022, with primary data collection occurring from June 2022 to January 2023.
The evaluation used a mixed methods approach and gathered data through various lines of evidence, including:
| Methodologies | Description |
|---|---|
| Documentation, program data, and file review | The evaluation team reviewed documentation to collect both quantitative and qualitative data related to ISC's processes and activities. This included Performance Information Profiles (PIPs), program performance data as available, previous evaluation reports, as well as any additional documentation identified during interviews. |
| Literature and media review | The evaluation team conducted a review of literature and media publications related to elements of First Nations health governance and infrastructure on reserve and in the Northern Territories of Canada, and in relation to impacts of COVID-19. Literature within both the domestic and international contexts was reviewed. Over 50 external literature sources were reviewed, including: journal articles; academic reports; non-governmental organization reports; and relevant journal, newspaper, and online media articles. |
| Key informant interviews and focus groups (n=109) |
The objective of key informant interviews and focus groups was to collect in-depth information, performance data, and stories based on stakeholder experiences with one or more of the Cluster programs. Semi-structured interviews were conducted with a purposeful sample of internal key informants, including:
A total of seven (7) focus groups were conducted with ISC Regional Staff. One focus group per program was held, and representatives from each region per program were in attendance. The total number of participants across all focus groups was 57. Semi-structured interviews were conducted with a stratified random sample of external key informants, including:
For participants who declined the request to be interviewed, the Evaluation Team accepted written responses to the interview questions. A total of 6 written responses were collected. In total, 109 key informants were engaged with to provide information for this evaluation. |
| Survey |
A survey was administered to both internal and external respondents to gather both qualitative and quantitative data for the evaluation. 74 total responses (16 from First Nations Representatives; 18 from Implementing Partners; and 40 from ISC Regional Staff) were received. Participation in the survey was voluntary and as such is not representative of the perceptions of the entire population of internal and external program partners. |
| Case studies (n=6) | The objective of the case studies was to gain an in-depth understanding of First Nations' experiences with the Cluster programs as well as identify any potential lessons learned in program delivery. Each case study involved interviews, documentation review, and external research. 6 of 6 selected case study contacts completed interviews. |
The lines of evidence and their relationship with Key Evaluation Questions are outlined in Appendix A – Evaluation Matrix. Appendix E – Case Study Background Information provides additional details on the case studies represented in this report.
This evaluation faced challenges that limited a complete appraisal. The limitations of the evaluation and their associated mitigation strategies are described below:
| Limitations | Mitigation Strategy |
|---|---|
| Lack of a robust performance measurement strategy: Through consultations with ISC staff, the evaluation noted that the program indicators used to assess performance (as defined in the PIPs) were not consistently used. Program performance information may not have been collected, tracked, monitored, or reported on in a consistent manner (i.e., within the evaluation scope period), or the programs noted that the indicators were no longer relevant and were in the process of updating their PIPs. This limited the amount of quantitative data the evaluation was able to analyze and report on.Footnote 16 |
|
| Inconsistency in external interviewee regional coverage and low interview participation rate: There were challenges in obtaining a consistent and high external interviewee (e.g., First Nations Representatives, Implementing Partners) participation rate across all regions. Some ISC staff were unable to provide the evaluation team with contact information for external partners. Some external partners either chose not to participate or did not respond to the participation request. |
|
| Issues with quantitative data quality: Given FNIHB’s programs moved from Health Canada to Indigenous Services Canada during the evaluation period, different IT systems and coding were used to manage funding and human resources. For the evaluation, this resulted in issues with data consistency. |
|
2.3 Project Governance
The evaluation team used a participatory and consultative approach through engagement with an Evaluation Advisory Committee (EAC) chaired by the Director of Evaluation. Members of this committee were made up of directors within ISC who are responsible for the oversight of the Cluster programs in FNHIB. They, along with representatives from the Assembly of First Nations (AFN) and Inuit Tapiriit Kanatami (ITK), commented on the purpose and scope of the evaluation, the key evaluation questions, and the evaluation methodology. Committee members were asked to: review the methodology report, including the data collection instruments; validate quantitative data and the evaluation preliminary findings following data collection; and review the draft evaluation report.
3. Findings
3.1 Relevance
Evaluation Question: What are the needs that this cluster of health programs for First Nations and Inuit should address? Are the needs still relevant and/or have new needs arisen?
To conduct this assessment, it is necessary to ensure a wholistic understanding of what the health needs of First Nations and Inuit are in the present day, and how they may have evolved since 2015 (the beginning of the evaluation scope period).
IndigenousFootnote 17 peoples in Canada face significant inequities in access to and quality of health care services. The First Nations Health Authority depicted a First Nations' perspective of health and wellness visually (as seen in Image 1), encompassing several elements, including: social, economic, environmental, and cultural.Footnote 18 Based on both the western and Indigenous perspectives of the wholistic definition of health, a sufficient understanding of the core health needs of First Nations and Inuit requires consideration of the social determinants of health, the specific barriers to access, and the specific health crises that First Nations and Inuit face as a result.
Text alternative for Figure 1 - FNHA depicted the First Nations' perspective of health and wellness (FNHA, n.d.)
Figure 1 is an image depicting a First Nations perspective of health and wellness. At the center of the figure is a five ring circle, with the inner most circle representing the human being, the second ring illustrating emotional, mental, spiritual, and physical, the third ring represents wisdom, respect, relationships, and responsibility; the fourth ring represents family, land, nations, and community, and the outermost ring, represents environmental, social, economic, and cultural health and wellness. Outside of the circle there are 21 silhouettes of people holding hands.
Finding #1: First Nations and Inuit experience significant social inequities that greatly impact access to quality and culturally safe health services.
The Government of Canada (GoC) acknowledges health and social inequities faced by Indigenous peoples in Canada.Footnote 19 The quality of an individual's health is heavily influenced by socioeconomic factors, with studies demonstrating that social determinants of health can account for 30-55% of health outcomes.Footnote 20 Half of all interviewees engaged in this evaluation highlighted the importance of understanding the social determinants of health, and the necessity to address these needs in order to see meaningful and sustainable improvements to Indigenous access to high quality health services. Specifically, interviewees and literature emphasized the need to address housing, economic adversity, connectivity, and racism and discrimination in the health care system to improve access to health and improved health outcomes for Indigenous peoples.
Indigenous Peoples face Insufficient Quality and Quantity of Housing
Canadians are currently facing a severe shortage of affordable housing, with housing demand significantly increasing from 2016 to present, while housing supply has not maintained the same pace.Footnote 21 As of 2021, 35.7% of First Nations living on reserve and 52.9% of Inuit living in Inuit Nunangat live in unsuitable and inadequateFootnote 22 housing.Footnote 23
56% of First Nations Representatives engaged in this evaluation specifically highlighted the impact that the acute shortage of housing has had on the health of First Nations, and the ability of health care workers to provide adequate care. The lack of housing availability, adequacy, and suitability impacts health, including health conditions (e.g., mould leading to asthma), increased spread of viral diseases due to overcrowding (e.g., as during the COVID-19 pandemic), and even leads to increased gender-based violence.Footnote 24 According to key informants, the lack of housing availability has also impacted communities' and health centres' abilities to recruit and retain health care staff as they are unable to offer temporary and stable housing in the community. As such, when Indigenous peoples seek education in health care professions, they are often required to leave the community to access employment opportunities and training. This further exacerbates existing challenges in the recruitment and retention of qualified health professionals in community to provide culturally safe and accessible care to remote or rural Indigenous patients.
Indigenous Peoples face heightened rates of Economic Adversity
The economic statusFootnote 25 of any individual has a significant impact on their ability to maintain their health and access services when needed. Notwithstanding the direct link economic status has to one's ability to access other key social determinants of health (i.e., ability to afford housing, food, and/or education) which impacts health status, it also directly affects an individual's ability to afford services that are not covered by provincial or territorial health insurance.
Indigenous peoples throughout Canada face higher rates of economic adversity.Footnote 26 First Nations and Inuit contend with barriers including higher cost of living (particularly in remote and rural areas), lower opportunity for employment, and lower comparative incomes.Footnote 27 Living in poverty has strong ties to substance use and increased violence in communities, which in turn impact both the physical and mental health of those residing within these communities, resulting in greater need for emergency services and mental health support programs.
Indigenous Peoples continued to face Social Exclusion, Anti-Indigenous Racism, and Discrimination
Social Inclusion
Experts categorize social inclusion as a determinant of health, as research shows that social exclusion can negatively impact both access to care and mental health and wellness.Footnote 28 Social exclusion is a result of social inequities, typically dictated by the way certain populations are marginalized and systemically excluded through social and economic policies and systems. Canada has acknowledged that Indigenous peoples are among four populations of people who have been denied equitable access to social services, including health, housing, and education.Footnote 29 To support addressing the social determinants of health, social prescribing was introduced to with the goal to increase collaboration between clients, staff and community providers to develop solutions. Social prescribing intends to function as a tool to complement medical care.Footnote 30
Anti-Indigenous Racism
Anti-Indigenous racism refers to racism directed specifically to Indigenous individuals. According to interviews, anti-Indigenous racism has both direct and indirect impacts on the health of people in First Nations and Inuit communities. Indigenous peoples have long been subjected to discrimination and poor treatment due to the deep-rooted and severely harmful assumptions and negative stereotypes that are directed at them. The federal government acknowledges that Indigenous peoples in Canada continue to face racism and discrimination in the healthcare system.Footnote 31 For example, a common stereotype is that Indigenous people experience substance addiction challenges (i.e., alcohol and drugs), and as a result, Indigenous patients are often dismissed or ignored when they seek medical help with symptoms assumed to be alcohol or drug-related. In many cases, Indigenous peoples face violent and hateful treatment in the health care system, leading to increased trauma, dismissal of medical challenges by health care professionals, and fear of seeking care.
According to research conducted and shared by a First Nation subject matter expert (SME), the trauma of colonialism and continued racism faced by Indigenous peoples have intergenerational repercussions that manifest through higher likelihood of physical maladies. Countless instances of abuse and mistreatment of Indigenous peoples within the health care system have resulted in preventable fatalities. Interviewees noted the need for prioritizing the recruitment and retention of human resources who are equipped to provide culturally safe care and support Indigenous peoples accessing safe and traditional medical practices and healing.
Further to physical health impediments, research has shown racism and discrimination can cause intense stress and trauma in victims.Footnote 32 These conditions are often linked to deeper mental illnesses (i.e., anxiety, depression) and can even cause addictions to alcohol or drugs.
As such, a significant number of interviews (29%), particularly among First Nations Representatives (67%) and Implementing Partners (60%), highlighted the need for trauma-informed, culturally sensitive health care services, citing racism and discrimination as a major barrier to health care for Indigenous peoples nationwide.
Indigenous Women and Girls
While being a member of any one designated group (e.g., women, persons with disabilities, racialized groups, etc.) already creates numerous barriers, the challenge becomes even greater when considering the impacts of intersectional identitiesFootnote 33. When assessing the impact of Indigeneity on access to health services, it is important to consider the unique challenges faced by Indigenous people who also identify as members of other designated groups. In particular, Indigenous women were highlighted by interviewees as a group that experiences challenges that differ from both Indigenous men and non-Indigenous women.
Callout Box 1: Research demonstrates that:
- The lack of access to culturally-responsive care exacerbates health concerns related to chronic illness and increases the need for additional health care providers. For example, a lack of access to care for diabetes results in additional need for foot care specialists.Callout Box 1 note 1
- Approximately 40% of First Nations adults on reserve are living with diabetes, compared to 8.9% of the general population.Callout Box 1 note 2
- Indigenous peoples are 2 times as likely to develop cardiovascular disease than non-Indigenous Canadians. Research also shows that First Nations and Inuit patients generally have heart attacks earlier in life.Callout Box 1 note 3
- For 14 of the 15 most common forms of cancer, First Nations have lower five-year survival rates than other populations in Canada.Callout Box 1 note 4
- The rate of tuberculosis is 50 times higher among Inuit and 5 times higher among First Nations than the national Canadian average.Callout Box 1 note 5
- In Canada, Indigenous people account for 5% of the populationCallout Box 1 note 6, yet 5-8% of reported HIV cases.Callout Box 1 note 7
Before colonization, many Indigenous women and girls held positions of leadership and decision-making in their respective populations, which were significantly harmed by forcible alteration of matrilineal practices and the denial of rights for Indigenous women under the Indian Act. The National Inquiry into Murdered and Missing Indigenous Women and Girls (MMIWG) notes that Indigenous women and girls are almost twice as likely to face violence than non-Indigenous women, with almost six in every ten Indigenous women and just over three in every ten non-Indigenous women having experienced physical assaultFootnote 34Footnote 35 Furthermore, it is imperative to consider the additional health services required for people with uteruses. Indigenous women and girls, those identifying as two spirit, women, gender fluid, or non-binary with uteruses have additional health needs which may include pregnancy and childbirth.
Finding #2: First Nations and Inuit in Canada experience a disproportionate level of medical challenges, including chronic illnesses and mental health and wellness conditions.
Interviewees noted particular medical conditions and challenges that are most prevalent amongst Indigenous populations, which includes the following:
Chronic Illnesses and Multi-Morbidities
Throughout interviews, partners discussed the medical conditions and illnesses that were most prevalent for First Nations and Inuit. The heightened incidence of chronic illness and multi-morbidities among Indigenous peoples is added to by literature.
Chronic Conditions
A significant number of First Nations respondents (33%) noted that obesity, cancer, diabetes, and other chronic illness continuously impacted the overall health and wellness of First Nations and Inuit. More specifically, several partners noted diabetes as a core health need, with statistics validating that Indigenous populations are diagnosed with diabetes earlier in life, with more severe symptoms at the time of diagnosis, and also experience higher rates of complications and worse treatment outcomes than non-Indigenous Canadians.Footnote 36 The increased prevalence of diabetes among First Nations and Inuit results in greater need for appropriate staff and equipment to support with preventative care and treatment, and education initiatives in Indigenous populations. Further, the symptoms of diabetes can increase the need for other specialists (i.e., for foot care treatment).
Self-reported rates of long-term chronic health conditions and their prevalence among Indigenous populations are outlined below:
| Self-Reported Health Issues | Proportion of General Population | Proportion of Indigenous Peoples (Statistics Canada, 2022) |
|---|---|---|
| Long-Term Health Problems | 44%
(16.8 million people)Footnote 37 |
57%
(568,940 people) |
| Asthma | 9.9%
(3.8 million people)Footnote 38 |
14.3%
(142,540 people) |
| Arthritis | 20%
(6 million people)Footnote 39 |
20.1%
(200,590 people) |
| High-Blood Pressure | 19.6%
(7.5 million people)Footnote 40 |
17.5%
(175,200 people) |
Communicable Diseases
A select number of interviewees (7%) noted sexually transmitted infections (STIs) and tuberculosis as additional core health issues experienced by First Nations and Inuit within their communities. In the case of tuberculosis, it was noted that the housing shortage and lack of capacity to support isolation of contagious patients results in increased numbers of the disease among First Nations and Inuit in their communities.
Mental Health and Wellness
Content Warning: This section may cause distress for some readers.
The number of Indigenous peoples impacted directly or indirectly by mental health and wellness challenges continues to grow.
Case Study #1
File Hills Qu'Appelle Tribal Council (FHQTC)
Region: SK | Program Focus: Health Planning; HSIF; eHealth
The All Nations Healing Hospital and FHQTC Health Services operates the Miko-Mahikan Red Wolf program (further described in Case Study #3) and began as a response to the rising prevalence of homelessness, addiction struggles, and overdose within the 11 Nations represented by the File Hills Qu'Appelle Tribal Council (FHQTC). Miko-Mahikan operates a harm-reduction program, addiction support, opioid replacement therapy, and education, awareness, and outreach programming to support patients. In part, some of the operations of the Hospital, including pharmacy, women's health and low risk birthing was supported by HSIF funding.
Trauma
Traumatic experiences and intergenerational trauma are linked to mental health challenges in First Nations and Inuit populations. Historically and to this day, Indigenous peoples have endured trauma from a number of sources, which include but are not limited to colonialism, residential schools, forcible removal of children from their families, racism and discrimination. In addition, Missing and Murdered Indigenous Women, Girls, and Two-Spirit People, and the persistent impacts of residential schools are all examples provided by interviewees as traumatic events that continue to exacerbate mental health challenges for themselves and people in their communities. According to the Calgary-based Mental Health Literacy Organization, mental health challenges are also linked to substance use challenge and suicide.Footnote 41
Substance Use & Addiction
Interviewees noted particularly acute challenges with alcohol and drug dependencies faced by First Nations and Inuit throughout Canada. Socioeconomic factors, including poverty, homelessness, and lack of access to social services and education are known contributors to substance dependence and addiction struggles. Literature also notes the impact of substance use and addition on exacerbation of homelessness, poverty, and barriers to access to social services.Footnote 42
Suicide
Statistics illustrate that youth suicide rates are higher among Indigenous youth than non-Indigenous youth in Canada. Suicide rates for First Nations people are three times higher than that of non-Indigenous people at 24.3 deaths per 100,000 person-years at risk.Footnote 43 The rates of youth suicide among Inuit is nine times higher than that of non-Indigenous people, at 72.3 deaths per 100,000 person-years at risk.Footnote 44
Finding #3: First Nations and Inuit communities have limited access to appropriate community-based health resources, including facilities, equipment, programs, staff, and training.
As noted in Finding #1 and Finding #2, accessFootnote 45 to health care is a significant challenge faced by people in Indigenous communities.
Community-Based Care
Due to the rural and/or remote nature of many Indigenous communities, the nearest health care center for First Nations and Inuit is often not close to their home. The lack of community-based care can, therefore, be the difference between life and death when seeking treatment for health-related issues. This is even more difficult where ambulatory services or transport treatment is unavailable, or in some instances as shared by interviewees, provision of service is refused near reserve communities.
Regional Specific Needs
Interviewees and literature review also note the unique needs faced in urban, rural and remote, and Northern communities. In urban settings, Indigenous peoples often experience a lack of cultural sensitivity when interacting with health care workers, as well as an overall lack of healthcare capacity and funding for health care services. In rural, remote, and Northern communities, there are increased difficulties with recruiting and retaining health care staff. In Northern communities the unique climate can cause limited or obstructed access to community by road (where road access exists), creating interrelated challenges of recruiting and retaining health care staff, climate impacts can result in a higher probability of certain medical conditions (e.g., respiratory and cardiovascular illness)Footnote 46 manifesting as well as increase challenges in housing or health facility construction and maintenance.
In order to ensure timely access to care, it is vital that people in communities have adequate and suitable facilities within the community, with the functioning equipment to provide health services.
According to interviews, many communities lack the physical space to operate facilities that support the level of health service delivery required, with some noting that their only option was to operate health services in closets or church basements. It was noted that some communities continue to not have access to clean waterFootnote 47, a necessity for an appropriate health facility.Footnote 48 In one Focus Group, it was noted that over 80% of one region's health facilities inventory had not been renovated/repaired since 2000, highlighting the need for renovations and repairs to maintain adequate facilities in which to provide care. The outdated nature of many of these buildings create additional challenges when attempting to outfit facilities with the necessary technology to operate effectively in the current society.
Furthermore, it was highlighted in interviews that facilities are not always equipped to allow for traditional and cultural practices, either as a result of limited financial and resource capacity or actual barriers in the physical infrastructure of the buildings (i.e., Heating, Ventilation, and Air Conditioning (HVAC) system for smudgingFootnote 49), which sometimes relates to adhering to codes and/or standards in building construction and/or operation. When considering the adequacy and suitability of community-based health facilities, it is important to consider what the specific needs of the patients in that area are, and in the case of Indigenous communities, access to traditional medicine is a core need. One of the key challenges Indigenous peoples have faced is erasure of their culture and traditions, and an imposition of assimilation to western practices. For health facilities to truly meet the needs of the Indigenous communities, they must reflect community needs and values.
Community-Based Health Care Workers
In order to provide adequate and timely care, community health facilities require an appropriate level of staff. Most interviewees (58%) noted that there is a shortage of health care workers and limited health care capacity in communities. Partners noted an acute need for additional community-based workers to deliver health services and emphasized in these discussions that there have been ongoing challenges with recruiting and retaining health care staff in communities. These challenges include a lack of funding to allocate to salaries and benefits, a lack of interest from staff in remaining in-community (due to working conditions), and a lack of housing capacity to provide shelter for external health care workers. The lack of accommodation for health care workers in Northern regions was specifically noted as a key issue in one focus group. Interviewees highlighted a need for early education opportunities to encourage and support Indigenous youth to pursue careers in healthcare to support sustainable measures to overcome these continuous staffing shortages.
Appropriate Training & Expertise for Community
Most interviewees (55%) noted a specific gap in having access to health care workers with appropriate expertise, training, and cultural sensitivity. A select number of SMEs who participated in interviews recounted the challenges in hiring nursing staff, and how in their absence, communities have worked to train paramedics to ensure that they have the basic capabilities to treat patients in community rather than sending them to the provincial health center. In addition, due to the lack of training provided, even when staff have the appropriate tools, they would likely not be able to use them. Program partners also noted that community health directors have voiced the need to improve skillsets to support Licensed Practical Nurses (LPN), including training for various fields, including therapy, registered massage therapy (RMT), acupuncture, reflexology, dental hygiene, and child and youth counselling. It was emphasized that while there is great need for frontline health care workers, such as nurses and doctors, there is also need for support workers, including nursing informatics and digital technicians, particularly as the demand for remote, digital health services grows. Due to the distance between provincial health facilities and communities, there is often a need for speciality doctors (e.g., oncologists, endocrinologists) in community that continuously remains unmet.
Further, the need, and current lack of, culturally trained health practitioners was a key trend in interviews. A significant number of First Nations Representatives (44%) and SMEs (50%) noted that racism and discrimination in the healthcare system remains an ongoing issue. Given this, as well as trauma endured in the healthcare system, First Nations and Inuit patients require services delivered by individuals trained in cultural humility. Ideally, community-based staff would be members of the Indigenous community and would therefore have the necessary understanding of cultural sensitivities. Moreover, First Nations and Inuit patients require health services professionals who practice two-eyed seeing when providing care, including the strengths of both culturally-specific medicine and western medicine.
Technological InfrastructureFootnote 50
In today's technology-fueled society, particularly in the post-pandemic environment, having virtual access to health care services is vital. As such, the electronic infrastructure in communities is key to their ability to access, and professional's ability to provide, digital care. Throughout interviews with both internal and external partners, connectivity was highlighted as a key ongoing challenge for First Nations and Inuit communities in a significant number (25%) of discussions. Specifically, it was noted by First Nations Representatives and Implementing Partners that even when the required technology is implemented and deployed, the communities are challenged to connect to the required networks. Given the numerous barriers to accessing health services in person (further explored throughout this report), communities require the capability to communicate with health professionals virtually through reliable networks. The absence of this can result in patients not receiving timely, life-saving care.
Additionally, the health facilities located in communities need to be able to electronically communicate with each other. Appropriate health care requires a complete understanding of a patient's medical history. This data is typically shared among health care practitioners through the patient's Electronic Medical Record (EMR).
From the perspective of community members seeking care, connectivity is required to connect with health professionals, regardless of physical residence. From the perspective of health practitioners within the communities, connectivity is required to conduct daily operational activities efficiently, monitor and store patient data, and perform medical procedures. It was specifically noted by one First Nations Representative that many health centers in communities still use paper systems, and as a result, they are inefficient and exposed to critical patient safety issues. If medical data is illegible or misplaced, this can result in very serious consequences for the impacted patients. With already such limited capacity and resources in the health centres, inefficiencies result in time taken away from being able to attend to patient needs.
Maintenance
Another key challenge highlighted by partners was the level of maintenance required to keep technological equipment up to date. Technology is rapidly evolving and as such, hardware and software often require regular updates. The pace at which e-infrastructure investments are evolving is not matching the evolution of technology, meaning that even where communities have access to technology, it is often outdated. Further, there is a need for properly trained staff with the ability to operate the technology, and support with education initiatives, support evolving technologies, and maintain hardware, as needed.
Data Management and Sovereignty
Under the umbrella of the identified need for Indigenous peoples to lead the direction of their own health services, the need for data sovereignty must be considered, particularly as it relates to health data management through digital health technologies such as electronic medical records (EMRs). This also considers the First Nations principles of Ownership, Control, Access, and Possession (OCAP®), which asserts that First Nations alone should have control over data collection processes and how data is then stored, interpreted, used, or shared,Footnote 51 and the National Inuit Strategy on Research (NISR), outlining the five priorities to facilitate Inuit Nunangat research in an efficient, impactful, and meaning manner.
The movement of health data is vital to patient health, as is the integrity of the privacy around health data. As such, it is important for Indigenous communities to control the level of access others have to their data. A significant number of First Nations Representatives (22%) and Implementing Partners (20%) noted the need for data sovereignty and governance as it relates to OCAP® principles.
Further, from an efficiency perspective, interviewees noted the need to ensure appropriate data management and sharing practices are in place to ensure health practitioners have access to the data they need to provide adequate care.
Health Care Services Continuum
The highest quality health care is continuous, proactive, and comprehensive. Health services should exist on a continuum, with consideration given to preventative, emergency, and aftercare, as well as access to related or complementary health services.
Promotion and Prevention Care
As a result of the many barriers to access health services, it is highly common for First Nations and Inuit to fall ill to more severe conditions or in some instances, succumb to preventable diseases. According to interviews, this is directly linked to an absence of appropriate health care promotion and early prevention care in communities. Health promotion initiatives work to communicate the value of healthy practices, in many areas, including mental health and wellness, as well as education and identification of indicators of specific conditions or illnesses. In order to avoid the continuation of challenges in the areas of mental health and substance use, interviewees noted that communities would benefit from increased ongoing and preventative programming that supports community members prior to reaching the point of requiring medical attention.
Emergency Services
In addition to the gaps identified in prevention and after care, interviews also indicated a need to improve access to emergency services. This was noted in relation to a lack of appropriate emergency transportation, such as ambulances or helicopter evacuation options, for remote communities. In a health emergency, response time can heavily impact prognosis and probability of survival, and the absence of accessible emergency services for remote communities can result in a higher rate of patient fatality.
Long-Term Care
Another theme that emerged throughout interviews was the need for enhanced long-term care in communities. While the Indigenous population of Canada is overall younger than non-Indigenous Canadians, the Indigenous population is projected to age faster, due to a shorter estimated life expectancy.Footnote 52 As the aging Indigenous population continues to grow, access to long-term care has become a greater challenge, yet health care funding is often not sufficient to include such areas of care. Elder populations tend to require more frequent and specific types of care, which leads to increased need for health care professionals with those skillsets, facilities that can accommodate patients, and appropriate funding to provide both. Furthermore, Indigenous peoples tend to favor aging-in-placeFootnote 53; however, this requires adequate levels of health professionals to provide live-in or home-visit medical care.
Cultural Safety and Humility
Cultural safetyFootnote 54 and cultural humilityFootnote 55 are vital to ensuring an equitable health care system. A culturally safe and humble environment requires an absence of racism and discrimination, and an understanding and respect of Indigenous cultures. This includes an integration of traditional and cultural practices in health services.
Traditional Practices
Indigenous cultures have traditional healing practices that differ from those commonly applied in western cultures. Traditional healing and wellness are defined by the FNHA as "health practices, approaches, knowledge and beliefs that incorporate First Nations healing and wellness".Footnote 56 These practices often incorporate the use of natural remedies, ceremonies, and energetic therapies.Footnote 57
Partners emphasized that to provide genuinely effective, inclusive, and complete care to Indigenous populations, health services need to make space for traditional medical practices. While this was a gap noted by a significant number of interviewees (43%) in current health centres, some First Nations Representatives and Implementing Partners shared ways in which these practices have been incorporated in their community health centres, which has included Elders and Knowledge Keepers being onsite to encourage smudging and praying.
Finding #4: The scope of health needs of First Nations and Inuit have remained consistent over the time period of the evaluation (2015-2021); however, the level of need has been further exacerbated by external factors, most prominently the COVID-19 pandemic.
Since the conduct of the last evaluation of these programs in 2015, health needs of First Nations and Inuit have been exacerbated, largely due to the impacts of the COVID-19 global pandemic. Indigenous peoples, due to existing unmet health needs, suffered additional acute impacts from the pandemic.
The spread of COVID-19 was exacerbated by ongoing issues related to overcrowding, inadequate housing conditions, homelessness, and water and food insecurity, as described in further detail in Finding #1. The virus also exacerbated existing underlying conditions and was particularly dangerous for those who have chronic illnesses or compromised autoimmune systems, both of which are issues that are already prevalent among Indigenous peoples. As such, in addition to treating patients with COVID-19, health care centres were also overwhelmed with the aftercare requirements of those suffering from long-term impacts, while new COVID-19 cases still continued to rise.
Impact of COVID-19
The pandemic exacerbated the existing social inequities that contribute to the barriers Indigenous peoples face in accessing high quality health care services. Economic challenges associated with lockdown measures impacted individuals financially, forced both temporary and permanent closures of businesses, closure of schools and childcare centres, and left many people struggling to balance caring for families, homeschooling children, and navigating the economy. The economic impact of COVID-19 pressured unemployment rates and increased the incidence of homelessness throughout Canada. Studies distinctly demonstrated disproportionate impacts to marginalized communities throughout the pandemic, Indigenous peoples being one of these populations.Footnote 58
The measures implemented to reduce the spread of the virus resulted in a number of additional consequences to the health of First Nations and Inuit communities. Overcrowding made isolation mandates very challenging. 20% of interviewees recounted higher than average mental health and wellness needs during the pandemic, as well as an increase in number of individuals seeking support for substance use and addiction.
Positive Outcomes
Case Study #2
Onion Lake First Nation
Region: Treaty 6 Territory, SK & AB | Program Focus: Health Planning; HSIF; HFP; eHealth
Individuals living in circumstances of overcrowding were presented with extreme challenges associated with attempting to medically isolate after they or a person living with them had contracted COVID-19. Representatives of Onion Lake First Nation noted that COVID-19 heightened the prevalence of homelessness within the Nation. In response to this, the Nation purchased isolation trailers which were available to community members for isolation purposes, in order to combat not only the spread of COVID-19, but also the harmful impacts of being unhoused.
Interviewees (ISC staff as well as First Nations Representatives and Implementing Partners) noted that there were positive outcomes or best practices that could be taken from the COVID-19 pandemic and applied in the future. These best practices focused on the flexibility in reporting requirements, the enhanced communication, and ease of transfer of funding. Many interviewees indicated that if these processes were as efficient on an ongoing basis as they were during COVID-19 response efforts that their relationships with ISC staff would be strengthened.
One key example provided by interviewees of a positive outcome of the COVID-19 pandemic was the support for the adoption of virtual care. As a result of lockdowns, mandatory quarantine, and the impact for the healthcare system to deliver services in-person (e.g., elective surgeries), much of healthcare pivoted to digital delivery which made care more accessible for some individuals. Program Leads and Implementing Partners noted an increase in demand for certain services, particularly the Quality Improvement and Accreditation program and connectivity for eHealth programming. Many interviewees also noted the positive impact that being accredited had on their organization, including emergency preparedness and crisis management planning that is part of the accreditation program.Footnote 59
Evaluation Question: Are the objectives of this cluster of programs (i.e., what the programs are designed to do) aligned to the needs of First Nations and Inuit?
Finding #5: The Cluster programs support the principles of the Declaration on Cultural Safety and Humility and the Canadian Patient Safety and Quality Framework strategically; however, there is minimal integration of these elements within the design of programs.
Note:
This finding does not apply to the QIAP.
Both the Canadian Patient Safety & Quality Framework (CPS&QF) and the British Columbia Declaration on Cultural Safety and Humility (CS&H) are frameworks that outline the objective of improving equity in health care to ensure all Canadians have access to quality health care services. These frameworks present standards through which to assess the level of consideration both patient safety and cultural safety have been given in the Cluster programs. One of the objectives of this evaluation was to understand the extent to which the Cluster programs are aligned with the principles outlined in the CPS&QF and the Declaration.
British Columbia Declaration on Cultural Safety and Humility
The CS&H was signed by the FNHA in 2015 as a commitment to advance cultural safety and humility within health organizations delivering services to Indigenous peoples.Footnote 60
The Declaration is based on the following guiding principles of cultural safety and humility:
- Cultural humility builds mutual trust and respect and enables cultural safety;
- Cultural safety is defined by each individual client's health service experience;
- Cultural safety must be understood, embraced, and practiced at all levels of the health system including governance, health organizations and within individual professional practice.
Truly effective health care should make the patient feel safe, both from a medical competency and a cultural standpoint. In addition to interviews, this evaluation included a survey conducted with both internal and external partnersFootnote 61 in order to capture insights from those unable to participate in interviews. This survey included a number of questions that specifically related to the alignment of the Cluster programs to the CS&H principles.
As described previously throughout the Relevance section of this report, the mistreatment of Indigenous peoples can often lead to either a lack of appropriate attention or treatment from health professionals or an avoidance of health facilities from Indigenous patients, which can ultimately result in delayed and misdiagnoses or preventable fatal illnesses.
Despite these identified gaps, survey data indicated that the majority of both internal (72%) and external (60%) partners agree or strongly agree that the Cluster program(s) they are involved with allow for wholistic support including the right to access cultural practices.
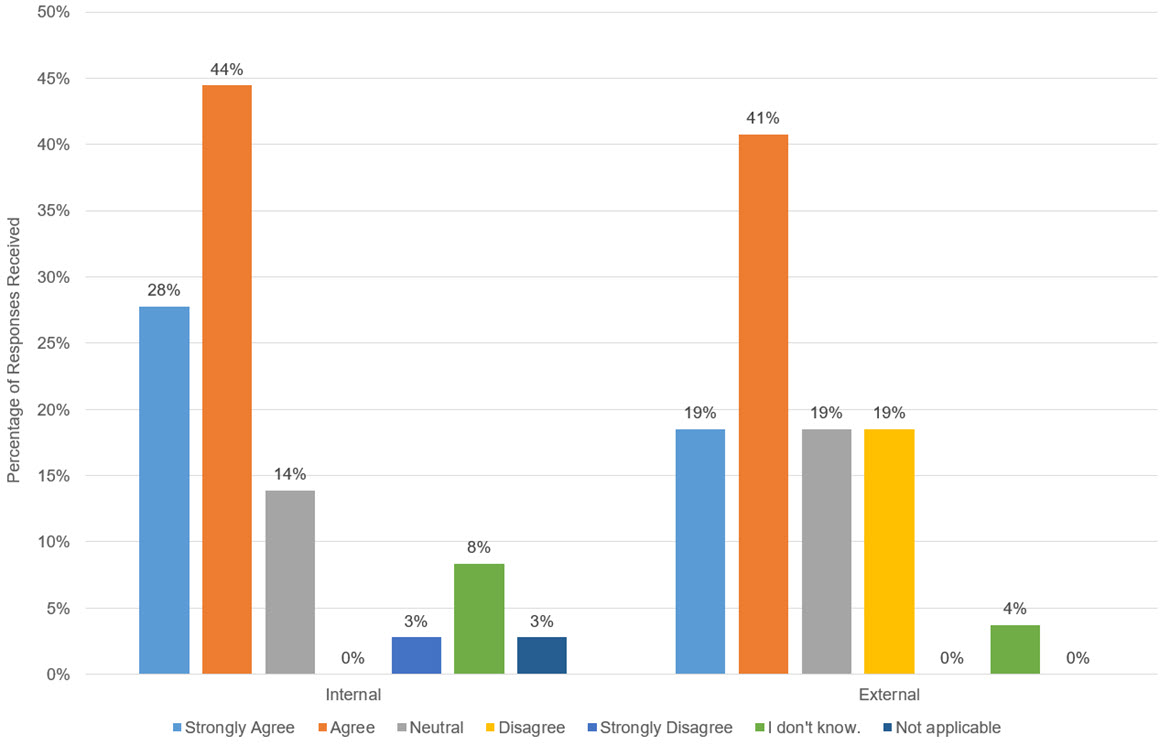
Text alternative for Figure 2 - The Cluster program(s) respect First Nations and Inuit values and rights, including right to access cultural ceremonies, practices, and supports
Figure 2 is a bar chart that illustrates survey results in response to the statement "The Cluster program(s) respect First Nations and Inuit values and rights, including right to access cultural ceremonies, practices, and supports". Responses were on a scale include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (28%), Agree (44%), Neutral (14%), Disagree (0%), Strongly Disagree (3%), I don't know (8%), and Not Applicable (3%). External (to ISC) responses were Strongly Agree (19%), Agree (41%), Neutral (19%), Disagree (19%), Strongly Disagree (0%), I don't know (4%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
While the objectives of the programs align with these principles, there were several gaps shared throughout interviews, including a lack of appropriate training of staff on cultural humility (ISC internal staff and health centre staff) and a lack of consideration of traditional medicine practices in infrastructure of health facilities that indicate room for improved integration in execution. It was highlighted in interviews that the need for cultural humility is required in all roles, including those that do not operate directly with patients. This includes roles internal to ISC, as well as those in implementing partner institutions who play a role in defining program objectives/parameters and developing resources and frameworks within which communities operate health services.
The survey also asked if respondents felt as though there was an established culture of accountability to advance anti-racism and cultural safety and humility in their respective organizations, to which the majority of both internal (66%) and external (52%) partners agreed.
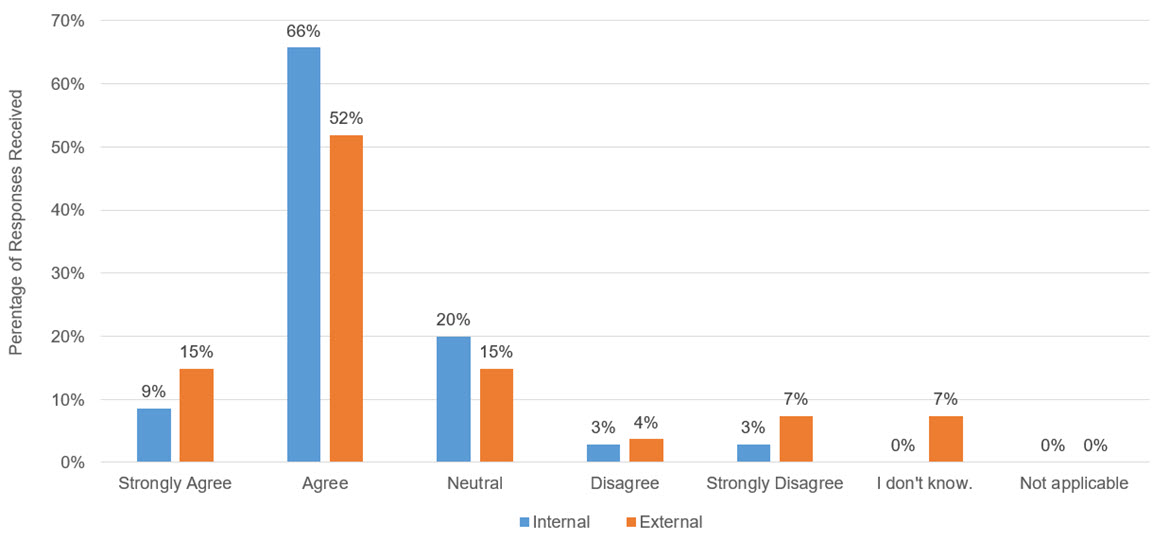
Text alternative for Figure 3 - There is an established culture of accountability to advance anti-racism and cultural safety and humility in my organization
Figure 3 is a bar chart that illustrates survey results in response to the statement "There is an established culture of accountability to advance anti-racism and cultural safety and humility in my organization". Responses were on a scale include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (9%), Agree (66%), Neutral (20%), Disagree (3%), Strongly Disagree (3%), I don't know (0%), and Not Applicable (0%). External (to ISC) responses were Strongly Agree (15%), Agree (52%), Neutral (15%), Disagree (3%), Strongly Disagree (3%), I don't know (0%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
Additionally, approximately half of internal (49%) and external (52%) respondents responded "Agree" in response to a question asking if their respective organizations have processes to manage feedback or reports of harm on racism-related, quality and safety issues.
The data gathered in interviews and surveys suggest that while opportunities to improve the level of prioritization of cultural humility and patient safety in the design and delivery of health programs remain, Cluster program partners and communities have worked to apply these principles as much as capable within program restraints.
Canadian Patient Safety and Quality Framework
The Canadian Patient Safety and Quality Framework was developed in 2018 by the Health Standards Organization (HSO) and the Canadian Patient Safety Institute (CSPI) in order to align quality and safety improvement across Canada.Footnote 62
The CPS&QF is guided by the following principles:
- Patient care is as safe as possible across the country, and efforts are made to prevent, respond to, and learn from a patient safety incident;
- Jurisdictions and organizations have mechanisms for measuring and monitoring safety;
- Patients, families, and the public are actively engaged and empowered;
- Supportive and engaged leadership promotes a culture of safety;
- A caring and just culture is established at all levels of Canadian health care; and
- The health workforce is engaged and supported.
When asked about perception of whether current services were safe and free from preventable harm, survey responses were more varied, with internal and external groups voting Agree (26% and 33%), Neutral (20% and 30%) and Disagree (23% and 19%), respectively.
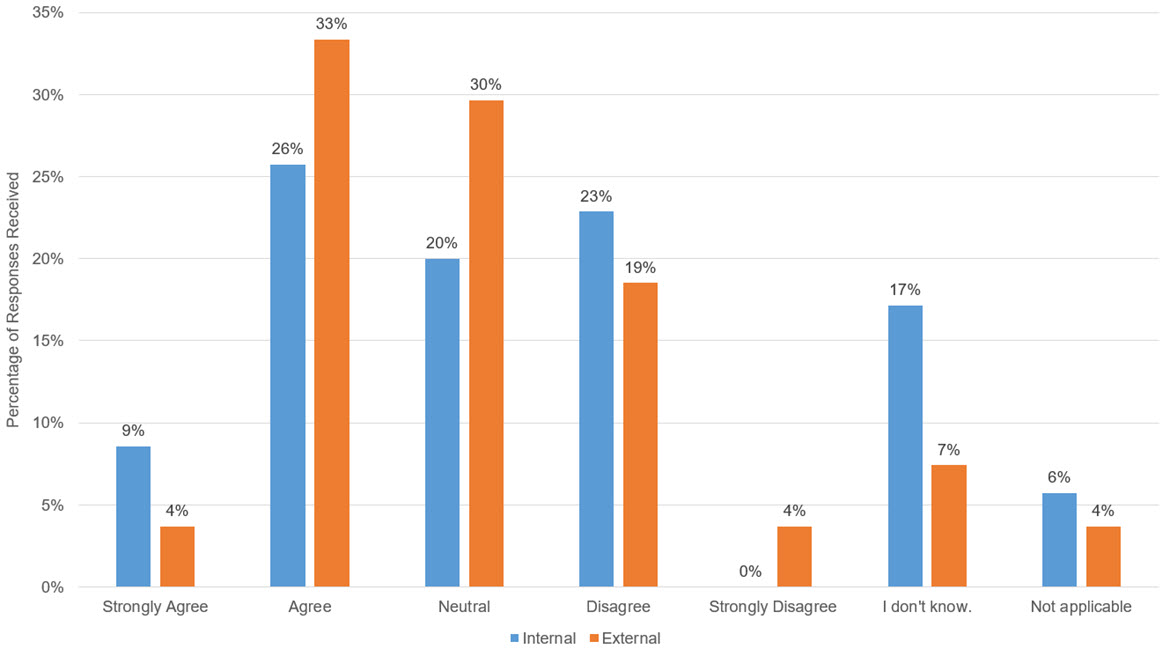
Text alternative for Figure 4 - The Cluster programs allow for services that are safe and free from preventable harm
Figure 4 is a bar chart that illustrates survey results in response to the statement "The Cluster programs allow for services that are safe and free from preventable harm". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (9%), Agree (26%), Neutral (20%), Disagree (23%), Strongly Disagree (0%), I don't know (17%), and Not Applicable (6%). External (to ISC) responses were Strongly Agree (4%), Agree (33%), Neutral (30%), Disagree (19%), Strongly Disagree (4%), I don't know (7%), and Not Applicable (4%).
Source: Survey deployed by ISC Evaluation, 2022.
It was noted that the CPS framework is predominantly relevant to the QIAP, given the program's objective of improving quality of services. As part of the Accreditation program of one accrediting body, organizations are required to complete a Canadian Patient Survey tool used to build the culture of patient safety in their communities. Additionally, it was highlighted that the existing standards involve ensuring clients, patients, and families are involved in the development of the organization's priorities.
In response to a question asking if the Cluster programs could be improved for better patient safety and harm prevention, the majority of both internal (75%) and external (89%) respondents Agreed or Strongly Agreed.
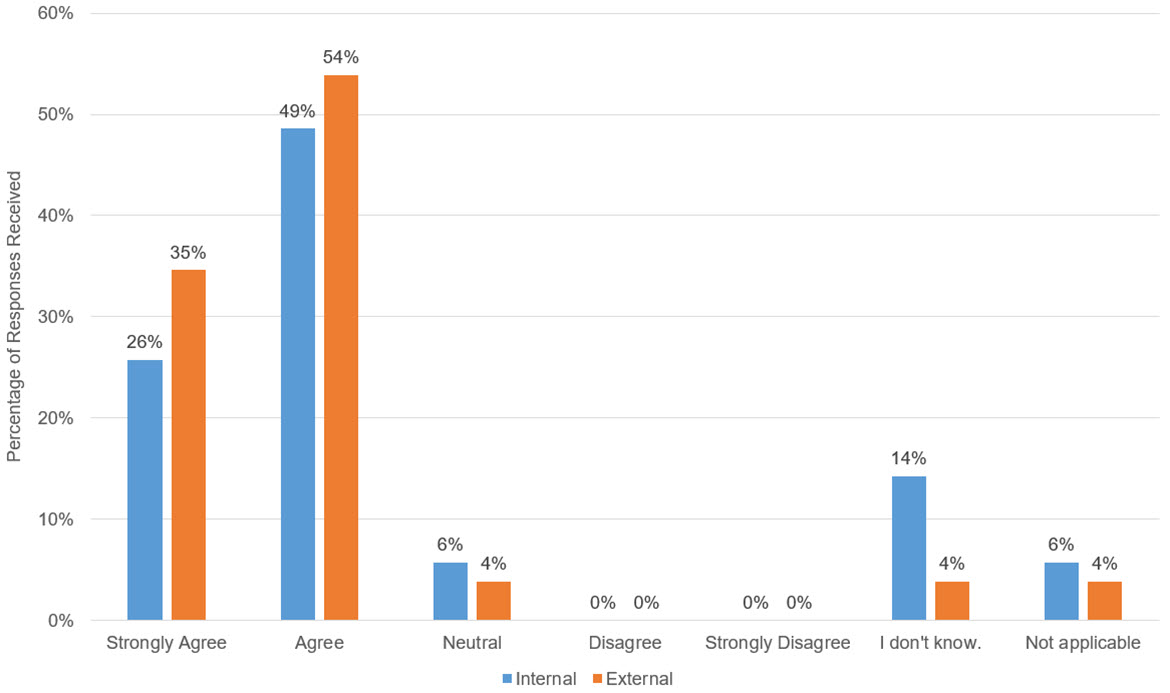
Text alternative for Figure 5 - The Cluster programs could be improved for better patient safety and harm prevention
Figure 5 is a bar chart that illustrates survey results in response to the statement "The Cluster programs could be improved for better patient safety and harm prevention". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (26%), Agree (49%), Neutral (6%), Disagree (0%), Strongly Disagree (0%), I don't know (14%), and Not Applicable (6%). External (to ISC) responses were Strongly Agree (35%), Agree (54%), Neutral (4%), Disagree (0%)3, Strongly Disagree (0%), I don't know (4%), and Not Applicable (4%).
Source: Survey deployed by ISC Evaluation, 2022.
Interviews highlighted a number of gaps in patient safety in existing health services, and the majority of survey respondents strongly agreed (26% of internal respondents and 35% of external respondents) or agreed (49% of internal respondents and 54% of external respondents) indicated that the Cluster could be improved for better patient safety and harm prevention.
While the CPS focuses on safety from a medical perspective, to be truly safe in health care facilities, Indigenous patients require services delivered by people and environments that also promote cultural safety.
Finding #6: The objectives of the Cluster programs are well aligned to the current health needs of First Nations and Inuit communities. However, significant improvements are required to align the design and delivery of the programs to the objectives, including enhanced involvement of First Nations and Inuit in the design and delivery of programming.
Overall, the evaluation found that the objectives and intended outcomes of the programs are well aligned to the needs of First Nations and Inuit communities. However, it is important to note that while the intent of the programs is aligned, there are significant gaps in the delivery of programs that impede progress towards achieving these objectives. These gaps are explored further in the Effectiveness section. While each program within the Cluster was designed to contribute to a shared ultimate outcome, the individual programs outlined specific immediate and intermediate outcomes to be achieved in service of the shared ultimate outcome. This path of outcomes for the Cluster was synthesized into a Logic Model, outlined in Appendix D – Cluster Logic Model. Where First Nations were involved in the design and delivery of their healthcare services, programming was tailored to their communities' needs and delivered culturally safe and traditional methods of care.
Case Study #3
File Hills Qu'Appelle Tribal Council (FHQTC)
Region: Treaty 4 Territory, SK | Program Focus: Health Planning; HSIF
FHQTC co-owns and operates All Nations Healing Hospital, which is the only wholly-owned First Nations hospital in Canada. It serves 15 First Nations, 11 of which are represented by the Tribal Council. The hospital has a busy emergency room, laboratory services, a low-risk birthing unit, acute services clinics, and multiple clinical programs. The hospital also operates clinical services, including Miko-Mahikan Red Wolf (further described in Case Study #1), as well as opioid replacement therapy programming and services related to Hepatitis C and HIV. Services are provided under the premise that if programming and services are meeting the needs of the most vulnerable populations, then they will reach everyone and generate positive outcomes. The services were kickstarted using HSIF funding and is overseen by the Tribal Council which forms the administrative arm of the hospital.
A comparison of each program's objectives to the identified health needs is outlined below. Overall, the integration of First Nations and Inuit in program design would bolster the consideration of Indigenous health needs and promote the integration of cultural health and safety and traditional healing and medicinal practices in health care.
Health Planning and Quality Management
The HPQM program aims to provide guidance to regions who work directly with First Nations and Inuit on creating health and wellness plans. Funding agreements are issued under the program to support the development and ongoing management of Multi-Year Work Plans and of Health and Wellness Plans. The program also supports improving health services and programming by incorporating quality improvement activities in health programs (e.g., accreditation and evaluation of health programs).
A key trend noted in interviews was the need for community-specific needs-based health planning and funding. Indigenous communities desire the autonomy to identify the needs of their community themselves and build programs that address those needs as they see fit. However, they also require the appropriate level of sustainable support to build the capacity to continue to conduct their own health planning in the long-term. Further, the need for improved quality of care, including access to health services in the appropriate facilities, with culturally and medically competent staff and the necessary equipment to provide adequate treatment was emphasized throughout stakeholder groups.
Interviewees noted that the HPQM program was one that related to many of the other Cluster programs, in that appropriate health planning requires consideration of the required health facilities, the technology infrastructure, accreditation processes, as well as the hiring and training of health care staff.
As such, the objectives of the HPQM are well aligned with the current health needs of First Nations and Inuit.
Quality Improvement and Accreditation
The program contributes to advancing the self-determination and capacity for health services in Indigenous communities that meet their needs to improve health outcomes. The program accomplishes this by facilitating the uptake of accreditation and recommending Quality Improvement activities to increase community-based health human resource capacity of First Nations and Inuit to design, manage, evaluate, and deliver health programs and services. The benefit and value of the accreditation program is outlined as improving alignment with provincial health care services, promoting community engagement in patient safety activities, contributing to improved health outcomes, and supporting First Nations and Inuit-led health systems. Recently, enhancements have added emphasis in addressing racism in health care and a focus on cultural safety.
The value of accreditation for Indigenous health facilities was noted repeatedly across interviews with various partners. In particular, interviews emphasized that accreditation was often a point of pride for community health facilities and is considered a building block on which many of the other Cluster programs can leverage to continue to build capacity in communities. Accreditation was described as crucial to ensuring provision of services is aligned to best practices. Specifically, the element of cultural safety being integrated into accreditation processes is highly aligned to the existing needs of Indigenous communities. Given these outlined challenges, the objectives of the QIAP are considered to be aligned to the health needs of the First Nations and Inuit communities.
Health Human Resources
The HHRFootnote 63 program was created to contribute to the strengthening of Indigenous communities' social services, including healthy living and child development, community care, kindergarten to post-secondary education services, familial support, and communicable disease prevention. The objective is to increase the number of First Nations, Inuit, and Métis practicing in healthcare, and to increase the number of qualified individuals working in healthcare delivery in First Nations and Inuit communities. The program is delivered through two streams: scholarships and bursaries for Indigenous students pursuing health careers, and training and certification for community-based workers and health managers to improve the quality and consistency of health care services in First Nations and Inuit communities.
Interviews demonstrated that the intent behind the HHR program is aligned with the needs of the communities, given the notable shortage of community-based workers and appropriate expertise and training, as well as the need for early education in health care professions for Indigenous students.
eHealth Infostructure
The objective of the eHealth program is to provide the "right information to the right people at the right time" to support First Nations and Inuit in being connected, informed, and healthier, and to enable front-line health care workers working in First Nations and Inuit communities to improve Indigenous peoples' health through eHealth programming. The goal of current activities is to increase access to eHealth technologies to enable First Nations, Inuit, and health care providers to use eHealth technologies for the delivery of health care services.
According to interviews, the objectives of the eHealth program are well aligned with the needs identified in interviews, including connectivity, remote access to care, and the provision of integrated services across the health care continuum. Moreover, eHealth is well aligned with the First Nations OCAP® principles by facilitating communities' capacity to effectively collect, distribute, and retain health-related data as they see fit.
Health Facilities Program
The HFP aims to support the development and delivery of health programs and services through investments in health facilities infrastructure. This contributes to First Nations and Inuit in assuming greater control over their own health program and service design, governance, and delivery, including through the planning and management of infrastructure.
The program supports three main categories of activities in relation to health facilities: facilities operations and maintenance (e.g., rent, utilities, cleaning, routine maintenance, minor repairs); minor capital projects (e.g., minor repairs and renovations that cannot be addressed through existing operations and maintenance budgets, less complex projects); and major capital projects (e.g., more complex projects to build new, expand, or significantly renovate/repair health facilities).Footnote 64 However, the program and ISC as a department is not directly involved in the delivery of these First Nation capital activities.
As aforementioned, interview data demonstrated that the lack of accessible, adequate, and safe health facilities is a very prominent need across Indigenous communities. As such, a program such as the HFP dedicated to bridging that gap is aligned to the health needs of First Nations and Inuit.
Health Services Integration Fund
The Health Services Integration Fund (HSIF) supports collaborative planning and multi-year projects aimed at better meeting the healthcare needs of First Nations and Inuit by working with provincial and federal levels of government and creating partnerships to integrate federally and provincially/territorially funded health services in First Nations and Inuit communities; improving access to healthcare for First Nations and Inuit; and increasing the participation of First Nations and Inuit in health programming design, delivery, and program evaluation.
As such, in the HSIF program, particularly in its noted flexibility, is aligned to the identified need for health programming to be driven by community-specific needs, with greater collaboration and control granted to First Nations and Inuit communities.
BC Tripartite Relations Initiative
In 2011, the federal and provincial Ministers of Health and BC First Nations signed the BCT Tripartite Framework Agreement on First Nation Health Governance, which established a new province-wide FNHA to assume control over the design, management, and delivery / funding of federally funded First Nations health programs and services in BC. Since 2013, the FNHA has worked to transform how health care is delivered to First Nations in the province, including closer collaboration and integration with provincial health services.
Interviews with BCT representatives highlighted availability and access to safe and effective care in remote regions, including primary care, mental health and wellness, and culturally safe care as key health needs for the region. A number of interviewees also referred to the recently published In Plain Sight Report that summarized the findings of an Addressing Racism Review that was launched in response to allegations of racist, discriminatory, and inequitable behaviour in BC hospitals.Footnote 65 This report emphasized the need for cultural safety and humility in BC health facilities.
Interviews with key partners demonstrated a clear desire among Indigenous communities to assume control of health services in their communities. As such, the proven transfer of health services under the BCT Agreement is highly indicative of strong alignment between the program and the needs of communities.
Cluster of Health Infrastructure Support
It is important to note that while the assessment of the aggregate data indicates that the Cluster programs' objectives are each aligned with the health needs of people in First Nations and Inuit communities, the level of need in each of the areas varies in specific regions or communities. This is noteworthy as there could be needs in communities that are higher priority that are not being met by these programs, while funding is only being allocated to these specific areas.
One key trend noted amongst interviews was the emphasis placed on the unique needs of various communities and how this must be adequately considered in order to ensure true program alignment. For example, there are some communities who may struggle more in training community-based workers and therefore value HHR, while another community may have no issues with training and instead require more funding to put towards mental health and wellness programs for at-risk youth. This type of scenario was used in interviews to highlight the potential pitfalls associated with designing programs with such specific parameters and objectives, as opposed to more widely applicable health transformation funding that communities could allocate to core needs as they are identified.
Extent to Which Cluster Programs are Appropriate Mix to Achieve Service Transfer
This evaluation also assessed the programs through the lens of understanding whether the combination of these targeted initiatives (Cluster programs) make up the appropriate mix to achieve service transfer. In discussions with key program partners, there were varying perceptions shared.
While a number of partners perceived the programs as aligned in objectives and identified opportunities to increase collaboration, a select number of program partners identified their perceived misalignment, particularly, that any existing alignment is not being highlighted at the national level and instead only if regions take the initiative to link them. However, many of these same partners noted that there are certain programs (e.g., Accreditation, Health Planning) that connect many similar elements.
Ultimately, partners emphasized that true alignment to needs requires the basis of a shared objective of improved capacity and self-determination. For programs such as Accreditation, interviewees highlighted that it creates a foundation that facilitates capacity building in the other program target areas, such as eHealth and HHR.
The level of continued demand for funding under all programs evaluated indicate a high degree of relevance to the existing needs. However, the continued challenges faced by people in First Nations and Inuit communities despite receiving some funding through these programs highlights a gap in effectiveness. These challenges are detailed further in the following sections of this report.
3.2 Effectiveness
Given the Cluster programs have been operational for several years, this evaluation sought to assess the level of effectiveness of the programs in achieving their respective outcomes and objectives since fiscal year 2015-2016 and highlight areas of proven success and areas for potential improvement moving forward.
Evaluation Question: What aspects of the programs are working well and what aspects need improvement?
Finding #7: While progress towards program objectives was made over the evaluation period, the effectiveness of Cluster program delivery and administrative processes was significantly impeded by limited funding, staffing shortages, and a misaligned performance measurement framework.
In order to assess the effectiveness of the Cluster programs to date, this evaluation collected data through a number of consultations with internal and external partners, as well as reviewing internal program data in order to conclude on the extent to which these programs have progressed towards achieving their defined objectives.
Program Delivery and Administrative Processes
In interviews, Implementing Partners and Program Leads were asked to rate their perception of the effectiveness of program delivery for the programs they were involved with on a scale of one to five (Very Ineffective - Very Effective).

Text alternative for Figure 6 - Perception of Partners on Overall Effectiveness of Program Delivery
Figure 6 is a pie chart that illustrates the responses of Implementing Partners who participated in interviews on the overall effectiveness of the delivery of program(s) they interact with under this Cluster. Responses were on a scale and included Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. Responses were Very Effective (20%), Effective (60%), Neutral (20%), Ineffective (0%), and Very Ineffective (0%).
Source: Interviews by ISC Evaluation, 2022-2023.
Generally, Implementing Partners and Program Leads found the delivery of Cluster programs to be effective, with all respondents describing delivery as either Neutral (20%), Effective (60%) or Very Effective (20%). However, it should be noted that this data encompasses Implementing Partners' experiences with any number of the six programs being evaluated, and as such, could include varying perspectives depending on the program. In order to ensure the key strengths and areas of potential improvements were adequately captured, a further qualitative assessment of the effectiveness of each individual program's delivery in consideration of their unique context is outlined in Findings #8 - #13. To provide additional contextual information, this Finding seeks to illustrate the common areas of strength as well as areas of improvement that were noted regarding the effectiveness of program delivery across all Cluster programs.
Working Well
As indicated in the above graph, Program Leads and Implementing Partners generally perceive that the delivery of Cluster programs is effective, with 29% of internal partners selecting Neutral, 43% selecting Effective and 29% selecting Very Effective. 100% of external partners selected Effective. Commentary about aspects that were working well included the following:
- Cluster programs have been effective in progressing towards their intended outcomes and objectives, despite challenges such as limited funding or human resources.
- The flexibility and efficient administration of the additional funding provided during COVID-19 was highlighted as a key success. Timely access to data and information about First Nations and the impact the pandemic had on First Nations also allowed the department to better allocate resources and make decisions more quickly.
- Efforts have been made to reduce the reporting burden on recipients. For example, HSIF has updated their progress report template in recent years by simplifying the amount and type of information required to ensure only the most crucial elements remain, while also providing open text space for recipients to include additional information about their projects as they see fit.
Needs Improvement
In interviews, certain partners shared their perception of key program elements, such as administrative processes, performance measurement, and communications. Of those who were asked, between 20%-30% of partners noted that the following aspects needed improvement:
- While there have been efforts made to reduce administrative burden on First Nations, it was noted that there are still opportunities to streamline some administrative processes, especially for First Nations who may access various streams of funding from ISC and may therefore be required to complete a significant amount of progress reporting.
- Performance measurement and reporting requirements are often misaligned to operational outcomes and First Nations and Inuit ways of knowing, creating barriers to collecting accurate and meaningful data and presents an incomplete reflection of progress.
- Roles and responsibilities between various partners (e.g., ISC Headquarters (HQ) and Regions, Regions and First Nations) are often ambiguous, creating confusion around expectations and priorities.
- A localized approach to prioritizing needs is necessary in order to adapt to the unique needs of varying regions.
Case Study #4
First Nations of Québec and Labrador Health and Social Services Commission/Commission de la santé et des services sociaux des Premières Nations du Québec et du Labrador
Region: Québec and Labrador | Program Focus: Health Planning; HSIFCase Study #4 note 1; eHealth
The Commission currently measures the success of their programming and services by observing community involvement with initiatives; effective communication with stakeholders; implementing and maintaining effective infrastructure for communities and community members; providing technology-related advice to communities and community members; and having technology and training for optimal use of this technology available for communities and community members. This performance measurement framework allows the Commission to track, monitor, and report on what is important to its members, which in turn promotes feelings of successful programming and desire to continually invest.
Throughout both internal and external interviews, over 74% explicitly noted insufficient funding and almost 60% explicitly noted a lack of capacity as barriers to the achievement of the Cluster programs' ultimate objectives. The specific ways in which these barriers impact the program delivery of each program is noted in the following pages.
These areas of improvement are detailed further below and in other sections of this report in Findings #16, 17, 21, and 22.
Performance Measurement & Reporting
In order to assess effectiveness, the evaluation required access to program data, tracked through performance measurement frameworks and results reporting. This proved to be more challenging than anticipated, due to limitations in data collection from programs. An assessment of the effectiveness of the Cluster programs' respective performance measurement frameworks and resulting reporting highlighted significant barriers to assessing progress. As such, the following sections of the report are based on limited quantitative program data.
The Cluster programs have individual performance measurement frameworks that are designed to measure program progress towards immediate, intermediate, and ultimate outcomes. Each program has a PIP, where specific performance indicators are meant to be outlined with targets, baseline data points, as well as descriptions of rationale, measurement strategy and data sources. While each PIP outlines a number of program-specific indicators, the programs may only be required to publicly report on one unique indicator in ISC's annual Departmental Results Reports.
Those indicators, for each program in scope, that are required to be reported are outlined below:
| Program | Performance Indicator Reported to Treasury BoardFootnote 66 |
|---|---|
| HPQM | Percentage of nursing stations that are accredited or in the process of being accredited |
| QIAP | |
| HSIF | |
| HFP | Percentage of First Nation health facilities with a condition rating of good |
| HHR | Percentage of Indigenous people working in the health sector in Canada |
| eHealth | Number of Digital Health Record systems (e.g., electronic medical record, electronic health record, community electronic medical record, other) in communities |
Each program had different approaches to collecting and reporting results from Implementing Partners and program recipients; however, the program files received demonstrated significant gaps in reporting against program indicators.
Review of internal documentation demonstrated that HSIF and eHealth each have annual project report templates that are provided to recipients, detailing the expected contents to be included.Footnote 67 For QIAP and HHR, annual reports are developed by the programs' respective Implementing Partners (i.e., Accreditation Canada, Canadian Accreditation Council, and Indspire) which outline progress in that fiscal year. However, in all documentation received, there was notable inconsistencies in either the nature of the data being collected/reported or the availability of these figures on an annual basis. This created barriers in evaluating program performance against outlined program objectives. Furthermore, the review of program data received indicated a significant gap in data collected over the evaluation period across the Cluster programs. In many cases, data reported varied between fiscal years or recipient reports, or was simply not provided in its entirety.
Performance measurement was noted in interviews as an area to improve by over 40% of Program Leads, 29% of Regional Staff, and 33% of Regional Executives. According to interviews, the reporting requirements can be difficult to meet due to a misalignment between government expectations and the nature of community reporting, the latter of which is often more based in cultural values, community needs, and storytelling rather than outcome reports. This variance was noted to cause challenges for programs to illustrate the outcomes of the program in a format that the federal government expects. As such, the effort required to align community reporting to these standards was said to be burdensome to First Nations.
Interviewees noted that overall program delivery would benefit from engaging with First Nations and Inuit who may be experiencing challenges with reporting requirements and develop a more relational approach to improve the process rather than expect First Nations and Inuit to follow existing, often bureaucratic processes that can lead to inaccuracies and inefficiencies.
Historically, reporting was completed through a reporting template that captured output-based data. However, in discussions with internal partners, it was noted that there are efforts to shift away from output measuring due to the challenges presented for infrastructure programs, such as HFP, which operate primarily as a facilitator of health projects or initiatives rather than service providers seeking to achieve a set of outcomes. Further, it was noted that while performance measurement frameworks are in place, they are rarely leveraged as the identified performance indicators are not reported against consistently. Internal program partners highlighted that the indicators in place are often outdated or misaligned to the current intended outcomes of the programs and that many programs described performance measurement as challenging, due to notable data gaps (e.g., baseline data against which to measure progress), lack of First Nations and Inuit input in metrics, and a lack of capacity to apply the frameworks in a consistent manner.
It was also noted in a select number of interviews that expectations around reporting can be particularly difficult to manage as to not infringe on First Nations and Inuit data sovereignty and OCAP® principles. As a result, gathering data and aggregating information to report on program progress has been a challenge for a number of regions.
Internal interviews highlighted that as services continue to be transferred, more performance measuring and reporting activities will fall to those in First Nations and Inuit communities rather than regions, rendering existing frameworks redundant. This further supports the identified need to further integrate First Nations and Inuit input and direction in the development of relevant indicators in consideration of current and future operating landscapes. The evaluation also noted that there are efforts underway, both internally within the Department and externally with partners such as the FNHMA, to mitigate the potential reporting burden.
Evaluation Question: To what extent has each of the programs included made progress toward the achievement of their respective expected outcomes?
In the Relevance section, an analysis was conducted to conclude on the alignment of the program objectives to the identified current health needs of First Nations and Inuit. In this section, this analysis extends further to assess the effectiveness of each program in achieving these outcomes in delivery.
While the immediate, intermediate, and ultimate outcomes were synthesized in the Cluster Logic Model (Appendix D – Cluster Logic Model), each program has specific outcomes defined in their respective program profiles. The progress of each program towards these outcomes, as well as the strengths that facilitated progress and barriers that impeded progress, are described in the following pages.
Finding #8: The HPQM program has made progress in supporting First Nations and Inuit in the development and management of health plans, with over 289 plans in place in Fiscal Year 2020/21, an increase of 22% since Fiscal Year 2015/16.
| Immediate | First Nations and Inuit plan and manage health programs and services. |
|---|---|
| Intermediate | Improved access to quality health services for First Nations and Inuit. |
| Ultimate | First Nations and Inuit design, deliver and manage their health programs and services; communities are healthier; Indigenous people have reliable and sustainable infrastructure. |
The primary immediate outcome outlined for the HPQM program is that "First Nations and Inuit plan and manage health programs and services." With consideration of this outcome, this evaluation sought to assess the effectiveness of the program by analyzing the extent to which First Nations and Inuit can now manage and operate health programs and services. This is primarily measured by the program by tracking the number of First Nations and Inuit communities that are supported through HPQM funding to develop a Community Health Plan.
A review of program data highlighted that the HPQM program has funded the development and management of an increasing number of community health plans annually, from 236 in Fiscal Year 2015/16 to 289 Fiscal Year 2020/21.Footnote 68

Text alternative for Figure 7 - First Nation and Inuit Supported by ISC to Develop a Community Health Plan
Figure 7 is a bar graph that illustrates internal ISC program data on the number of First Nations and Inuit who have been supported by ISC to develop a Community Health Plan, by year, and percentage increase, from fiscal years 2015-16 through 2020-21. In 2015-16 ISC supported First Nations and Inuit in the development of 84 Health and Wellness Plans and 152 Multi-Year Work Plans, for a total of 236 plans. In 2016-17 ISC supported First Nations and Inuit in the development of 87 Health and Wellness Plans and 162 Multi-Year Work Plans, for a total of 249 plans and a 6% year-over year increase. In 2017-18 ISC supported First Nations and Inuit in the development of 88 Health and Wellness Plans and 177 Multi-Year Work Plans, for a total of 265 plans and a 6% year-over year increase. In 2018-19 ISC supported First Nations and Inuit in the development of 90 Health and Wellness Plans and 193 Multi-Year Work Plans, for a total of 285 plans and a 7% year-over year increase. In 2019-20 ISC supported First Nations and Inuit in the development of 85 Health and Wellness Plans and 219 Multi-Year Work Plans, for a total of 304 plans and a 7% year-over year increase. In 2020-21 ISC supported First Nations and Inuit in the development of 53 Health and Wellness Plans and 236 Multi-Year Work Plans, for a total of 289 plans and a 5% year-over year decrease.
Source: HPQM Program Data, retrieved 2022.
It should be noted that Health and Wellness plans are funded through block agreements, and Multi-Year Work plans are funded through flex agreements. In 2020-21, recipients transitioned to the New Fiscal Relationship (NFR) GrantFootnote 69, and away from the block funding agreements demonstrated above, resulting in the noted decrease of community plans being supported in that fiscal year.
Further, it was also noted that people in First Nations and Inuit communities experienced challenges in meeting deadlines for plan development and submissions due to the COVID-19 pandemic which impacted the results for 2019-20 and 2020-21.
External researchFootnote 70 noted that as of Fall 2019 ISC has supported 161 First Nations to complete community-led plans, and 204 First Nations and 1 Inuit community are in the process of creating or updating community plans.
In surveys, both First Nations Representatives and Implementing Partners were asked whether they perceived access to wholistic health services to have increased since 2015 in relation to the HPQM program. In response, the majority of respondents indicated that they either Agreed (50%) or Strongly Agreed (7%), while over a fifth Disagreed (22%) or Strongly Disagreed (7%).
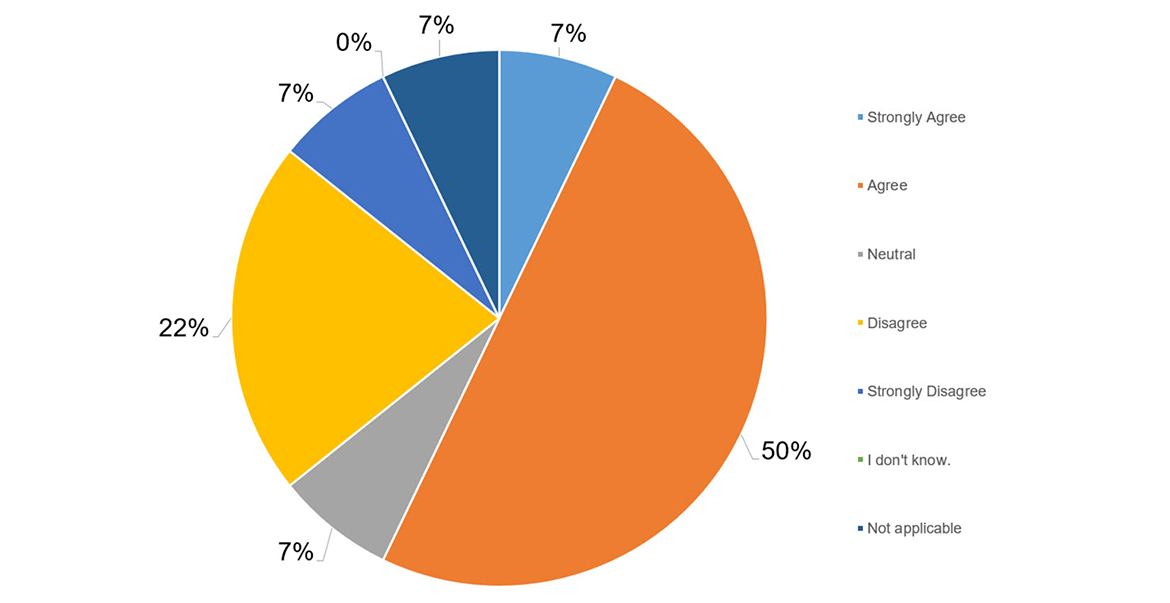
Text alternative for Figure 8 - Access to wholistic health services has increased between 2015-2020
Figure 8 is a pie chart that illustrates survey responses to the statement "Access to wholistic health services has increased between 2015-2020 (HPQM)". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses were Strongly Agree (7%), Agree (50%), Neutral (7%), Disagree (22%), Strongly Disagree (7%), I don't know (0%), and Not Applicable (7%).
Source: Survey deployed by ISC Evaluation, 2022.
Further, both First Nations Representatives and Implementing Partners were asked if they perceived the quality of care being provided as excellent as a result of the HPQM program. Responses were more varied for this question, with a slightly higher number of partners indicating that they Agree (36%) than Disagree (29%) and a significant number indicating neutrality (21%).
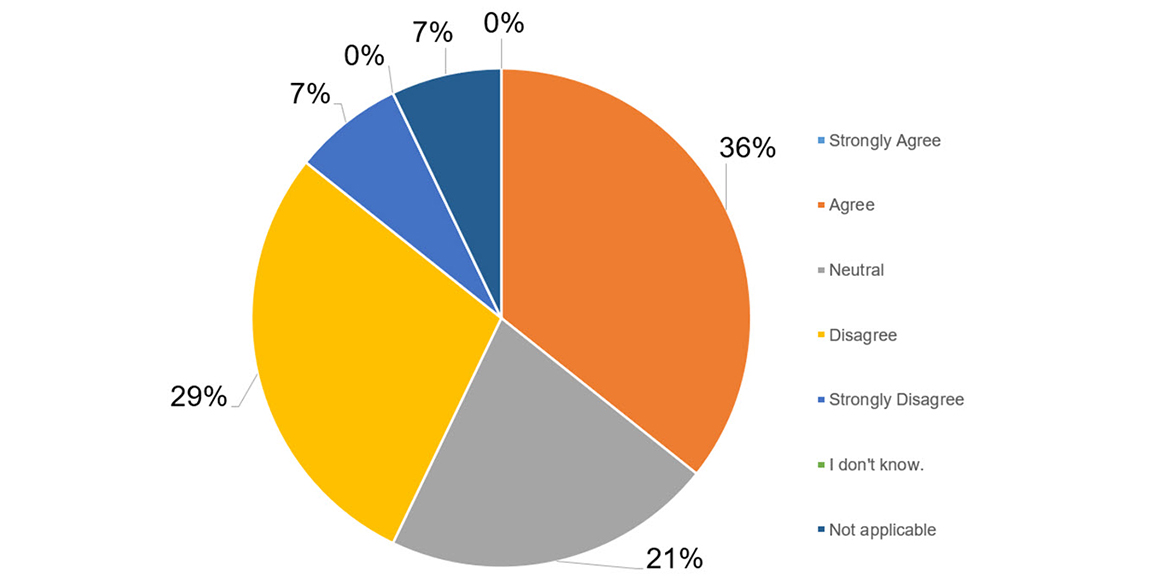
Text alternative for Figure 9 - The quality of care provided is excellent because of HPQM
Figure 9 is a pie chart that illustrates survey responses to the statement "The quality of care provided is excellent because of HPQM". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses were Strongly Agree (7%), Agree (50%), Neutral (7%), Disagree (22%), Strongly Disagree (7%), I don't know (0%), and Not Applicable (7%).
Source: Survey deployed by ISC Evaluation, 2022.
Internal partners involved with the HPQM program highlighted strides made in transitioning First Nations and Inuit from set or fixedFootnote 71 funding arrangements to flexibleFootnote 72 or blockFootnote 73 funding arrangements.
According to interviews, where First Nations and Inuit previously required consultants to support their health planning activities at the onset of the HPQM program, they have now begun taking ownership of their own health planning, utilizing developed health plans, and getting more involved in the process. It was noted that the pandemic resulted in delays in the development and submission of health plans which has amassed the need for more support for First Nations and Inuit to progress past these obstacles. However, it was also highlighted that the health directors in communities that worked with HPQM were key to the pandemic response in providing leadership and expertise, as a result of the capacity the program helped build within their organizations and communities.
Finding #9: With over 280 projects completed or ongoing, HSIF has provided value to First Nations and Inuit and has advanced towards the outcome of improving access to quality care and increasing the level of integration of health services and systems.
| Immediate | Increased capacity of partners to collaborate on health service integration initiatives. |
|---|---|
| Intermediate | Improved access to quality health services for First Nations and Inuit. |
| Ultimate | First Nations and Inuit design, deliver and manage their health programs and services; communities are healthier; Indigenous people have reliable and sustainable infrastructure. |
The objective of the HSIF is to support collaboration between provincial and federal governments and First Nations and Inuit to improve the level of involvement of First Nations and Inuit in the design, delivery, and evaluation of health programming. The evaluation sought to assess the extent to which there has been an increase of integration of health services systems across federal, provincial, territorial, municipal and community levels.
HSIF provides funding on a multi-year project basis. According to interviews, these projects were historically focused on health systems transformationFootnote 74, and now with the creation of the broader Health TransformationFootnote 75 initiative, HSIF projects are leveraged to lead First Nations and Inuit to full service transfer. According to the HPQM&SI PIP, the HSIF program's performance is measured against the following indicators:
- Number of partnerships that develop from projects;
- Percentage of First Nations and Inuit partnerships within HSIF projects with an assessment of 'proceeding as planned' or 'proceeding better than expected';
- Number of and type of integration knowledge products developed;
- Number and type of newly integrated First Nations and/or Inuit health institutions, programs, activities, standards, practices or regulations; and,
- Number of new Memoranda of Understanding (MOU), protocols, agreements, frameworks or arrangements which further integrate First Nations and/or Inuit health services.
These indicators were inconsistently reported on throughout the evaluation period, and as such, this evaluation was unable to measure progress against all outlined indicators. However, certain data points were tracked and a project sample was reviewed in order to understand the status of current projects, regional distribution and primary focus areas of funded projects in alignment with intended outcomes. Additionally, this data was supplemented by stakeholder interviews and survey data, where perceptions of progress were shared. Through these consultations, partners emphasized progress made towards supporting health services integration and transformation across Canada.
A review of program data demonstrated the achievement of approximately 280 projects, 204 of which are completed.Footnote 76

Text alternative for Figure 10 - HSIF Projects as of 2022 By Region
Figure 10 is a bar chart that represents HSIF program data that documents the number of complete, active/new, incomplete/cancelled, upcoming, and total projects in 2022, separated by region. In the Atlantic region, there were 53 completed projects, 10 active/new projects, 1 incomplete/cancelled project, 0 upcoming projects for a total of 64 projects. In the Saskatchewan region, there were 15 completed projects, 10 active/new projects, 0 incomplete/cancelled project, and 0 upcoming projects for a total of 25 projects. In the Quebec region, there were 7 completed projects, 15 active/new projects, 0 incomplete/cancelled project, and 1 upcoming project for a total of 23 projects. In the Manitoba region, there were 30 completed projects, 6 active/new projects, 1 incomplete/cancelled project, and 0 upcoming project for a total of 37 projects. In the Alberta region, there were 58 completed projects, 18 active/new projects, 0 incomplete/cancelled project, and 0 upcoming project for a total of 76 projects. In the Alberta region, there were 58 completed projects, 18 active/new projects, 0 incomplete/cancelled project, and 0 upcoming project for a total of 76 projects. In the Northern Region, there were 26 completed projects, 9 active/new projects, 0 incomplete/cancelled project, and 0 upcoming project for a total of 35 projects. In the Ontario Region, there were 15 completed projects, 8 active/new projects, 0 incomplete/cancelled project, and 0 upcoming project for a total of 23 projects.
Source: HISF Program Data, retrieved 2022.
When broken down further by region, the program data indicates that a significant proportion of HSIF projects are pursued in Alberta (AB) and Atlantic (ATL) regions, with progress also notable in Manitoba (MB) and the Northern (NR) region. Further, progress towards increasing integration is demonstrated through the sample of HSIF projects assessed, noting a higher proportion of projects aiming to increase integration of government-funded health services for First Nations and Inuit (FN/I) interests into provincial/territorial (P/T) health planning and delivery.Footnote 77
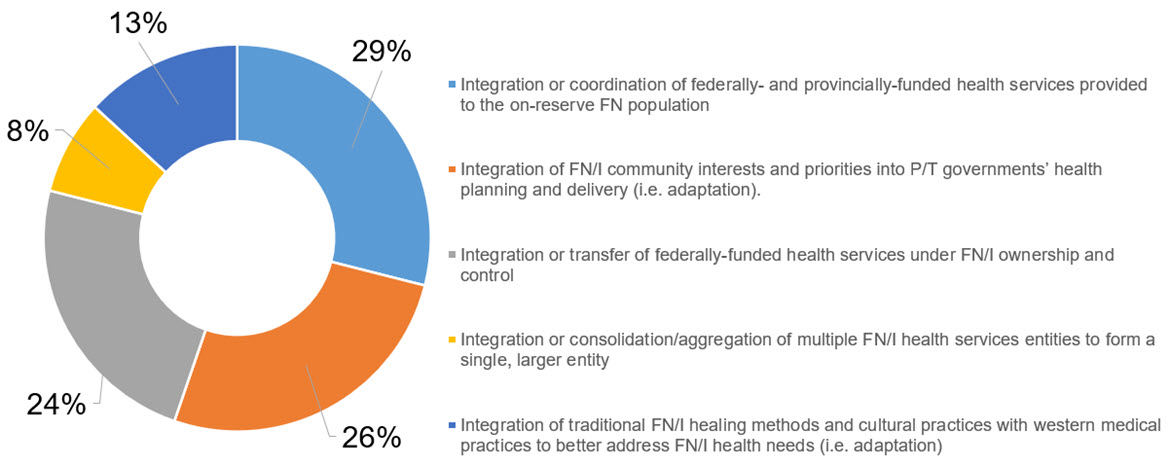
Text alternative for Figure 11 - Sample of HSIF Projects, Types of Integration Covered by Projects Reported
Figure 11 is a pie chart illustrating the types of Integration Projects that had been included in projects reported to and funded by HSIF. 29% of projects involved the integration or coordination of federally- and provincially-funded health services provided to the on-reserve First Nations population; 26% of projects involved integration of First Nations or Inuit community interests and priorities into Provincial/Territorial governments' health planning and delivery (i.e., adaptation); 24% of projects involved the integration or transfer of federally-funded health services under First Nations or Inuit ownership and control; 8% of projects involved the integration or consolidation/aggregation of multiple First Nations or Inuit health services entities into one single, larger entity; and 13% of projects involved the integration of traditional First Nations or Inuit healing methods and cultural practices with western medical practices to better address First Nations or Inuit health needs (i.e., adaptation).
Source: HISF Program Data, retrieved 2022.
The sample of HSIF projects across ON, AB, and SK reviewed, as shown in Figure 11, demonstrate that progress has been made across a variety of areas aligned to the identified key health needs of First Nations and Inuit, including mental health and addiction, eHealth, health planning and traditional and cultural health.Footnote 78

Text alternative for Figure 12 - HSIF Sample of Projects Focus Areas
Figure 12 is a bar chart that represents program data of a sample of projects funded by HSIF and the project areas that they most closely align with. The focus areas include Mental Health & Addiction (10); Chronic Disease Management (8); Public Health (8); Primary Health Care (8); Health Planning (8); Integrated Governance (8); Health Promotion (5); Health Human Resources (5); Data Management (4); Elder Care (4); Children and Youth (4); Delivery of Training (1); Maternal Care (3) Continuing Care (3); eHealth (3); Cancer Care & Screening (2); Suicide Prevention (2); Traditional and Cultural Health (1); Non-Insured Health Benefits (1); Treaty-Based Health Funding Agreement (1); and Collaborative Partnership (1).
Source: HISF Program Data, retrieved 2022.
Overall, interviews were predominantly positive in their perceptions of the program's effectiveness thus far. Specifically, many interviewees noted the value of the flexibility of the fund, enabling First Nations to adapt programming to meet their unique needs. However, some program partners (13%) highlighted several challenges stemming from the lack of sustainability of progress. For example, it was noted that any MOUs or protocols developed are based on the leaders in government at the time and are often not codified, and as such they are subject to change when the leaders shift.
Further, it was noted that managing expectations and perceptions among the layers of government from the federal level down to the community levels can be challenging and political. This, according to interviews, results in barriers to policy decision-making and collaboration amongst these partners and often causes a subsequent lack of action. Interviewees emphasized that needs should come from the community up, rather than top down from Provincial/Territorial governments, as it should be First Nations and Inuit who direct what health integration should look like.
Interviews highlighted a potential barrier to achieving objectives, including the limited reach to people in First Nations and Inuit communities as a result of the proposal-based approach to providing funding to projects, given that health service personnel in First Nations and Inuit communities may not be aware of the funding opportunities or have adequate resources to dedicate towards developing proposals on an annual basis.
In consideration of the ultimate outcomes of the HSIF program and the Cluster as a whole, surveys were leveraged to gather internal and external partners' perceptions of an increase in access to health services within the evaluation scope timeline and whether they credit HSIF for provision of excellent quality care.
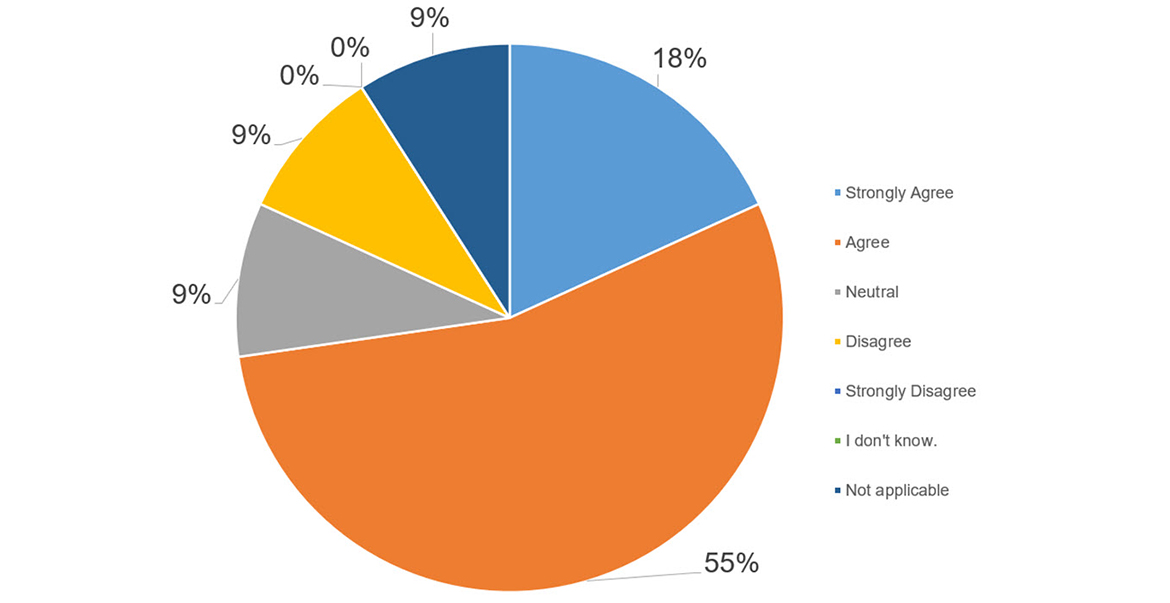
Text alternative for Figure 13 - Access to wholistic health services has increased between 2015-2020
Figure 13 is a pie chart that illustrates survey responses to the statement "Access to wholistic health services has increased between 2015 - 2020 (HSIF)". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses were Strongly Agree (18%), Agree (55%), Neutral (9%), Disagree (9%), Strongly Disagree (0%), I don't know (0%), and Not Applicable (9%).
Source: Survey deployed by ISC Evaluation, 2022.
In response to the former, the majority of partners found that access to wholistic services have increased since 2015, with 55% respondents indicating that they Agree, and 18% stating that the Strongly Agree. In response to the latter question, results were more varied, with half of partners indicating they Agree (33%) or Strongly Agree (17%), and the remaining half mostly Neutral (25%) or indicating that this is not applicable (17%).
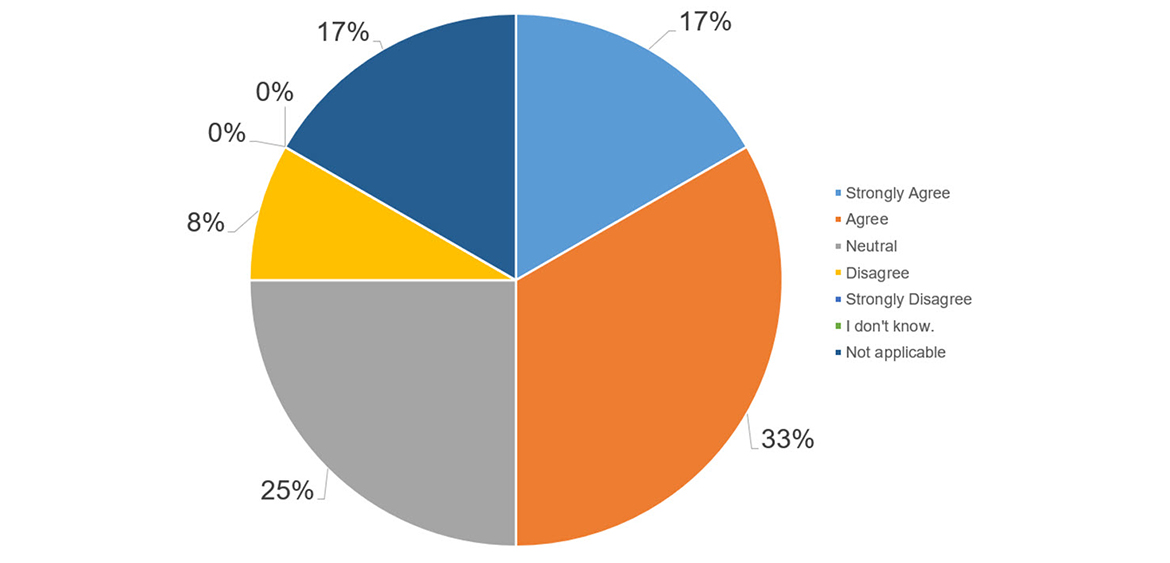
Text alternative for Figure 14 - The quality of care is excellent because of HSIF
Figure 14 is a pie chart that illustrates survey responses to the statement "The quality of care is excellent because of HSIF)". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses were Strongly Agree (17%), Agree (33%), Neutral (25%), Disagree (8%), Strongly Disagree (17%), I don't know (0%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
Further, partners were asked to indicate whether they perceived there to be a high level of satisfaction of services delivered through HSIF. Results were primarily positive, with the majority of respondents indicating that they Agree (50%) or Strongly Agree (9%), and the rest indicating neutrality (25%) or a lack of relevance or knowledge (8%).
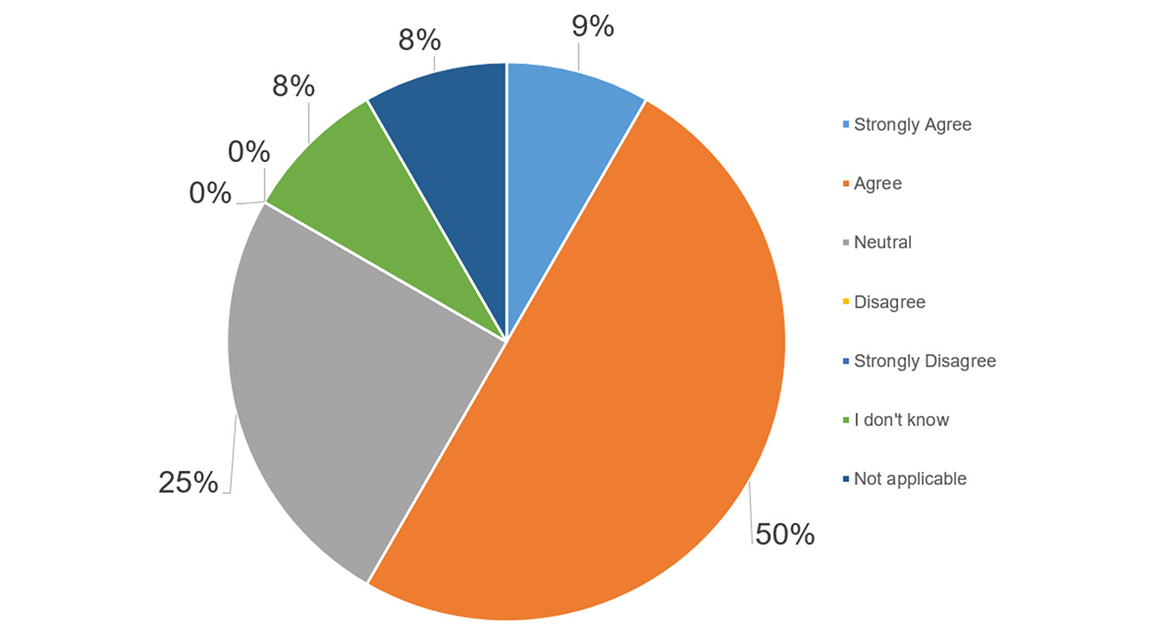
Text alternative for Figure 15 - There is a high level of satisfaction of services delivered through HSIF
Figure 15 is a pie chart that illustrates survey responses to the statement "There is a high level of satisfaction of services delivered through HSIF". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses were Strongly Agree (9%), Agree (50%), Neutral (25%), Disagree (0%), Strongly Disagree (0%), I don't know (8%), and Not Applicable (8%).
Source: Survey deployed by ISC Evaluation, 2022.
Program data, key informant interviews, and survey results indicate that HSIF has provided value to First Nations and Inuit and has advanced towards the outcome of improving access to quality care. However, there are key barriers in place that prevent the program from reaching its full potential.
Finding #10: The QIAP has supported the accreditation of 34% of First Nations health centres, 10% of First Nations nursing stations, and 91% of First Nations treatment centers nationally as of 2021. Demand for the program has surpassed funding capacity since funding stalled in 2017/18.
| Immediate | Health programs and services are accredited. |
|---|---|
| Intermediate | Improved access to quality health services for First Nations and Inuit. |
| Ultimate | First Nations and Inuit design, deliver and manage their health programs and services; communities are healthier; Indigenous people have reliable and sustainable infrastructure. |
In consideration of the QIAP objective of advancing the accreditation of health programs and services through the provision of funding, this evaluation assessed the progress of the program towards its outlined objectives. Accreditation is an ongoing quality improvement process that focuses on community, client and staff safety and supports the streamlining of health standards. Health centres can leverage a collaborative approach to develop a road map outlining what is working well and where there is room for improvement, including innovative ways of achieving service excellence.Footnote 79
While managed by ISC's First Nations and Inuit Health Branch (FNIHB), the QIAP is delivered in partnership with national accrediting bodies, including Accreditation Canada and the Canadian Accreditation Council. As such, program data is collected through annual reports developed by these partners, as well as internal data and external sources, such as the Regional Health Survey.
According to the HPQM&SI PIP, the QIAP's performance is measured against the following indicators:
- Percentage of nursing stations and health centers that are accredited or in the process of being accredited;
- Percentage of accredited health programs and services that met 90% or more of the safety standards of the accreditation body; and
- Percentage of First Nations adults in communities with accredited health programs and services who rate the quality of health services in their community as either 'excellent' or 'good'.
As aforementioned, data collection in accordance with PIPs was predominantly found to be inconsistent between 2015 and 2021. However, according to the ISC Departmental Results Report, the QIAP, formally reported under the HPQM&SI umbrella program, has consistently met its target of 10% of First Nations and Inuit nursing stations being accredited or in the process of accreditation since 2019-2020.Footnote 80
Furthermore, the program data reviewed highlighted progress achieved in the number of First Nations and Inuit health facilities and organizations that are accredited or in the process of achieving accreditation. This data is presented in Table 6, broken down by region.Footnote 81
| As of 2021 | FN Health Centres | FN Nursing Stations | FN Treatment Centres | |||
|---|---|---|---|---|---|---|
| Number Accredited |
Number of Organizations |
Number Accredited |
Number of Organizations |
Number Accredited |
Number of Organizations |
|
| BC | 33 | 163 | 0 | 10 | 9 | 9 |
| AB | 12 | 45 | 3 | 5 | 7 | 7 |
| MB | 33 | 42 | 2 | 22 | 5 | 5 |
| SK | 44 | 69 | 2 | 12 | 8 | 9 |
| ON | 15 | 105 | 0 | 29 | 11 | 11 |
| QC | 12 | 16 | 2 | 11 | 5 | 6 |
| ATL | 8 | 34 | blank | blank | 5 | 6 |
| Total | 159 | 474 | 9 | 89 | 49 | 54 |
| 34% | 10% | 91% | ||||
The value of accreditation was noted repeatedly throughout interviews with both internal and external partners. Participation in the program was said to be a point of pride for organizations; those who are accredited were seen as leaders within the community.
A review of literature also demonstrated the impact of Accreditation on the ability of First Nations and Inuit to manage health services. For example, a published interview with an advanced practice nurse at Esk'etemc Health Department noted that Accreditation Canada's Primer process allowed the Esk'etemc Health Department to evaluate its health care services on a systemic level, as exposure to Accreditation Canada standards enabled the department to perceive how the Nation's health care services compared to other First Nations and non-First Nations health providers. It was stated that "there was a real focus on the improvement of quality and safety as a process."Footnote 82
A survey conducted by ISC Regional Accreditation Managers/Leads as well as representatives from FNHA conducted a survey in 2020 to assess if accreditation had strengthened organizations' response to COVID-19. 89% of survey respondents indicated notable improvements in their ability to respond effectively to the pandemic.Footnote 83
Although the value of the QIAP was well understood and highlighted during key informant interviews, partners noted that demand for the program has surpassed the program's capacity due to severely limited funding.
According to internal program documentation, Accreditation's requested amount for funding was not renewed in 2017/18, leading to a funding deficit of $2.1 million as of 2021/22.Footnote 84 A review of program data indicated that as of September 2021, over 24 additional organizationsFootnote 85 were on the waitlist for accreditation. As such, despite this notable level of success and rising interest from First Nations and Inuit, partners emphasized the limitations created as a result of insufficient funding and support from ISC.
This significantly impacts the potential of success of the program, as funding is critical to support the growth of the program as well as the maintenance of the accreditation itself. First Nations Representatives emphasized that considerable resources, both human and financial, are necessary to maintain accreditation requirements, resulting in additional challenges in the sustainability of remaining accredited.
Internal partners voiced their frustration in the lack of Departmental recognition of the value of the Accreditation program and the impact it has on building capacity in First Nations and Inuit to take ownership of their services.
Finding #11: The eHealth program has increased the number of telehealth sessions delivered by 15% (from 15,682 to 18,106) since 2016-2017. Reduced funding has created a barrier to improving connectivity and access to digital health record systems.
The effectiveness of the eHealth infostructure program was assessed in this evaluation in consideration of the outlined objectives of the program to increase access to eHealth technologies.
| Immediate | First Nations and health care providers have access to eHealth technologies. |
|---|---|
| Intermediate | Improved access to quality health services for First Nations. |
| Ultimate | First Nations and Inuit design, deliver and manage their health programs and services. |
According to the eHealth PIP, the program's performance is measured against the following key indicators:
- Percentage of First Nations using Panorama or an equivalent provincial integrated public health information system;
- Percentage of clinical telehealth sessions delivered to First Nations clients;
- Number of Digital Health Record systems (e.g., EMR) in communities;
- Percentage of First Nations with improved broadband connectivity (with speeds at or greater than 5 Mbps);
- Number of telehealth sessions delivered in each region by type (Clinical, Education, Administrative);
- Number of communities with health systems integrated with provincial systems (by type, by region); and,
- Number of communities that have access to remote presence technologies.
In consultations with program partners, it was noted that despite the inclusion of the above indicators in the eHealth PIP, only one indicator is regularly tracked by the program, and another single indicator is tracked by the Department.
According to the ISC Departmental Results Report, the eHealth program has not met the outlined target of 320 digital health record systems in First Nations communities, having achieved 300 in fiscal years 2019-2020 and 2020-2021.Footnote 86
The program data, however, provided results towards the indicator noting 'the number of telehealth sessions delivered', over the evaluation period, as shown in Table 3.
| Telehealth Session Type | Number of Telehealth Sessions DeliveredFootnote 87 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2016-17 | 2017-18 | 2018-19 | 2019-20 | 2020-21 | ||||||
| Target | Actual | Target | Actual | Target | Actual | Target | Actual | Target | Actual | |
| Clinical | Not applicable | 10,501 | 11,026 | 13,059 | 13,712 | 14,092 | 14,398 | 14,922 | 15,117 | 15,073 |
| Education | Not applicable | 2,171 | 2,280 | 2,757 | 2,895 | 3,260 | 3,040 | 3,059 | 3,192 | 2,582 |
| Admin | Not applicable | 1,592 | 1,672 | 1,134 | 1,191 | 1,055 | 1,250 | 1,317 | 1,313 | 451 |
| Total | 14,975 | 15,682 | 14,977 | 16,950 | 17,798 | 18,407 | 18,687 | 19,298 | 19,622 | 18,106 |
With the exception of fiscal year 2020-2021, the eHealth program has consistently surpassed the outlined target of an annual increase of 5% in sessions delivered over the previous year. This lapse was noted to be most likely due to the impacts of the pandemic on access to communities and resource availability to deliver sessions.
Case Study #5
First Nations of Québec and Labrador Health and Social Services Commission
Region: Québec and Labrador | Program Focus: Health Planning; HSIFCase Study #5 note 1; eHealth
The First Nations of Québec and Labrador Health and Social Services Commission continues to make notable strides towards objectives of the Cluster of programs under this review, including the delivery of an information network through the following activities:
- Information Security
- Information Management Systems
- Health Centers
- Electronic Medical Information
Additionally, the organization is involved in developing and implementing telehealth, as well as the deployment, implementation, and programming of quality information technology services and security. The organization remains committed to the protection of data, prioritizing its confidentiality, accessibility, and auditability.
Both internal and external partners shared that the eHealth program was instrumental in supporting First Nations through the pandemic, facilitating innovation and higher quality care. Program partners highlighted notable progress in their objectives to increase access to health services through initiatives such as telemedicine and virtual care (e.g., "doctor for a day"). Additionally, interviewees noted a significant effort around building the connectivity strategy (e.g., funding to improve connectivity within First Nation data centers). Interviews highlighted that eHealth technologies are in demand more than ever, and the support provided thus far has proven critical to improving access to health care services, including mental health and wellness programming.
Interviews with internal and external partners noted that people in First Nations communities often experience challenges in connectivity, data management, privacy, cybersecurity and maintenance of systems. It was highlighted that the current funding provided is insufficient to address these challenges and cover the long-term maintenance fees and rising costs of materials. Furthermore, the lack of appropriately trained staff to maintain and operate digital systems is a major barrier to the continued achievement of outlined objectives.
Throughout interviews, partners emphasized the complexity of the eHealth landscape, outlining the several layers associated with realizing the benefits of this technology, from the implementation of technology to deployment of systems. However, it was highlighted regularly that the pandemic has facilitated major improvements in the deployment, implementation, and uptake of virtual care and telemedicine. Further, partners noted that eHealth played a significant role in supporting vaccination roll out and tracking efforts during the COVID-19 pandemic by building data management and transfer capacities.
Finding #12: The HHR program has made progress towards increasing the number of Indigenous peoples studying and working in health care, funding training to over 4,690 community health care workers and awarding over 3,725 bursaries to Indigenous students studying in the health field since 2015-2016.
| Immediate | Indigenous people participate in post-secondary education leading to health careers; community-based workers are trained to improve the quality and consistency of health care services. |
|---|---|
| Intermediate | Improved access to high quality and culturally appropriate and safe health services. |
| Ultimate | First Nations and Inuit design, deliver and manage their health programs and services; communities are healthier; Indigenous people have reliable and sustainable infrastructure. |
Given the HHR objective of increasing the number of Indigenous students pursuing an education in a health profession as well as the number of community-based health care workers, this evaluation assessed the progress towards this objective since 2015. The HHR program is divided in two distinct streams each with its own respective objective. While managed by FNIHB, Stream 1 of this program is delivered in partnership with Indspire, while Stream 2 is supported by implementing partners such as the First Nations Health Managers Association (FNHMA) and other entities.
According to the HHR PIP, the program's performance is measured against the following key indicators:
- Number of bursaries and scholarships provided to First Nations, Inuit, and Métis students in a health-related field of study;
- Percentage of Indigenous bursary and scholarship recipients who are health-sector employed in a First Nations or Inuit community;
- Percentage of regions offering training to community-based workers using AHHRI funding;
- Percentage of First Nations, Inuit, and Métis working in the health sector in Canada; and,
- Number of community-based workers that have completed training in the fiscal year.
In alignment with the other Cluster programs, a review of program data indicated inconsistent tracking of key data points throughout the evaluation period. However, data was provided and reviewed in relation to most of the above noted indicators. The results are outlined by each stream below.
Stream 1: Bursaries
A review of Indspire program data from Fiscal Year 2019-2020Footnote 88 indicates that bursaries were awarded to over 700 Indigenous recipients, 49% of whom were status First Nations recipients, 3% of whom were non-status First Nations recipients, 4% of whom were Inuit recipients, and 44% of whom were Métis recipients. The bursaries awarded in 2019-20 had a total value of $2,550,000.Footnote 89
| Fiscal Year | Number of Awards | Amount Allocated |
|---|---|---|
| 2015-2016 | 764 | $2,405,072 |
| 2016-2017 | 709 | $2,380,113 |
| 2017-2018 | 901 | $2,556,000 |
| 2018-2019 | 646 | $2,550,000 |
| 2019-2020 | 705 | $2,550,000 |
| Over 5-Year Period | 3,725 | $12,441,185 |
| Fiscal Year | Number of Status First Nations Recipients | Number of Non-Status First Nations Recipients | Number of Inuit Recipients | Number of Métis Recipients |
|---|---|---|---|---|
| 2015-2016 | 359 | 31 | 15 | 359 |
| 2016-2017 | 340 | 35 | 21 | 312 |
| 2017-2018 | 441 | 38 | 29 | 393 |
| 2018-2019 | 290 | 26 | 28 | 302 |
| 2019-2020 | 348 | 21 | 29 | 307 |
| Over 5-Year Period | 1,778 | 151 | 122 | 1,673 |
The HHR PIP outlined a target of over 650 bursaries awarded, which was surpassed in every year except Fiscal Year 2018-2019.Footnote 92 Over 3,725 bursaries were provided to Indigenous students in health-related fields since 2015.
Program data received from fiscal year 2017-2018 to 2019-2020 provided greater depth of insight into the recipient profiles of the HHR program, as well as geographical reach.

Text alternative for Figure 16 - Breakdown of Bursary Recipients by Region
Figure 16 is a pie chart that represents program data of HHR bursary recipients from fiscal years 2017-18 through 2019-20 and their regional distribution. Throughout this timeframe, there were bursary recipients in Alberta (14%), British Columbia (16%), the Atlantic Region (17%), Saskatchewan (13%), Manitoba (17%), the Northern Region (2%), Ontario (19%), and Quebec (2%). 1 bursary recipient was outside of Canada.
Source: Indspire Program Data, retrieved 2022.
For example, as shown Figure 16, bursaries over the three-year period between 2017 and 2020 have been awarded to recipients predominantly in the Ontario, Manitoba, Atlantic, and BC regions, followed closely by Alberta and Saskatchewan.Footnote 93
Additionally, the data indicated that the most common programs of study with the health field for program recipients were Nursing, Medicine, and Kinesiology.Footnote 94

Text alternative for Figure 17 - Breakdown of Bursary Recipients by Programs of Study
Figure 17 is a bar chart that represents program data of HHR bursary recipients from fiscal years 2017-18 through 2019-20 by their field of study. Throughout this timeframe, there were bursary recipients in the fields of Nursing (41%); Medicine (15%); Kinesiology/Human Kinetics (10%); Pharmacy (3%); Dental medicine/assistant/hygienist (3%); Occupational & Physical Therapy (3%); Public Health (2%); and all other fields (22%).
Source: Indspire Program Data, retrieved 2022.
Indspire conducts periodic surveys to assess the impact of the program in support of achieving intended outcomes of supporting Indigenous education and subsequent employment in healthcare-related fields. In 2017, bursary recipients reported a 42% employment rate, though 53% of graduates went on to pursue a subsequent post-secondary qualification.Footnote 95
According to these same reports, in 2015, 80% of graduates of health-related programs were employed in roles servicing Indigenous populations. In 2017, this data was not broken down by field of study; however, of all bursary recipients, 61% of graduates were servicing Indigenous populations.
As funding has not increased over the years, the number of bursary recipients has decreased since Fiscal Year 2015-2016, after decreasing post-2018.
Overall, bursaries met 20% of financial need, with a variance between amounts requested and amounts rewarded of over $10M across the last five fiscal years.Footnote 96
Partners described a lack of notable increase in First Nations working in the health care system, highlighting that people in First Nations communities lack the required capacity to devote time to training and professional development.
In interviews with ISC Program Representatives, it was noted that the HHR program only tackled a portion of the challenges at hand by providing an education to First Nations, Inuit, and Métis students and hoping they return to their communities to support the health needs. However, the gap, according to interviewees, is in the lack of funding available to allocate towards addressing the current challenges (e.g., ability to provide accommodations, compensation) in staffing nurses, physicians, and other health care workers in community.
Further, interviewees highlighted that the existing program supports Indigenous students by providing funding to pursue studies or professions; however, there is no evaluation of the effectiveness of the chosen programs. This indicates a potential opportunity for improvement, given the health needs identified around the necessary level of training, both medical and cultural.
According to interviews, the limited funding available through the program translates to an inability to meet demand despite a desire from Indigenous students to pursue health care education.
Stream 2: Community-Based Worker Training
The second stream under HHR provides funding to recipients in order to pursue community-based healthcare related training, in support of the program's immediate, intermediate and ultimate outcomes.
A review of HHR program data across the evaluation period indicates progress towards outcomes under Stream 2, with training provided to almost 4,700 community workers since Fiscal Year 2015-16.
| Province | 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 | 2020-21 | Total | RE Percentage |
|---|---|---|---|---|---|---|---|---|
| AB | 68 | 75 | 75 | 60 | 50 | 75 | 403 | 9% |
| ATL | 125 | 82 | 100 | 150 | 75 | 130 | 662 | 14% |
| QC | 42 | 68 | 58 | 68 | 42 | 60 | 338 | 7% |
| ON | 75 | 75 | 82 | 86 | 68 | 82 | 468 | 10% |
| MB | 185 | 169 | 153 | 196 | 100 | 190 | 993 | 21% |
| NR | 112 | 78 | 86 | 115 | 150 | 119 | 660 | 14% |
| SK | 224 | 200 | 180 | 196 | 142 | 224 | 1,166 | 25% |
| National | 831 | 747 | 734 | 871 | 627 | 880 | 4,690 | |
The HHR program reached the target of providing training in 100% of regions in Canada by 2018.
One of the primary indicators tracked under the HHR program is the percentage of Indigenous people working in the health sector in Canada. The outlined target since 2019-20 has been 2.9%, which has been surpassed at 3% consistently. As a result of this continued success, the target for 2022-23 was raised to 3.3%. While the maintained target of 3% and the promising rise in Indigenous peoples working in health care since 2015 are positive results, the existing performance measure framework does not include the necessary level of analysis to conclude that the HHR program plays a significant role in increasing these numbers.
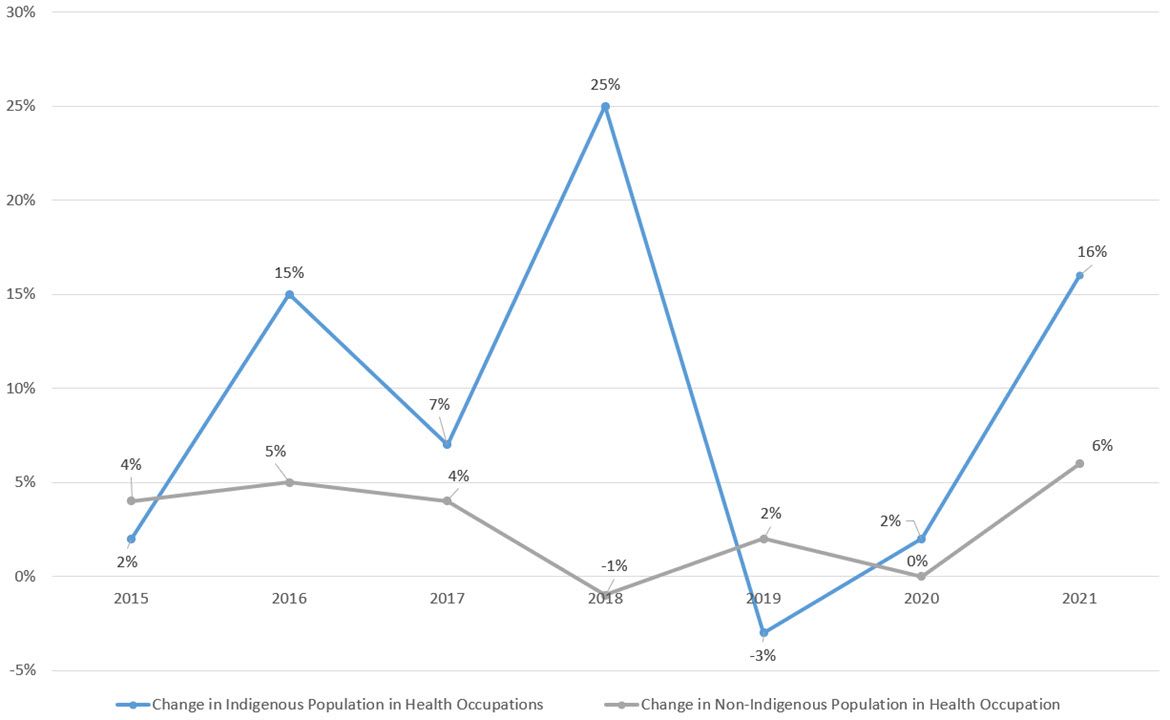
Text alternative for Figure 18 - Annual Percentage Change in Number of Indigenous peoples and Non-Indigenous People Working in Health Care in Canada
Figure 18 is a line chart with markers and represents Census Data from 2015-2021 noting the annual percentage change in the number of Indigenous peoples and non-Indigenous peoples working in health care in Canada. The year-over-year change in the percentage of the Indigenous population that works in health care was (from the baseline of 0%), up 15% 2015-16, up 4% 2016-17, up 26% from 2017-18, down 3% 2018-19, up 2% 2019-20, and up 16% 2020-21. The year-over-year change in the percentage of the non-Indigenous population that works in health care was (from the baseline of 0%), up 5% 2015-16, up 4% 2016-17, down 1% from 2017-18, up 2% 2018-19, unchanged from 2019-20, and up 6% 2020-21.
Source: Statistics Canada, 2023.
A review of literature highlighted that the number of Indigenous peoples working in health occupations has increased significantly between 2015 and 2021, rising from 28,300 to 50,200 (77%). As demonstrated in Figure 18Footnote 98, the number has fluctuated dramatically year-over-year, while the number of non-Indigenous population in the health sector is comparatively more steady.
Despite this increase, Indigenous people only account for 3% of the healthcare workforce in Canada while making up 5% of the Canadian total population (as of 2021).Footnote 99 Interviewees also noted challenges in availability and sustainability of funding and the capacity of people in First Nations and Inuit communities to take on training and professional development activities. Further, it was noted that the parameters of the type of training program participants can receive (i.e., training for non-regulated workers and community-based workers in health promotion and disease prevention) can be restrictive and limit the opportunities for individuals to gain relevant expertise to address key health needs in First Nations and Inuit communities.
It was noted during interviews that the annual cycle of funding disbursement is misaligned with the multi-year lens with which plans are often developed, creating challenges in the ability of First Nations and Inuit to sustainably increase the number of community-based workers. It was suggested by one stakeholder that the restriction of funding exclusively to community-based workers has both positive and negative impacts towards the achievement of objectives, as smaller communities might be able to train external staff and bring them into community more effectively than training the limited number of members who may not be interested in pursuing health care training.
Case Study #6
Onion Lake First Nation
Region: Saskatchewan and Alberta | Program Focus: Health Planning; HSIF; HFP; eHealth
A major challenge for the Nation is the volume of health human resources that are able and available to provide health services, including the lack of a reserve workforce who can support the core team when a situation requiring additional individuals arises. The case load for healthcare professionals performing services for the members of the Onion Lake First Nation is extraordinarily high, with one physician providing healthcare for all 7,006 individuals. Where possible, the Nation has adapted to create workaround supports, however, these are not sustainable and long-term solutions that are able to keep First Nations healthcare at the forefront. For example, where Onion Lake has been unable to secure funding for additional physicians, they have instead used funding to hire nurse practitioners to augment the current physician services. If the Nation can secure funding and subsequently recruit resources, they then face additional challenges related to retention. The healthcare system's fee for service standard is noted as not being attractive to practitioners, and the heavy workload with limited human resources potentially causing burnout and preventing healthcare providers from being able to take time off all contribute to the challenges associated with retaining service providers for the Nation.
One internal stakeholder noted that the Department is often forced to hire third-party agency nurses to fill the existing human resource shortages in First Nations and Inuit communities; however, they are rarely culturally trained. Further, it was noted by one Program Lead that it would be beneficial for the federal government to invest in early education opportunities to increase awareness and interest in health care career paths.
ISC Regional Staff highlighted an opportunity to increase the level of promotion and awareness of programs to increase uptake of the program by clarifying the types of education and training that are eligible. It was suggested that the program explore the implementation of a national guide that outlines these parameters.
Finding #13: The HFP reached a favourable rate of 84% of First Nation facilities receiving a condition rating of "good" in Fiscal Year 2020/21; however, the HFP has been unable to reach targets in other critical areas due to insufficient funding and resources as well as misaligned performance measures.
| Immediate | First Nations are supported to plan, design, and make other capital investments in their health infrastructure; and First Nations are supported to manage and maintain their health facility infrastructure. |
|---|---|
| Intermediate | Health facility infrastructure deficiencies are addressed; health facilities provide space for in-community health services delivery. |
| Ultimate | Indigenous people have reliable and sustainable infrastructure. |
The HFP aims to support First Nations in planning, designing, and making capital investments in their health facility infrastructure, as well as in managing and maintaining that infrastructure. In consideration of these objectives, the evaluation considers the extent to which this has been achieved thus far.
The HFP PIP outlines 10 original performance indicators that have been approved as of 2019; however, the program has since updated the PIP to include 16 proposed performance indicators that provide more useful or relevant information. Since these new performance indicators were developed part way through the evaluation period, many were either not completely applicable to this evaluation or the results will only be available after the period of time included under the evaluation. The tracking of data for the original version of the PIP remained inconsistent and did not include the comprehensive list of indicators. While it would not be expected that results would be available for all performance indicators in the updated PIP due to the timing of its development, some data was available.
According to the 2019 HFP PIP, the program's performance is measured against the following indicators:
- Percentage of SIF major capital projects that have signed contribution agreements in place;
- Percentage of existing Aboriginal Head Start facilities on reserve that have been repaired or upgraded;
- Number of designs for new or replacement health facilities that were completed in the current fiscal year;
- Percentage of recipients who received health facilities operations and maintenance (F – O&M) funding who have developed plans for managing their health infrastructure;
- Percentage of facility condition audit reports that were shared with First Nations building owners in the preceding year;
- Percentage of facilities that received health facilities operations and maintenance (F – O&M) funding in the preceding year;
- Number of health facilities that have been replaced or undergone renovations to improve quality;
- Percentage of "high priority" recommendations from facility condition audit reports that were addressed on schedule;
- Percentage of health facilities that have received a facility condition audit within 3 years;
- Percentage of health facilities that have been newly constructed or have undergone major renovations in the past ten years; and,
- Percentage of inspected health facilities that did not have critical property issues.
In the newly proposed 2022 PIP, the key indicator is:
- Percentage of First Nations health facilities with a condition rating of "good".
In consultations, HFP program partners noted that data was difficult to locate given the length of time lapsed since its collection and/or difficulty locating data due to inconsistent and varied storage locations. It was specifically noted that a majority of the indicators outlined in the previous PIP were no longer tracked as they did not provide useful or relevant Program information while those in the updated PIP were either not yet being collected or developed outside of the scope of this evaluation.
Recognizing historic difficulties in tracking and collecting data associated with performance indicators, the program is currently developing a more robust performance measurement and recording system and process so that all relevant information can be easily accessible.
Some of the results tracked for the 2019 PIP to date within the evaluation period are provided belowFootnote 100:
| Performance Measurement Indicator Results from Program Data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Performance Indicator | Percentage of FN health facilities that have received a facility condition audit within 3 years (2 years from 2019 onwards)Footnote 101 | Percentage of health facilities that have been newly constructed or have undergone major renovations in the past 10 years | Percentage of inspected health facilities that did not have critical property issues | Percentage of inspected health facilities with a condition rating of "good"Footnote 102 | ||||
| Fiscal Year | Target | Actual | Target | Actual | Target | Actual | Target | Actual |
| 2015-2016 | 100% | 30% | Not applicable | blank | 65% | 53% | Not applicable | Not applicable |
| 2016-2017 | 100% | 85% | Not applicable | blank | 65% | 68% | Not applicable | 94% |
| 2017-2018 | Not applicable | 44% | 65% | 60% | Not applicable | 80% | ||
| 2018-2019 | Not applicable | 13%Footnote 103 | 65% | Not applicable | Not applicable | 87% | ||
| 2019-2020 | 100% | 40% | Not applicable | blank | 65% | Not applicable | Not applicable | 87% |
| 2020-2021 | Not applicable | blank | 65% | Not applicable | Not applicable | 84% | ||
The HFP has contributed to improving health infrastructure in First Nations, having consistently surpassed targets laid out around the general condition rating of FN health facilities. However, the program has struggled to achieve progress in key targets around health facilities with critical issues and conduct of regular condition audits and tracking construction and major renovation projects against the inventory.
The COVID-19 pandemic impacted the ability of the HFP to achieve progress under certain indicators. For example, in 2020 and 2021, most facility audits/inspections were cancelled. Interviews with partners also highlighted challenges in achieving objectives due to a lack of sustainable funding to maintain and operate buildings, especially as costs of materials, delivery, and utilities have increased. External research indicates that the cost of non-residential business construction in Canadian Census Metropolitan Areas (CMAs) increased by 15% over the evaluation period.Footnote 104 Further, research shows that inflation has risen from 1.13% in 2015, to 3.4% in 2021, and an anticipated rate of 6.9% in 2023.Footnote 105
Internal partners highlighted that HFP annual budgets are based on calculations made 20 years ago and were never adjusted to account for economic changes over the years. This is a particular obstacle in the face of the pandemic, which exacerbated many economic challenges. One internal stakeholder even noted that a community had to transfer services back to the program due to an inability to keep up with the maintenance costs of the facilities without additional support.
The measurement of progress in this program was noted to be challenging because there is a perceived gap between the logic model's intermediate and ultimate outcomes, with one focused on infrastructure and the other on health outcomes. Further, program partners expressed concerns that they are not able to achieve either outcome due to existing barriers, most notably the lack of funding. The HFP program expenditures have experienced a notable decrease since Fiscal Year 2017/18, illustrating the barriers within which the program has been operating.Footnote 106
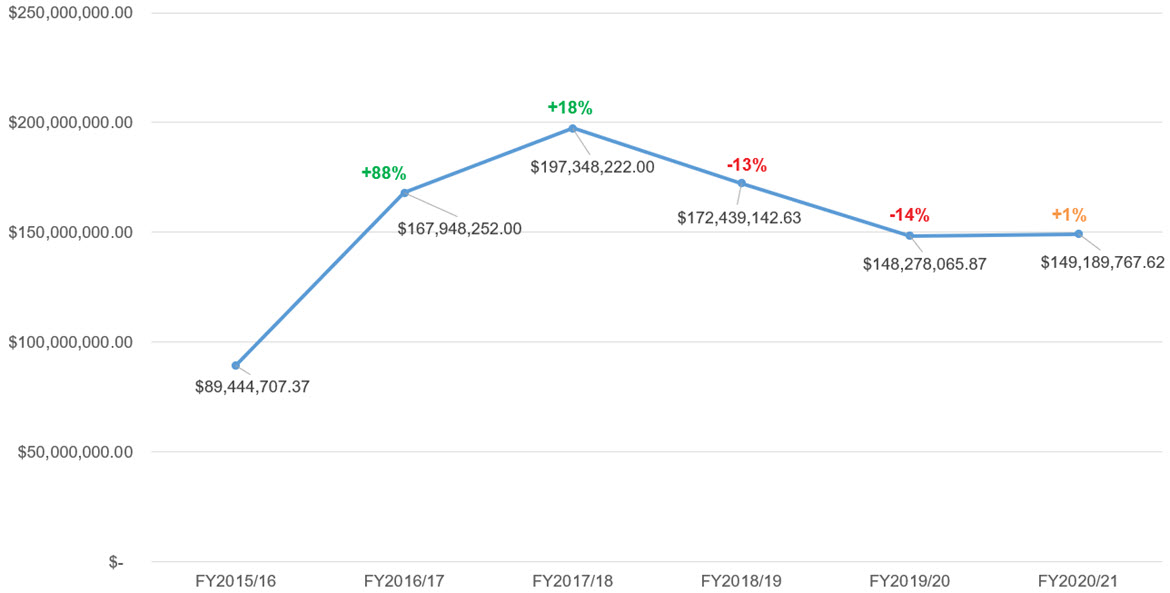
Text alternative for Figure 19 - HFP Program Expenditures
Figure 19 is a line chart with markers and represents the percentage change in HFP Program Expenditure data from fiscal years 2015-16 through 2020-21. The year-over-year change in program expenditures (from the baseline of $89.4M), up 88% from 2015-16 to 2016-17, up 18% 2016-17 to 2017-18, down 17% from 2017-18 to 2018-19, down 14% from 2018-19 to 2019-20, up 1% from 2019-20 to 2020-21.
Source: HFP Program Data, retrieved 2022.
According to interviews, when funding is provided to communities, it is often not sustainable to account for the maintenance of existing facilities. Often, funding provided is time limited; therefore, it does not allow for long-term planning. As a result, program partners shared that it is often more financially feasible to build new facilities than repair existing ones. However, the lack of funding available remains to be a primary challenge as there is limited funding available to build new facilities to begin with. To better allocate the limited funding available, the HFP developed a needs assessment and prioritization matrix to identify and target communities that could receive some funding for health facilities.
It is evident through interviews that despite the clear need for safe and accessible health facilities for First Nations and Inuit, the execution of the program is not as effective as it could be because of significant barriers that need to be overcome, particularly the lack of funding available.
Evaluation Question: How did the COVID-19 pandemic impact the delivery of the programs and their ability to support First Nations and Inuit?
Finding #14: The COVID-19 pandemic had significant impact on the delivery of health services, including creating obstacles in access to communities and barriers to obtaining the required resources for Cluster program delivery. However, new opportunities for service delivery were identified as a result of the changing operational environment resulting from the pandemic.
Note that Finding #4 in Relevance refers to the challenges faced by First Nations and Inuit as a result of COVID-19.
Impact of COVID-19 on Program Delivery
The impact of the COVID-19 pandemic on the core health needs of First Nations and Inuit was explored in the Relevance section of this report. In this section, the evaluation assesses the impact of the pandemic on the ability of the Cluster programs to effectively deliver their services.
In interviews, partners noted that the pandemic created several obstacles to program delivery, including:
- Limited access to communities to deliver care and engage First Nations and Inuit
- Diversion of resources towards COVID response and away from other health needs and priorities
- Staff in communities and within the Department experienced burnout, having the added burden of the COVID-19 response to their already excessive workloads
- Delays in Cluster program-funded project delivery
Despite the crisis, interviews highlighted that the pandemic resulted in some positive outcomes as well, including:
- Spotlight on First Nations health infrastructure gaps and needs
- Emphasis on value of eHealth technologies (e.g., access to virtual care)
- Emphasis on value of Accreditation (e.g., established governance structures and policies and procedures)
- First Nations adapted to the urgency of the pandemic, resulting in improved efficiencies in service delivery and quicker administration processes
- Collaboration with additional partners (e.g., HHR with Red Cross)
- Presence of the FNHA in BC facilitated a rapid response to COVID-19 in the Province and coordinated roll out of supports to BC First Nations
Access to Communities
It was noted by various interviewees that a key challenge for the delivery of health services throughout the pandemic was accessing First Nations and Inuit communities. To combat the spread of the virus, communities were required to completely shut down for months, creating increased barriers to delivering care. Further, maintaining communication with people in First Nations and Inuit communities was said to be particularly challenging, resulting in limited partner collaboration.
Diversion of Resources
When the pandemic hit in March 2020, it became the number one health priority worldwide, and First Nations and Inuit were no exception. According to interviews, the pandemic response required an all-hands-on-deck approach, dealing with quarantines, community shutdowns, vaccinations, and treatment for the virus. This left little time and even fewer resources to allocate to other health challenges. However, these other health needs did not cease to exist when the pandemic hit. In fact, many existing conditions were severely exacerbated by the virus or through the impact of the pandemic response. However, interviewees noted that there was no capacity in health treatment centers and no staff available to address anything but the most imminent of health threats.
The health care worker shortage was a challenge in First Nations and Inuit communities long before the pandemic; however, this shortage was dramatically exacerbated by the diversion of resources to pandemic efforts. Further, the labour demand on health care professionals was significant during the pandemic. Both frontline and administrative health care workers were overwhelmed with the non-stop crisis level urgency and were spread thin. As such, staff were unable to pursue additional training activities either.
Additionally, as a result of resources being diverted towards pandemic relief efforts, specific program activities were put on hold, such as the development of community health plans. HPQM program partners noted that this resulted in significant delays in the expected update or development of plans.
It should be noted that additional funding was provided by the Department to people in First Nations and Inuit communities to support the COVID-19 response. Without this additional injection of funding, existing health programs and services would have been even more adversely impacted. The impacts of the additional COVID-19 funding are further described below in the following sections.
Efficiency of Program Delivery
Throughout interviews, internal and external partners shared how First Nations were able to adapt in the face of the pandemic crisis and come together to deliver the necessary care to their communities.
Despite resource shortages from every perspective (financial, human, and material), interviewees noted how First Nations were able to achieve remarkable feats and apply their adaptive approaches to operate more efficiently. This highlighted the capacity that already exists in First Nations communities, and both internal and external program partners continuously expressed that with greater access to funding and resources, First Nations and Inuit could achieve so much more.
Interviews emphasized that through the pandemic, the Department was also able to work efficiently in order to provide short-term support rapidly. An example provided by a number of interviewees (14%) included the Department's procurement of short-term trailers and other physical pieces of infrastructures or measures (e.g., adapting schools, renting hotels) to be leveraged as isolation trailers for those infected with the virus, triage units to treat COVID patients, and overflow housing for health care staff.
Furthermore, ISC Regional Staff highlighted that alleviated reporting expectations during the initial years of the pandemic facilitated greater agility in program delivery because they were able to focus their efforts on emergency response and immediate needs instead of administrative tasks.
Lessons Learned for Future Health Crises
This evaluation also sought to understand if program partners learned any lessons to ensure better preparedness in the face of future health crises.
Emergency Preparedness
A significant number (20%) of interviewees noted that one of the key lessons learned throughout the pandemic was the importance of having emergency preparedness plans in place. In particular, partners noted the need for crisis management processes and mechanisms to be implemented in order to respond to any potential unprecedented disasters (e.g., floods, fires, etc.). Additionally, partners noted consideration should be made to medication distribution, vaccination programs, and health service delivery within a non-health centre context (i.e., triage units). Locating additional structures within which to provide care, vaccinations, and space for isolation was a challenge echoed by many. One Program Lead suggested integrating elements such as 'safe spaces' with separate entrances that can be used for immunization in the future.
A select number of partners highlighted the importance of community engagement on elements such as vaccinations to combat vaccine hesitancy. First Nation and Inuit communities were given priority access to COVID-19 vaccinations, which interviewees noted was very well appreciated; however, the process could have been even more effective had people in First Nations and Inuit communities had easy access to educational resources about the value and process of vaccinations in a pandemic setting.
As aforementioned, the Accreditation program's inclusion of emergency and disaster preparedness planning was particularly noted as valuable. In fact, when surveyed by the program, results indicated that health centres in communities that were accredited were better equipped to operate successfully during the pandemic, with 89% of organizations responding as such.Footnote 107 A review of the documented survey results demonstrated that First Nations and Inuit felt accreditation supported operations by ensuring policies and procedures were in place and protocols were followed, providing assurance to clients who felt safer knowing the facilities were accredited, having access to reliable information and webinars, and overall giving people in First Nations and Inuit communities a sense of confidence in their ability to provide quality care throughout the crisis.Footnote 108
The evaluation recognizes that one of the primary challenges with implementing any of these lessons remains securing adequate funding. Interviewees continuously noted the difficulty of planning for the future when constantly working to address the present emergencies while chronically understaffed and underfunded.
Case Study #7
File Hills Qu'Appelle Tribal Council (FHQTC)
Region: Treaty 4 Territory, SK | Program Focus: Health Planning; HSIF
The manner that ISC responded to the COVID-19 pandemic was largely regarded as effective and efficient in meeting the needs of communities. However, the pandemic response required communities to shift their focus from the usual services and programming that would typically be provided outside of an emergency situation. As a result, challenges such as food insecurity and disease or illness control were often exacerbated by the pandemic and have now become larger issues that require a significant effort to address. Specifically, cancer treatments were often paused or postponed so that the healthcare system could address the immediate needs of COVID-19, which is causing major concern now as the healthcare system works to clear a backlog of people who require treatment and who face escalating conditions as a result of not being able to receive treatment for a number of years.
The pandemic response from ISC involved regular dialogue and meetings with ISC, the Tribal Council, and the provincial Ministry of Health and Long-term Care (MHO) on a weekly basis to discuss the Council's needs and how ISC and the MHO could support those needs. ISC also provided funding in a timelier manner than pre-pandemic. The approach that was taken to COVID-19 response in which communication was timely, central, and incorporated all stakeholders was noted as a best practice to continuing to strengthen the relationship between ISC and First Nations.
Perceptions of COVID-19 Funding
In response to the COVID-19 pandemic, ISC committed to providingFootnote 109:
- An additional $285.1 million to support First Nations-led public health response.
- Additional health care resources, including medical supplies and equipment.
- 160 additional temporary assessment, screening, and isolation units.
- Surge capacity supports to community-based services in First Nations and Inuit communities.
Many of the Cluster programs were allocated additional funding to address the COVID-19 relief response. The COVID-related expenditures per program are outlined below. As such, through interviews, this evaluation assessed the extent to which the additional funding supported the efforts in communities.
| Cluster Program | COVID Special Expenditures | ||
|---|---|---|---|
| Fiscal Year 2019-20 | Fiscal Year 2020-21 | Total | |
| Health Planning and Quality Management | $5,775.09 | $10,942,708.70 | $10,948,483.79 |
| Health Services Integration Fund | $1,027.47 | $79,080.00 | $80,107.47 |
| Quality Improvement & Accreditation | blank | $21,805.24 | $21,805.24 |
| Health Facilities Program | $6,827,592.91 | $184,821,281.23 | $191,648,874.14 |
| eHealth Infostructure Program | $10,568.39 | $17,175,536.55 | $17,186,131.94 |
| Health Human Resources | $811.89 | blank | $811.89 |
Interviews with both internal and external partners highlighted the following perceptions of COVID-specific funding:
- Funding was allocated and received with greater efficiency
- Funding was highly valuable to addressing COVID needs
Depending on the program, the region, and the community, perceptions regarding the utility of COVID-19 funding was varied. However, a large portion of internal partners perceived it favourably.
A review of program data from eHealth supports this favourable perspective, which indicated that the program was able to allocate both the first and second waves of off-cycle surge funding of $17.4M towards a number of valuable initiatives across Canada, including launching an Indigenous Virtual Care Clinic in Alberta, expand telehealth to four additional sites in Ontario, covering EMR implementation licencing fees, and more.Footnote 111 Additionally, the nearly $200 million provided through the HFP was used to provide surge infrastructure and other applied solutions in communities to ensure a swift COVID-19 response.
One Program Lead discussed the ways in which they were able to mitigate funding challenges, including planning costs line by line to ensure funding was fully optimized. Certain program representatives noted that the additional funding facilitated the management of the pandemic as well as mitigation of health and wellness impacts such as the pandemic trauma. Furthermore, partners shared that they were able to pivot with agility to be responsive to immediate crisis events, describing funding as flexible, urgent, and well received by First Nations. However, they also noted that existing program funding was often repurposed towards pandemic relief initiatives out of necessity, and as such, additional COVID funding often could not bridge the existing and further exacerbated gap in resources.
Finding #15: The Accreditation and eHealth programs were instrumental to support First Nations in managing the pandemic crisis.
As discussed previously, the pandemic highlighted the need in First Nations and Inuit communities as well as the value of the services delivered through the Cluster programs. In addition to this spotlight, the pandemic also resulted in an increased demand for specific programs, most notably the Accreditation and eHealth programs. The value of Accreditation was particularly clear given that the accreditation process often requires organizations to develop safety plans as well as policies and procedures for emergency shutdowns or infection control. As such, interviewees noted that the importance of having these plans in place was especially clear during the pandemic.
A previous review of the QIAP indicated high effectiveness of the program. The review included a survey that revealed the followingFootnote 112:
- 89% of communities noted that accreditation supported their ability to manage the pandemic crisis.
- 81% of supported organizations indicated that accreditation has increased client safety.
- 85% of supported organizations indicated that accreditation has increased quality of care.
Most respondents, internal and external, noted that accreditation supported their response to the pandemic by enabling key services.Footnote 113

Text alternative for Figure 20 - Services Enabled by Accreditation
Figure 20 is a bar graph representing the percentage of survey respondents who identified specific service areas that have been enabled by QIAP. Survey respondents identified the following service areas as having been enabled by QIAP: Implementing infection prevention and control measures (94%); Accessing health services sites (90%); Providing communication (87%); Utilizing a pandemic and/or emergency plan (83%); Providing services (83%); Accessing traditional medicine and healing (75%); Accessing tele-remote health (72%); Implementing decisions (72%).
Source: QIAP Program Data, retrieved 2022.
Furthermore, the eHealth program was at peak demand during the pandemic period, given the requirements to limit physical contact while also continuing to provide health care in the midst of lockdowns and isolation measures. The value of virtual care and telemedicine became evident. Not only were these technologies supportive in the delivery of standard and COVID-related care, interviewees noted that they were also leveraged to provide access to mental health care, which was of particular importance given the psychological strain and trauma many endured during the pandemic.
In interviews, eHealth program partners shared that eHealth technologies were leveraged in the vaccination roll out during the pandemic, supporting the management of data to track the number of First Nations members who received vaccinations and provide them with the appropriate paperwork to demonstrate their vaccination status. One program partner noted they were able to partner with COVaxON (the system used to track COVID vaccination information in Ontario) by leveraging their EMR to easily migrate vaccination data to COVaxON. This helped ensure that the vaccination status of First Nations members was accurately tracked and stored in the broader provincial system.
Other programs were also innovative in their ability to pivot in the pandemic to optimize opportunities, including HHR. According to interviews with program partners in one region, HHR partnered with Red Cross and the FNHMA Help Desk for Indigenous Leadership to provide First Nations with a trustworthy communication channel through which they could seek advice or be directed to the necessary resources to help them navigate the pandemic, independent of the government. Additionally, HFP partners noted that organizations used the semi- or full lockdown periods to undergo construction at their health facilities (e.g., treatment centres) to address much needed structural changes.
While the increase in demand for Cluster programs is a positive outcome from the pandemic, this affected the already limited capacity in some First Nations to provide healthcare services and programs to meet demand, given that funding remained insufficient, and First Nations continued to struggle with staffing shortages.
Evaluation Question: How effective/productive are the relationships between partners within each of the programs (e.g., between ISC Headquarters and regional offices, First Nations and Inuit, implementing partners, provincial and municipal governments, etc.) and between programs?
Finding #16: Relationships between program partners were perceived as generally effective (though varied by region, program, and stakeholder group). However, challenges were identified regarding staff turnover and capacity as well as communication between ISC HQ and ISC Regions.
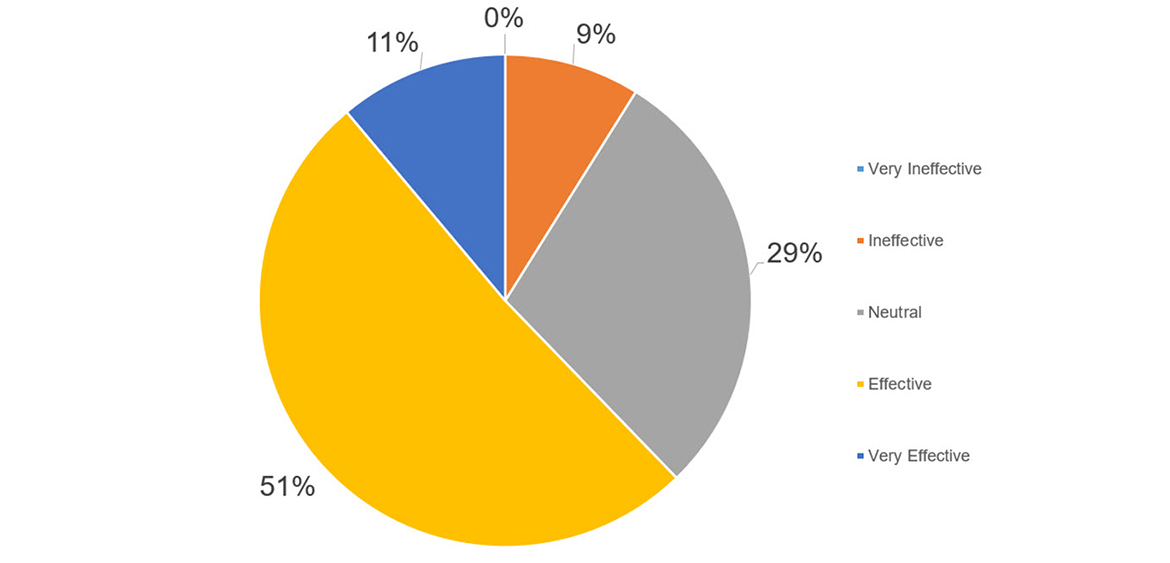
Text alternative for Figure 21 - Overall Effectiveness of Relationships Between Program Partners
Figure 21 is a pie chart that illustrates key informant interview perceptions of the overall effectiveness of relationships between program partners. Responses were on a scale and include Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. Responses were Very Ineffective (0%), Ineffective (9%), Neutral (29%), Effective (51%), and Very Effective (11%).
Source: Interviews by ISC Evaluation, 2022-2023.
A key element of a successful partnership is strong relationships. This evaluation sought to understand the perception of relationships between various program partners.
In interviews, partners (Program Leads, ISC Regional Staff, Implementing Partners, Subject Matter Experts) were asked to share their perceptions on the effectiveness of the relationships between program partners.
Overall, results indicated that perceptions of relationships between all program partners (in the aggregate) across all stakeholder groups interviewed were positive, with 51% rating relationships as Effective, 29% as Neutral and 11% as Very Effective. However, 9% of interviewees noted that relationships were ineffective.
When the data is broken down further by stakeholder groups responses, it indicates that perspectives are aligned, as each group's proportionate ratings are trending in the same direction (largest number of ratings for Effective, least number of ratings for Ineffective).
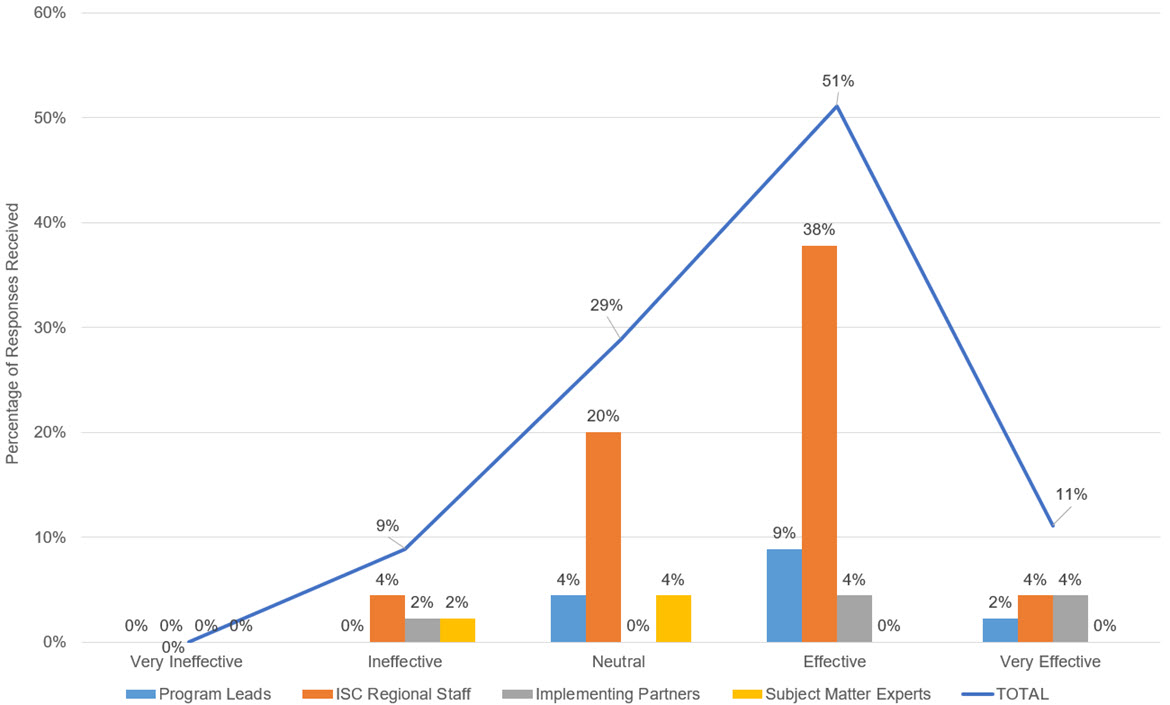
Text alternative for Figure 22 - Overall Effectiveness of Relationships Between Program Partners
Figure 22 is a bar chart that illustrates the perceptions of key informant interviewees on the overall effectiveness of relationships between program partners. Responses were on a scale and include Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. The responses of program leads were Very Ineffective (0%), Ineffective (0%), Neutral (4%), Effective (9%), and Very Effective (2%). The responses of ISC regional staff were Very Ineffective (0%), Ineffective (2%), Neutral (0%), Effective (4%), and Very Effective (4%). The responses of Subject Matter Experts were Very Ineffective (0%), Ineffective (2%), Neutral (4%), Effective (0%), and Very Effective (0%).
Source: Interviews by ISC Evaluation, 2022-2023.
The effectiveness of relationships was noted to be particularly difficult to assess by partners in interviews, and many specified that effectiveness of relationships often varied from individual to individual. Most interviewees shared that there were both very strong and very challenging relationships within their programs.
In certain focus groups and interviews, the question was further broken down to distinguish effectiveness of relationships between ISC HQ and Regions, between Regions and First Nations/Inuit, between Implementing Partners and ISC, and between various Implementing Partners. Key findings for each of these relationships is provided in more detail below.
Relationships Between ISC HQ and ISC Regions
Perceptions of partners about the relationship between ISC HQ and Regions varied across interviews. Of the regional partners who were specifically asked about the effectiveness of their relationships with ISC HQ, a large portion of respondents rated it as Effective (45%) or Neutral (27%), while the rest evenly rated (9%) across the other three options.

Text alternative for Figure 23 - Effectiveness of Relationships Between ISC HQ and ISC Regions
Figure 23 is a bar chart that illustrates key informant interviewees perception of the effectiveness of relationships between ISC headquarters and ISC regional staff members. Responses were on a scale and include Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. The responses of program leads were Very Ineffective (9%), Ineffective (9%), Neutral (27%), Effective (45%), and Very Effective (9%).
Source: Interviews by ISC Evaluation, 2022-2023.
When asked to elaborate, internal partners noted that relationships were good but had areas for improvement, particularly in the areas of organizational culture and communication. It was noted that the nature of ISC's mandate to transfer services and the large-scale transformation this would entail creates natural challenges with some ISC staff who may be more resistant to change. The required organizational culture for change was noted to be lacking by a significant number of interviewees.
In regard to communication, partners noted that internal communication continues to present challenges because the role of ISC HQ in program delivery has changed over the years. According to interviews, there is a lack of required support from ISC HQ to regions in terms of clear directives and sustainable resources. Some Cluster programs, such as the HFP, have made recent efforts to improve the relationship between ISC HQ and the regions by hosting bi-lateral meetings twice a month and gaining an increased understanding of the challenges and lessons learned their respective groups experience. It was also noted during interviews that consistent messaging from ISC HQ to the regions to ensure that the regions and subsequently the people in First Nations and Inuit communities they are supporting have a clearer understanding of the funding that is available in order to be able to better support First Nations and Inuit in affirming their vision of control.
Relationships Between Regions and First Nations and Inuit
Overall, perceptions of relationships between ISC regions and First Nations and Inuit were positive. Of the regional representatives who were asked to comment specifically on their relationships with First Nations and Inuit, the majority rated the relationships as Effective (58%) or Very Effective (33%).
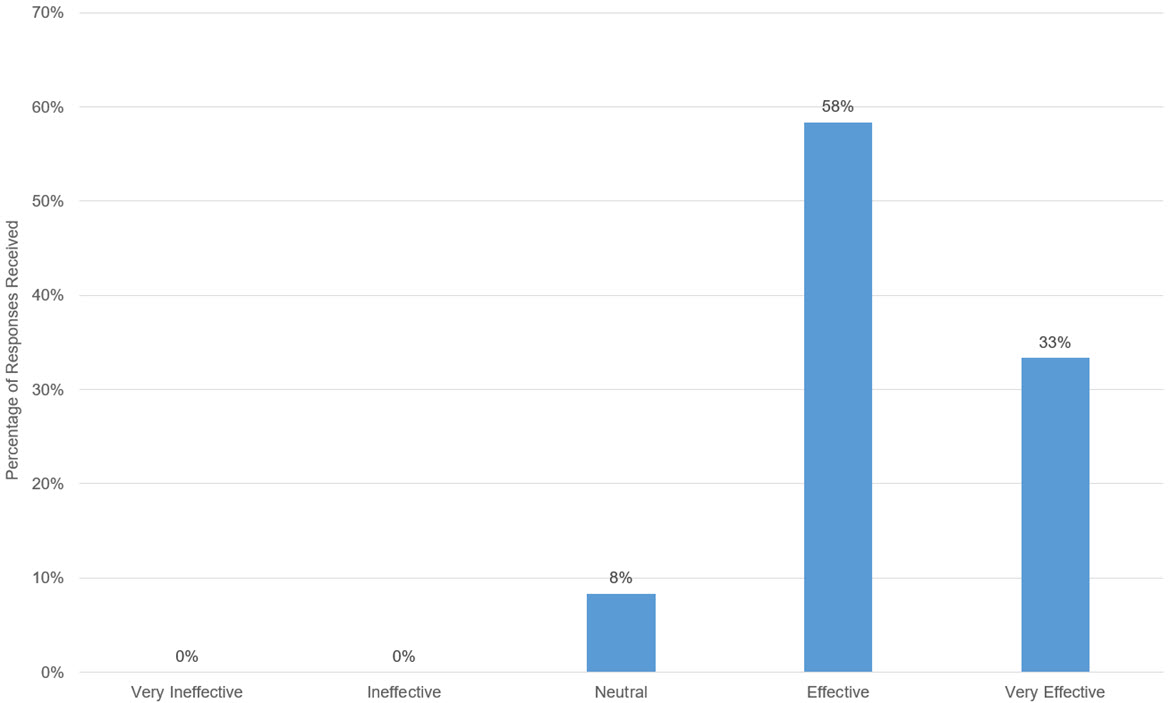
Text alternative for Figure 24 - Effectiveness of Relationships Between ISC Regions and First Nations and Inuit
Figure 24 is a bar chart that illustrates key informant interviewees perception of the effectiveness of relationships between ISC regional staff and First Nations and Inuit. Responses were on a scale and include Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. The responses of program leads were Very Ineffective (0%), Ineffective (0%), Neutral (8%), Effective (58%), and Very Effective (33%).
Source: Interviews by ISC Evaluation, 2022-2023.
Regional representatives highlighted the importance of transparency, honesty, and collaborative communication in their ability to build lasting relationships with people in First Nations and Inuit communities. The need to manage expectations and delineate between what First Nations and Inuit want to do and what they need to do was noted to be specifically challenging. Interviewees emphasized that building meaningful relationships allows First Nations and Inuit to feel comfortable approaching the regions with their priorities. However, it was noted during interviews that limited capacity and staffing shortages both within ISC Regions and within communities creates obstacles for both groups being able to dedicate time for meaningful engagement and collaboration.
It was noted in a select number of interviews that relationships were strained during the pandemic due to the loss of regular, face-to-face contact and engagement; however, the expectation is that this will change as communities begin to open their doors once more and travel resumes.
Partners highlighted that any changes in program regional leads should require orientation, training, and relationship building in order to maintain the relationships built between ISC regions and First Nations and Inuit; however, adequate resources to ensure this occurs is currently not provided.
Relationships Between First Nations and Inuit and Implementing Partners
During interviews, it was noted that relationships between First Nations and Inuit and implementing partners are strong and effective. Interviewees shared that there is a desire to increase the level of integration between community facilities and potential delivery partners, such as regional health authorities or organizations such as Aboriginal Health Access Centres.Footnote 114
HHR and QIAP partners noted effective relationships between First Nations and Inuit and accrediting bodies as well as strong relationships with partner groups, including the ITK and AFN. Partners interviewed from accrediting bodies highlighted extremely effective relationships with people in First Nations and Inuit communities, which allow them to better understand and respond to their needs.
Relationships Between Implementing Partners and ISC
It was noted by one Implementing Partner that as a result of their relationship with ISC strengthening through the pandemic, they were able to operate more effectively and efficiently (i.e., seek approvals with more ease).
Implementing partners also noted the value of cultural competency training being provided to ISC staff to ensure the appropriate level of understanding to operate effectively. It was highlighted that there have been occasions where Implementing Partners feel they must take it upon themselves to 're-teach' this training to staff in the absence of the required training and cultural competency.
Relationships Between Various Implementing Partners
A select number of implementing partners noted the gap in collaboration with other implementing partners in the same space, highlighting the potential value of working together to support First Nations and Inuit rather than as competitors. Additionally, it was highlighted by implementing partners that these programs are in a complex set of relationships with various related departments (e.g., Crown-Indigenous Relations and Northern Affairs Canada, Health Canada, Public Health Agency of Canada, etc.) and the communication amongst these parties should be improved to clarify roles and responsibilities (i.e., support a whole-of-government approach).
To further supplement the information gathered through interviews, respondents to the survey conducted were asked to indicate which relationships needed to be strengthened in order to improve the Cluster programs' functions. In alignment with the above noted interview data, survey results suggest opportunities to improve relationships between all program partners, though the relationship between ISC HQ and ISC Regions was highlighted the most frequently, followed by the relationship between ISC Regions and First Nations and Inuit, and closely afterward by the relationship between ISC Regions and Provinces/Territories (PT).
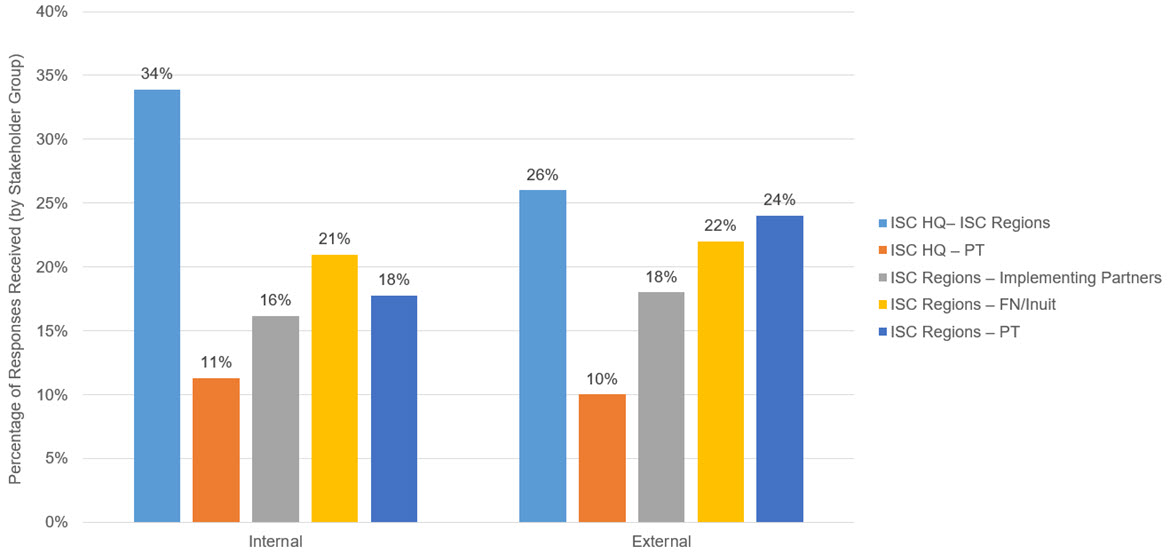
Text alternative for Figure 25 - Which relationships need to be strengthened to improve the program's function?
Figure 25 is a bar chart that illustrates survey respondents' responses to the question "Which relationships need to be strengthened to improve the program's function?" Internal (to ISC) respondents noted the following relationships needed to be strengthened: ISC headquarters and ISC regional staff (34%); ISC headquarters and Provinces/Territories (11%); ISC regional staff and Implementing Partners (16%); ISC regional staff and First Nations and Inuit (21%); ISC regional staff and Provinces/Territories (18%). External (to ISC) respondents noted the following relationships needed to be strengthened: ISC headquarters and ISC regional staff (26%); ISC headquarters and Provinces/Territories (10%); ISC regional staff and Implementing Partners (18%); ISC regional staff and First Nations and Inuit (22%); ISC regional staff and Provinces/Territories (24%).
Source: Survey deployed by ISC Evaluation, 2022.
Throughout interviews, several partners shared feelings of frustration related to the inability to surpass the surface relationships and make substantial progress towards real change. Further, interviews highlighted that ISC has been experiencing consistent turnover, and a review of internal ISC data1 indicated that in recent years, the churn rate of HQ and regional program staff working in the Cluster programs rose from 4% in Fiscal Year 2020-21 to 12.8% in Fiscal Year 2021-22. In Fiscal Year 2020-21, turnover was particularly high within the eHealth Infostructure program (6.2%) and overall, within the Alberta (13.1%) and Manitoba (8.7%) regions.
This was noted to be particularly challenging following FNIHB's transition from Health Canada to ISC, given the significant turnover and adjustment period required for new staff. This was further exacerbated by the pandemic, which created even more turnover, along with challenges in capacity and the ability to engage and collaborate with other partners, potentially due to challenges associated with having to limit in-person interactions.
Finding #17: There is a need for increased clarity of communication about
1. roles and responsibilities and
2. the departmental mandate of service transfer between program partners.
Communication is a vital element of an effective relationship. This evaluation included an assessment of the clarity and adequacy of communication to key partners.
When interviewees were asked about their perception of overall clarity and adequacy of communication between key program partners, internal respondents were primarily neutral (80%), with a fifth (20%) indicating a high level of clarity/adequacy. External respondents were more positive, with the majority indicating that communication is clear/adequate (75%) and a quarter (25%) noting communication as very clear/adequate.Footnote 115
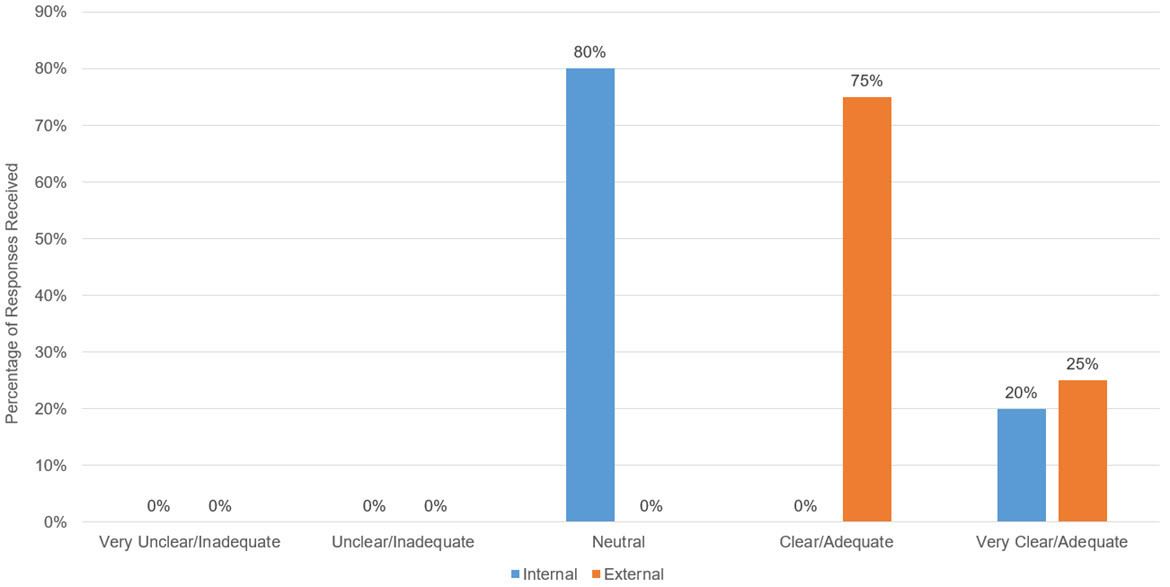
Text alternative for Figure 26 - Overall Perception of Clarity and Adequacy of the Communication Between Key Program Stakeholders
Figure 26 is a bar chart that illustrates key informant interviewees perception of the clarity and adequacy of the communication between key program stakeholders. Responses were on a scale and include Very Ineffective/Inadequate, Unclear/Ineffective, Neutral, Clear/Effective, and Very Clear/Effective. Internal (to ISC) responses were Very Ineffective/Inadequate (0%), Unclear/Ineffective (0%), Neutral (80%), Clear/Effective (0%), and Very Clear/Effective (20%). External (to ISC) responses were Very Ineffective/Inadequate (0%), Unclear/Ineffective (0%), Neutral (0%), Clear/Effective (75%), and Very Clear/Effective (25%).
Source: Interviews by ISC Evaluation, 2022-2023.
The survey indicated that more partners agree or strongly agree (32%) that communication among partners is effective than those who disagree or strongly disagree (21%). However, a notable portion of respondents indicated that they didn't know (23%).
The survey results demonstrated the nuance between partner relationships, and how they differ by region, by program, and by stakeholder group. The graph below indicates that communication is strongest between ISC HQ and Provinces/Territories, as well as ISC Regions and First Nations and Inuit, and weakest between ISC HQ and ISC Regions.
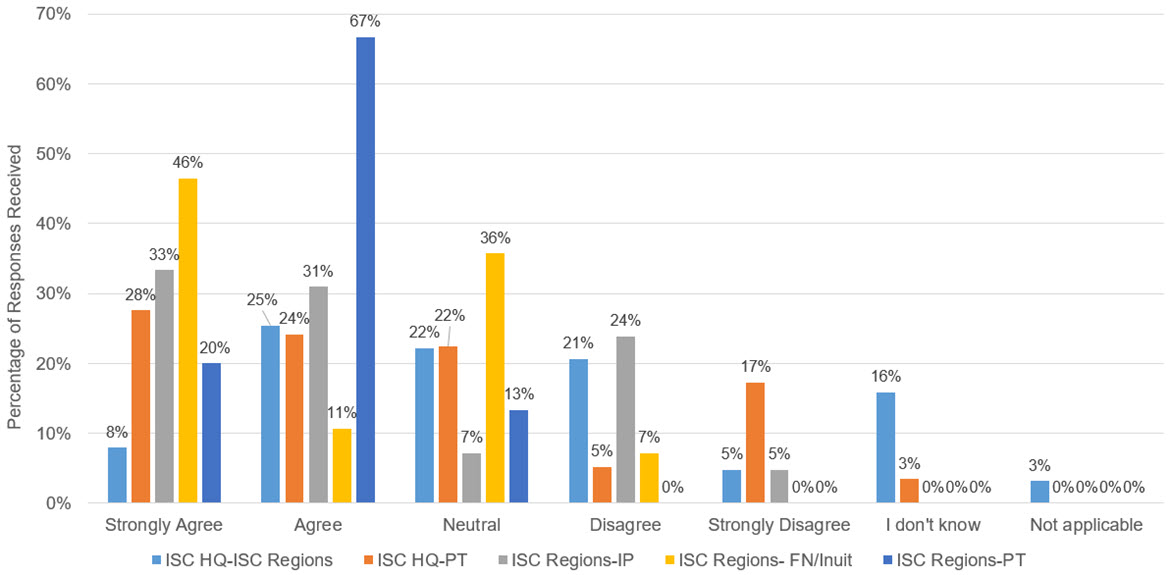
Text alternative for Figure 27 - Perception of partners that there is effective communication between program partners
Figure 27 is a bar chart that illustrates survey responses on the perception of partners that there is effective communication between program partners. Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Responses regarding the relationships between ISC headquarters and ISC regional staff were Strongly Agree (8%), Agree (25%), Neutral (22%), Disagree (21%), Strongly Disagree (5%), I don't know (16%), and Not Applicable (3%). Responses regarding the relationships between ISC headquarters and Provinces/Territories were Strongly Agree (28%), Agree (24%), Neutral (22%), Disagree (5%), Strongly Disagree (17%), I don't know (3%), and Not Applicable (0%). Responses regarding the relationships between ISC regional staff and Implementing Partners were Strongly Agree (33%), Agree (31%), Neutral (7%), Disagree (24%), Strongly Disagree (5%), I don't know (0%), and Not Applicable (0%). Responses regarding the relationships between ISC regional staff and First Nations and Inuit were Strongly Agree (46%), Agree (11%), Neutral (36%), Disagree (7%), Strongly Disagree (0%), I don't know (0%), and Not Applicable (0%). Responses regarding the relationships between ISC regional staff and Provinces/Territories were Strongly Agree (20%), Agree (67%), Neutral (13%), Disagree (0%), Strongly Disagree (0%), I don't know (0%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
To further supplement the quantitative information gathered through interviews and surveys about the adequacy of communication among partners, interviews highlighted specific comments:
Interviews indicated that constant communication takes place between ISC HQ and ISC Regions, regular committee meetings occur with national First Nations groups such as the AFN, and information flows effectively. Programs shared examples of different communication channels in interviews. For example, eHealth noted that they attend the Digital Health Conference regularly to remain up to date on any emerging changes in the industry and continue conversations with key players. It was noted, however, that pre-pandemic communication channels were stronger due to regular in-person meetings and presentations from projects, which interviewees noted facilitated clearer communication and understanding.
In discussions with external partners, a select number of interviewees raised concerns regarding their ability to contact and communicate with ISC program representatives. It was noted that they would benefit from having representatives that are more accessible and can visit the community to provide guidance and share knowledge.
The aforementioned turnover of ISC staff was highlighted during interviews in response to the question about adequacy of communication, with interviewees emphasizing that the turnover results in a major communication breakdown. Without the consistent presence of ISC staff within regions, the ability of ISC regions being able to understand First Nations and Inuit priorities and needs is affected and can result in a lack of adequate advocacy for funding to address those needs.
Despite predominantly positive survey and interview results around communication, specific areas of challenge were noted in interviews with both internal and external partners about roles and responsibilities and the departmental mandate of service transfer.
Clarity and Division of Roles and Responsibilities
Survey data indicated that partners have a varied perception of the clarity and adequacy of roles and responsibilities within their respective programs. Internal partners agree (47%) most consistently, while external partners are neutral (36%).

Text alternative for Figure 28 - The role and responsibilities of this program and its staff are clearly defined, well understood and communicated effectively
Figure 28 is a pie chart that illustrates survey responses to the statement "The role and responsibilities of this program and its staff are clearly defined, well understood and communicated effectively". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (3%), Agree (47%), Neutral (19%), Disagree (19%), Strongly Disagree (36%), I don't know (14%), and Not Applicable (0%). External (to ISC) responses were Strongly Agree (21%), Agree (14%), Neutral (36%), Disagree (14%), Strongly Disagree (14%), I don't know (0%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
While internal partners generally responded positively in the survey about the clarity of roles and responsibility, interviewees noted a need to improve the clarity of the division of roles and responsibilities between HQ and ISC Regions, particularly when faced with challenges associated with insufficient funding. According to interviews, ISC HQ used to be responsible for managing program budgets and allocating funding to regions based on workplans that are submitted by the regions. However, the roles have since changed and ISC HQ now has minimal control over funding allocations; it is the regions that hold the authority and determine how funding is allocated within the region. Due to internal changes such as this, it was noted in one focus group that there is sometimes confusion internally around who to contact for when questions arise about program administrative processes and approvals. Further, partners highlighted that leadership changes that occur both internally within ISC and externally within First Nations and Inuit communities can cause shifts in priorities or approaches to address those priorities. This can result in challenges in maintaining clarity of roles and responsibilities both internally between HQ and Regions, and subsequently between regions and First Nations and Inuit. In particular, internal partners noted a need for clarity around roles and responsibilities within service transfer, including post-transfer support to First Nations and Inuit. There may be an opportunity to ensure internal, foundational ISC processes that support the achievement of the department's goals related to the Cluster's programs are clearly defined, documented, and communicated. These processes should allow for a certain degree of flexibility should priorities shift but should also support an increased alignment of expectations between program partners and First Nations and Inuit around program-related roles and responsibilities.
Communication About Service Transfer
In the survey conducted, internal partners were asked whether they perceive information regarding service transfer was communicated effectively to their teams. Results were varied, with a large portion of respondents indicating that they Agree (31%), were Neutral (25%), or Disagree (22%).
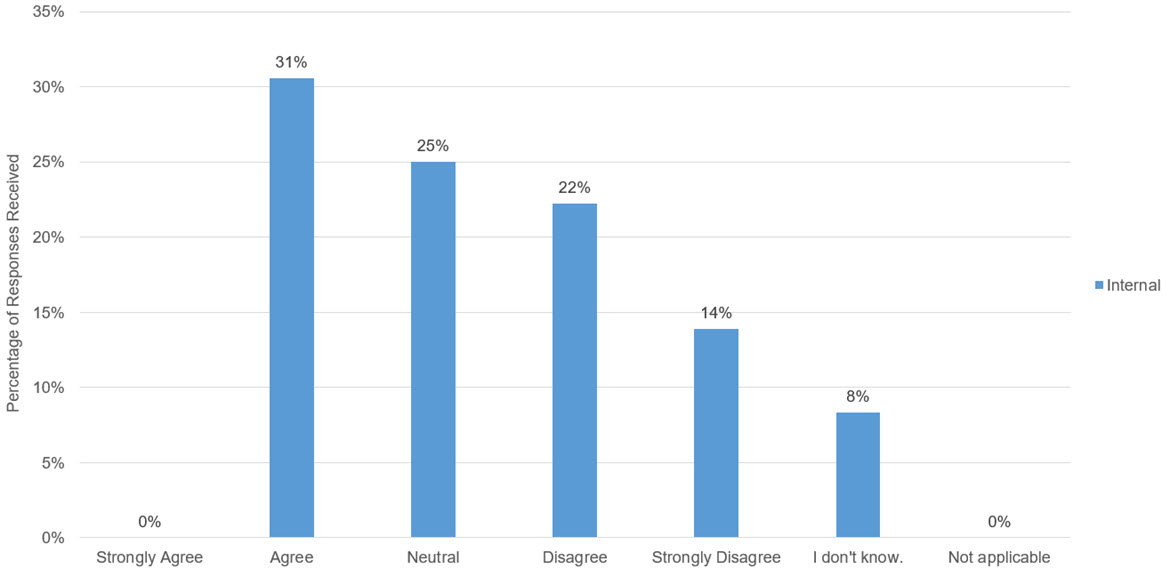
Text alternative for Figure 29 - Information about service transfer is communicated effectively to me and my team
Figure 29 is a bar chart that illustrates survey responses to the statement "Information about service transfer is communicated effectively to me and my team". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (3%), Agree (47%), Neutral (19%), Disagree (19%), Strongly Disagree (36%), I don't know (14%), and Not Applicable (0%). Note that this question was not included in the survey that was provided to external respondents.
Source: Survey deployed by ISC Evaluation, 2022.
In interviews, the lack of clarity in communication about the departmental mandate of service transfer was said to be due to the following factors:
- Departmental transfer of programs from Health Canada to ISC and resulting turnover resulted in a lack of understanding of the departmental mandate, particularly with regards to how the Cluster programs are meant to be supporting the achievement of broader service transfer to First Nations and Inuit. It was also noted that there is a lack of clarity around "small 't' transfer" of specific health programs and services versus full-scale "big 'T' transfer" of complete health systems means for both ISC and people in First Nations communities, particularly about how the former may present barriers to the latter, or how the former may be used to support the achievement of the latter.
- Cluster program siloes result in a lack of alignment in approach to service transfer creating difficulties in operationalization.
- Information sharing protocols act as a barrier, as documents that are classified cannot be shared from ISC internal partners and external implementing partners (i.e., FNHA) in alignment with the Security of Information Act, which restricts who can be communicated with, precluding conversations and relationship-building efforts with key partners.
Partners noted that increased collaboration across Cluster programs around service transfer messaging would improve alignment in approach, particularly because the Cluster programs' objectives are already well-aligned with each other (i.e., from a program design perspective). Additional details about collaboration amongst Cluster programs are provided in the next Finding.
Finding #18: Program partners perceive that the Cluster programs are operating in siloes, hindering productivity and effectiveness of program design and delivery. There is an opportunity for increased, intentional collaboration among programs.
Interviewees highlighted that there are clear linkages between all programs within the Cluster because they are all working towards common objectives and are foundational to achieving eventual service transfer. Some partners noted that HPQM and Accreditation are the building blocks of the Cluster, in that they support First Nations and Inuit in building an effective foundation on which to deliver health programs and services that meet their unique needs (e.g., identifying First Nations and Inuit needs and priorities, developing policies and procedures, establishing governance mechanisms, defining roles and responsibilities, etc.). This was further highlighted in the survey conducted where partners were asked to indicate which other health infrastructure services they collaborate with to perform their duties. 31% of internal partners noted the HFP as the health infrastructure service they collaborated with to perform their duties, followed by HPQM (17%), QIAP and eHealth (11% respectively), then HSIF and HHR (10% respectively). However, 11% of internal partners surveyed indicated 'none of the above'.
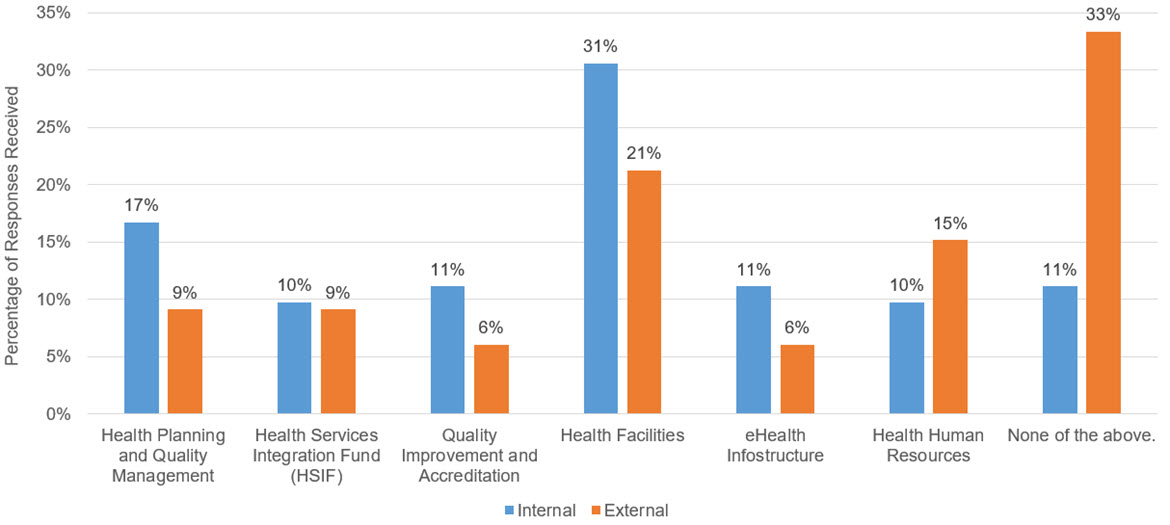
Text alternative for Figure 30 - Which other health infrastructure support services do you collaborate with to perform your duties?
Figure 30 is a bar chart that illustrates survey responses to the question "Which other health infrastructure support services do you collaborate with to perform your duties?". Internal (to ISC) responses received were Health Planning and Quality Management (17%); Health Services Integration Fund (10%); Quality Improvement and Accreditation (11%); Health Facilities (31%); eHealth Infostructure (11%); Health Human Resources (10%); and None of the Above (11%). External (to ISC) responses received were Health Planning and Quality Management (9%); Health Services Integration Fund (9%); Quality Improvement and Accreditation (6%); Health Facilities (21%); eHealth Infostructure (6%); Health Human Resources (15%); and None of the Above (33%).
Source: Survey deployed by ISC Evaluation, 2022.
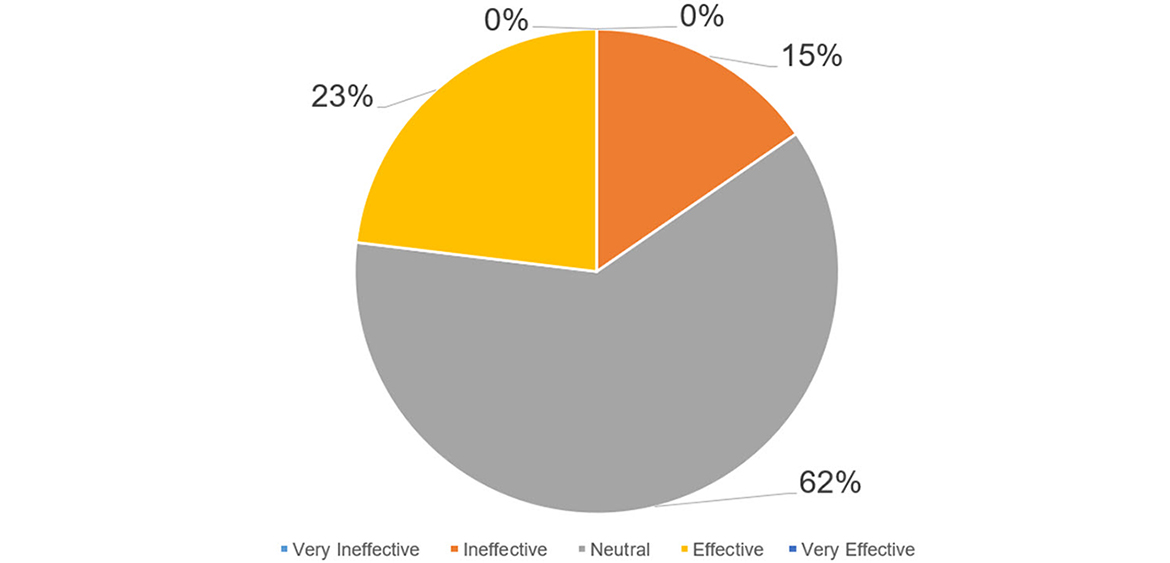
Text alternative for Figure 31 - Effectiveness and Productivity of Relationships Between Programs
Figure 31 is a pie chart that illustrates key informant interviewees perception of the effectiveness and productivity of relationships between the programs within the Cluster. Responses were on a scale and include Very Ineffective, Ineffective, Neutral, Effective, and Very Effective. Responses were Very Ineffective (0%), Ineffective (15%), Neutral (62%), Effective (23%), and Very Effective (0%).
Source: Interviews by ISC Evaluation, 2022-2023.
To further supplement the information gathered through surveys, partners were asked during interviews to provide their perception of the effectiveness and productivity of relationships between programs. The majority of respondents indicated Neutrality (62%), followed by Effective (23%), and Ineffective (15%). The results support overall commentary received from interviews around a lack of meaningful interaction between programs. According to interviews, programs do not have many opportunities to collaborate, and some interviewees who indicated Neutrality with regards to this question did so as they felt as though there was no true relationship between Cluster programs to comment on. One program regional representative highlighted that the relationships between programs tend to be informational but not highly collaborative. It was also highlighted that the regionalization of the Cluster programs creates siloes make it more difficult to identify potential commonalities between programs or take advantage of potential efficiencies. The common sentiment shared during interviews was that the programs work well in the same ecosystem; however, there is minimal communication or intentional collaboration amongst programs.
It is important to note that there were variations in responses between programs and regions, where some partners noted that the complementarity of some Cluster programs may be leveraged more heavily in some areas more than others. For example, program representatives noted that eHealth collaborated closely with the HFP and HPQM, particularly during the pandemic, to ensure isolation facilities, including aspects such as broadband connectivity and personal protective equipment, were made available to people in First Nations and Inuit communities as part of the pandemic response.
Through the survey, internal and external respondents were asked if there were other Cluster programs that collaboration with would increase benefits to First Nations and Inuit. Responses were almost evenly varied in both groups, with the most commonly indicated response for Internal partners being HFP (19%), followed by QIAP, HSIF, HHR and None of the Above evenly selected (14% respectively), then eHealth (13%), and HPQM (11%). External partners had similar leading trends, with HFP, QIAP, and HHR (17%) evenly selected, followed by HPQM (15%), HSIF (13%), and eHealth (11%).

Text alternative for Figure 32 - Are there other health infrastructure support services that collaboration with would increase benefits to First Nations and Inuit?
Figure 32 is a bar chart that illustrates survey responses to the question "Are there other health infrastructure support services that collaboration with would increase benefits to First Nations and Inuit?". Internal (to ISC) responses received were Health Planning and Quality Management (11%); Health Services Integration Fund (14%); Quality Improvement and Accreditation (14%); Health Facilities (19%); eHealth Infostructure (13%); Health Human Resources (14%); and None of the Above (14%). External (to ISC) responses received were Health Planning and Quality Management (15%); Health Services Integration Fund (13%); Quality Improvement and Accreditation (17%); Health Facilities (17%); eHealth Infostructure (11%); Health Human Resources (17%); and None of the Above (9%).
Source: Survey deployed by ISC Evaluation, 2022.
It should be noted that this data is influenced by the programs with which the respondent is involved (i.e., if most respondents are from HPQM, they would select it least as one to collaborate with).
Interviews highlighted that the concept of the Cluster has the potential to work very effectively, however, in practice, program partners perceive that the Cluster programs generally operate in siloes. Overall, partners highlighted that the programs are aligned and therefore there is opportunity to collaborate amongst programs.
It should be noted that, although outside of the evaluation scope period, the Department has implemented significant changes in Fiscal Year 2023-24 to the existing ISC program inventory in order to improve alignment of ISC programs that contribute to similar outcomes. In particular, this realignment has the overall objectives of strengthening performance measurement both at the program and departmental levels and streamlining the Department's programming and activities to improve efficiency.Footnote 116 Under the new proposed structure, the eHealth program will reside under Primary Health Care; HPQM, HSIF, QIAP, HHR and BCT will all reside under Health Systems Support; and HFP will reside with Community Infrastructure. These changes indicate a move in an effective direction; however, the potential benefits of these changes to the program inventory, such as increased effectiveness in cross-collaboration between sub-programs, lie outside of the evaluation scope period.
3.3 Service Transfer
Evaluation Question: Is the departmental goal of service transfer aligned to the needs of First Nations and Inuit?
Finding #19: The goal of service transfer is aligned to the need for autonomy and First Nations-driven health supports, however, there is a need to support capacity development and sustainable funding for long-term planning.
The mandate of ISC is to "work collaboratively with partners to improve access to high quality services for First Nations, Inuit and Métis". The Department's outlined vision is to empower Indigenous peoples to "independently deliver services and address the socio-economic conditions in their communities". As such, one of the key goals of the Department is to achieve successful transfer of services to Indigenous peoples. This report focuses specifically on the transfer of health services to First Nations and Inuit.
In the context of this evaluation, service transferFootnote 117 is defined by ISC as the transfer or shift of control of federally administered programs, policies, and services to First Nations and Inuit-led organizations, supporting self-determination and First Nations and Inuit control in designing, developing, and implementing their own program, services, and policies to address their unique needs and priorities and respect distinct cultural practices.
Given the intent behind service transfer is to improve the quality of health services for First Nations and Inuit, it is vital that consideration is given to whether this goal is aligned to the needs of First Nations and Inuit.
In interviews, it was evident that service transfer is aligned with the identified needs of First Nations to take control of their own services and develop programs that meet their unique health needs. Most First Nations Representatives (77%) and Program Lead (71%) interviews highlighted this alignment, specifically expressing the desire to prioritize their own communities in a way that is not done under federal control and allocate resources towards programs that address the specific needs of their individual communities.
However, it was also highlighted that while the majority of First Nations want services to be devolved, the challenge lies in the level of resources required for a successful transfer. In particular, interviewees noted a lack of sufficient capacity and a severe lack of sustainable funding that is impacting First Nations and Inuit ability to take on services. As a result, there are certain communities that resist transfer at this time, as this will only add burden to already over-capacity health departments.
Many interviewees also indicated that the size of a community is highly relevant to their interest and readiness to take on a transfer of services. A number of interviewees made the distinction between transferring services directly to First Nations, compared to transferring the services to a First Nations-led organization, similar to the FNHA. The latter was expressed as a promising solution to address capacity and expertise gaps that may exist in smaller communities, while still ensuring alignment to First Nations needs. However, in discussions with representatives of First Nations in urban areas, a different perspective was presented. A number of the challenges highlighted in this report are centered around the experiences of First Nations in community. However, there is a large population of First Nations who live outside of communities, in urban centres.
Case Study #8
Giishkaandago'lkwe Health Services (Fort Frances Tribal Health Authority)
Region: Ontario | Program Focus: Health Planning; HSIF
Giishkaandago'lkwe Health Services has had their Environmental Public Health Programming devolved to them, which was supported by HSIF funding.
The Environmental Public Health Program engaged with 10 First Nations in the district to support them in assessing their health and well-being. The program has seven pillars:
- Communicable Disease Control
- Safe Drinking Water
- Healthy Housing
- Waste and Water Management
- Emergency Preparedness and Response
- Food Safety
- Facility Inspections
Since taking over this program, Giishkaandago'lkwe Health Services has hired a water quality analyst and performed water testing and operations, created and enacted policies and procedures related to physical infrastructure work (septic fields, coding, animal bites), and education and community planning efforts to increase awareness and education of their water system.
In discussions with First Nations Representatives and Implementing Partners, it was noted that service transfer presented unique challenges for urban First Nations. Specifically, there was concern expressed that with a complete transfer of services, urban First Nations will no longer benefit from funding towards improving health services as First Nations health care will no longer be under the purview of provincial or federal governments, but instead that of First Nations organizations, whose priorities may lie within on-reserve community members. As such, it is important to consider the implications of service transfer on access to quality health services for all First Nations and Inuit. A more in-depth exploration of the necessary conditions for service transfer and the barriers currently in place are further described in the following sections.
Necessary Conditions for Service Transfer
Throughout this evaluation, partners were asked to share their perspectives on which conditions are required to be in place in a community to achieve a state of readiness for service transfer. Most interviewees agreed that in order to successfully transfer services, First Nations and Inuit require sustainable funding, access to support and training, effective relationships with program partners, most specifically ISC staff, and governance structures. It was also emphasized that the approach to transferring services is key to its potential success.
Effective Relationships and Stakeholder Buy-In
First and foremost, to be able to transfer services effectively, people in First Nations and Inuit communities need to have the capacity to manage the services in the long-term. As such, the transition between current state and a state of transfer requires effective relationships between program partners and First Nations and Inuit to support the building of the necessary capacity.
Interviewees noted a need for openness, cultural awareness and safety, and open-dialogue communication in relationships in order to ensure partners are understanding of the wholistic picture of what elements must be integrated for services to be appropriate for First Nations and Inuit. For a successful relationship, program partners must engage with First Nations and Inuit in a consistent and meaningful way to build trust, gain a better understanding of their identified needs, and support First Nations and Inuit assumption of true control in the allocation of resources. This trust must also be present in fiscal relationships and manifested through less reporting and planning requirements. Interviews emphasized that people in First Nations need the freedom to allocate the provided resources where they see fit.
Case Study #9
Southern Chiefs Organization (SCO)
Region: Manitoba | Program Focus: HSIF
SCO notes that they are in the planning and design phase for the Health Transformation service transfer and when data was collected for this evaluation, they had not actively had any ISC programming devolved to them. SCO calls for increased programming and funding responsibility as it leads the service transfer process. If organizations, including SCO, were not required to compete for funding from the same funding envelope, it is anticipated that an increased ability to deliver large aggregate programming and services to southern First Nations communities throughout Manitoba would be observed.
The system as it currently operates does not support collaboration within the First Nations because often the provincial or federal governments are providing funding to both large organizations to carry out large system change opportunities and smaller entities to do some of that work which causes confusion and challenges about who is leading the work.
Further, it was highlighted that transfer cannot occur solely on the basis of the desire of people in First Nations and Inuit communities, but rather that buy-in from all partners, including the federal government, Provinces/Territories, and other relevant health entities, is required to ensure First Nations and Inuit can access the appropriate resources for capacity building and an effective transition.
It was noted by regional representatives that consideration should be made to the maintenance of key residual roles within ISC Regions to continue to provide support during the transfer of control of services. Engagement with First Nations and Inuit would be required in order to understand and confirm that there is a need for lighter, but continued, support from ISC Regions during the process of service transfer.
Knowledge and Expertise
Another condition necessary for successful service transfer, related to effective relationships, is the knowledge and expertise required within key roles (e.g., health directors, health administrators, management roles, etc.) in First Nations and Inuit communities for the provision of the services being transferred. Interviews highlighted the value of program partners outside of First Nations and Inuit communities who can share their knowledge and expertise and provide the necessary training for areas where capacity may not be as developed.
Similar sentiments were expressed regarding access to resources and information. In order to effectively transfer services, people in First Nations and Inuit communities need to understand what is involved and how best to prepare for service transfer. The expectation, according to interviews, is that ISC should support First Nations and Inuit in obtaining that information. This could include facilitating knowledge sharing, where best practices and lessons learned from ISC and relevant program partners are shared in a consistent and widespread manner to First Nations and Inuit.
Sustainable Funding
Funding is required to build capacity in First Nations and Inuit and ensure patient safety, both from a physical infrastructure perspective (e.g., maintenance of health facilities, appropriate equipment) and a staff perspective (e.g., training and expertise). Only when First Nations and Inuit can confidently plan programs and projects knowing that funding will continue to support these initiatives, with consideration of core health needs, can First Nations and Inuit be in the best state to transfer services.
The importance of investing into infrastructure (i.e., physical, technological, governance etc.) in order to achieve service transfer was noted several times across stakeholder groups, with one internal stakeholder specifying that a large proportion of their success thus far is due to expenditures in the infrastructure space. Infrastructure is a foundational piece to the ability of First Nations and Inuit to provide adequate and safe care and is considered a necessary condition for service transfer.
Governance Structures
Another necessary condition that was noted frequently amongst various stakeholder groups was that of an appropriate governance structure in place.
Service transfer is more than a simple transfer of funding control to First Nations and Inuit; rather, it needs to be a transfer of ownership of programs and services. Interviewees noted the need for appropriate governance structures with two-way accountability (i.e., accountability of ISC and accountability of First Nations and Inuit) in order to ensure resources are allocated efficiently and effectively to achieve objectives of First Nations and Inuit programs and services. According to interviews, it is imperative that accountability and reporting frameworks be defined and developed in partnership with First Nations and Inuit. The value of strong governance lies in the ability to provide oversight over programs and services through clearly defined processes and procedures, roles and responsibilities, and intended outcomes, as well as defined indicators to measure performance against those outcomes. Having these systems in place allows for improved knowledge sharing, increased standard of quality, and a greater understanding of strengths and weaknesses to drive strategic planning.
In discussions with representatives from the FNHA, it was specifically noted that the governance structures in place, including formal reporting mechanisms (financial and narrative reporting), participation in partnership tables, and informal communication channels between key partners are instrumental in their continued success. Other governance-related conditions that can also facilitate successful service transfer include defined policies and procedures, data governance strategies, and change management plans.
This condition links back to the value stated by program partners of pursuing accreditation, given that when accredited, institutions are considered capable of running health systems in alignment to a set of clearly defined, approved, and accepted standards. With many of these governance pieces already in place through accreditation, QIAP partners noted that service transfer occurs more smoothly as a result.
Case Study #10
Onion Lake First Nation
Region: Saskatchewan and Alberta | Program Focus: HSIF
Onion Lake took over full control of community health programming, some non-insured health programs and services, and ambulatory care. The Nation negotiated with the Province of Saskatchewan to establish a dedicated ambulance service for their community members. The Nation has also negotiated with previous regional health authorities before they were disbanded to form the one remaining Saskatchewan Health Authority, allowing the services to be negotiated at the provincial level.
Community health programming that is delivered by Onion Lake includes pre-and-post-natal care, x-ray medical imaging, a pharmacy, and a clinic department staffed with doctors and nurse practitioners. These initiatives have been supported in part by the Health Services Integration Fund. The Nation is currently developing their own health care system for primary health care delivery.
Approach to Transfer
Above, it was noted that while the intent behind service transfer is aligned to the needs of First Nations, there were concerns around the approach to transferring services. Specially, interviewees noted the need to engage with First Nations to understand which services they are willing and currently capable of assuming full control over in order to better focus on building capacity in those areas.
It was also highlighted by a select number of internal partners that the objective does not always have to be an immediate and full transfer of service. There is value to the small victories (i.e., small-scale transfer) that can contribute to a greater transformation of health services. However, this was somewhat contradicted in other interviews, where it was noted that the disjointed nature of small-scale transfer can create siloes and potential strategic misalignment when broader Health Transformation is the eventual goal.
Despite the inconsistent perspectives from interviews, what was clear was the importance of considering the approach to transfer in order to properly understand its potential success or pitfalls. If small-scale, project-based transfer is the best way forward for some First Nations and Inuit, there should be appropriate consideration made to how this can be accomplished and what the implications will be for other related projects, entities, and partners. More broadly, to contribute to successful service transfer, regardless of the scale, efforts should be put towards ensuring the necessary conditions for service transfer outlined in this section are in place.
Potential Barriers to Service Transfer
Insufficient Funding
According to the majority of interviewees (45%), the most prevalent barrier to service transfer is the absence of sustainable funding. First Nations and Inuit are sometimes deterred from taking control of services due to the lack of access to sufficient funding that can maintain the services in the long-term.
Throughout interviews, it was emphasized that the lack of funding towards the Cluster programs, and subsequently the people in First Nations and Inuit communities they serve, is insufficient to achieve the objective of the individual programs and by extension, the broader Departmental goal of service transfer.Footnote 118
Due to insufficient levels of funding, First Nations and Inuit are unable to adequately address all areas of greatest need. When considering the social determinants of health, infrastructure needs, and emergency health services, it is often difficult to decide which area is of greater priority, particularly when faced with limited financial resources to support all areas of need. On the one hand, emergency services are required to address current crises; however, on the other hand, addressing root challenges, such as social determinants of health, is necessary to reduce and/or prevent the number of health emergencies occurring.
A select number of interviewees (6%) also noted the absence of comprehensive health care, as some health care staff may be funded through various avenues (e.g., doctors could be funded by both the federal government and provincial government, nurses could be federal employees, and other health care staff may be directly from community). The challenge of having multiple jurisdictions providing health care services on reserve can result in a lack of integrated care, particularly when roles and responsibilities are not clearly defined and overarching policies and procedures (e.g., sharing patient data and information between various parts of a health care system or between different types of health care working) are not in place to guide overall health care service delivery in communities. Therefore, sufficient funding is required not only to meet the broad range of needs of First Nations and Inuit, but to also support greater integration of health care services, an aspect that is HSIF's primary objective.
ISC Staff Turnover
As noted above in Finding #16, according to interviews, the level of turnover in staff at ISC has created barriers to the ability of people in First Nations communities to build relationships and access support in key areas. For example, one First Nations Representative mentioned that they were receiving support for data analysis and access from ISC regional staff; however, when the ISC representative changed positions, the First Nation was no longer able to receive that support. The constant need to rebuild relationships erodes at the trust that First Nations and Inuit have in the ability to make progress and remain aligned with ISC in a common path towards eventual service transfer.
Various Stages of Readiness
With regards to small "t" transfer, one area that was highlighted often throughout interviews was the challenge that stems from the different sizes of communities as well as the various stages of readiness they can be in for service transfer. With regards to big "T" transfer, fully transferring health programs and services to an entire region or province may be difficult to accomplish when all communities in that region are not yet equipped to take on services, or if there is limited capacity of a representative First Nations or Inuit-led governance body who will deliver the services.
It was noted by select program representatives that it is important to recognize that people in First Nations and Inuit communities may require varying levels of support in delivering services, given that some communities are already operating independently while others may be able to take on some services but not all. Overall, there is a need to support capacity building within communities to improve broader readiness for transfer. However, the challenge still remains that service transfer is not a one-size-fits-all approach, and flexibility is required to meet the unique needs of First Nations and Inuit when approaching service transfer. It should also be emphasized that the programs and services that are to be eventually transferred to First Nations and Inuit must themselves be in an appropriate state of readiness for transfer (e.g., they are sufficiently funded, governance mechanisms are established, mechanisms for knowledge sharing and transfer are established, etc.). It is important for ISC to work towards achieving a level of readiness in their health programs and services to ensure First Nations and Inuit are not faced with the additional burden of 'rehabilitating' programs and services before they are able to fully assume control over them.
Evaluation Question: How have the programs in the Cluster worked towards ensuring the eventual transfer of departmental responsibilities to First Nations and Inuit?
In Finding #19, this report assessed the level of alignment between the Department's goal of service transfer to the health needs of First Nations and Inuit. Through interviews, it was determined that the overarching objective of transferring control over key health services to communities was very aligned with their needs; however, the way in which this transfer would be accomplished is key to both the alignment and the sustainability of the services post-transfer. Taking these findings into consideration, this section explores the role the Cluster programs have and continue to play in building the necessary capacity in communities to take over services and ensure the eventual transfer of departmental responsibilities to First Nations and Inuit.
Finding #20: Each program in the Cluster contributes to the building of capacity to facilitate service transfer. While the Cluster programs have made progress towards achieving their respective intended immediate outcomes, there are significant gaps in the sustainability required to produce long-term systemic results.
Through interviews, this evaluation examined the extent to which the Cluster programs contribute to systemic change in how the federal government delivers health services to First Nations and Inuit. Considering the Department's mandate of service transfer and the way in which devolution of services would impact the delivery of health services to First Nations and Inuit, this section sought to further assess whether the programs are working together effectively to achieve this objective.
Interviewees had varied perceptions of the Cluster's role in service transfer and creating systemic change. Interviews highlighted that the ultimate outcome of the Cluster is for these programs to be under Indigenous institution control and design. This, according to interviews, requires a shift from the commonly existing mindset of national programming towards an understanding of the potential localization required to meet the needs of each region or nation. Program partners emphasized the importance of not further embedding programs into the federal system by ensuring that decision-making is in the hands of First Nations and Inuit.
When asked to share their perception that First Nations and Inuit are being treated as equal partners in health services, most survey respondents responded positively; however, 15% of external respondents were neutral and 19% of external respondents indicating further room for improvement. It is also worth noting that while both groups responded positively, internal respondents were much quicker to indicate they 'strongly agreed' that they were equal partners than external respondents. This is indicative of a misalignment of perception where First Nations and Inuit feel less like equal partners than internal partners believe they do. Based on information gathered through interviews and surveys, the evaluation noted that it can be challenging for First Nations and Inuit to feel like equal partners due to many of the barriers and challenges noted in previous findings, such as insufficient funding and a lack of capacity building support.
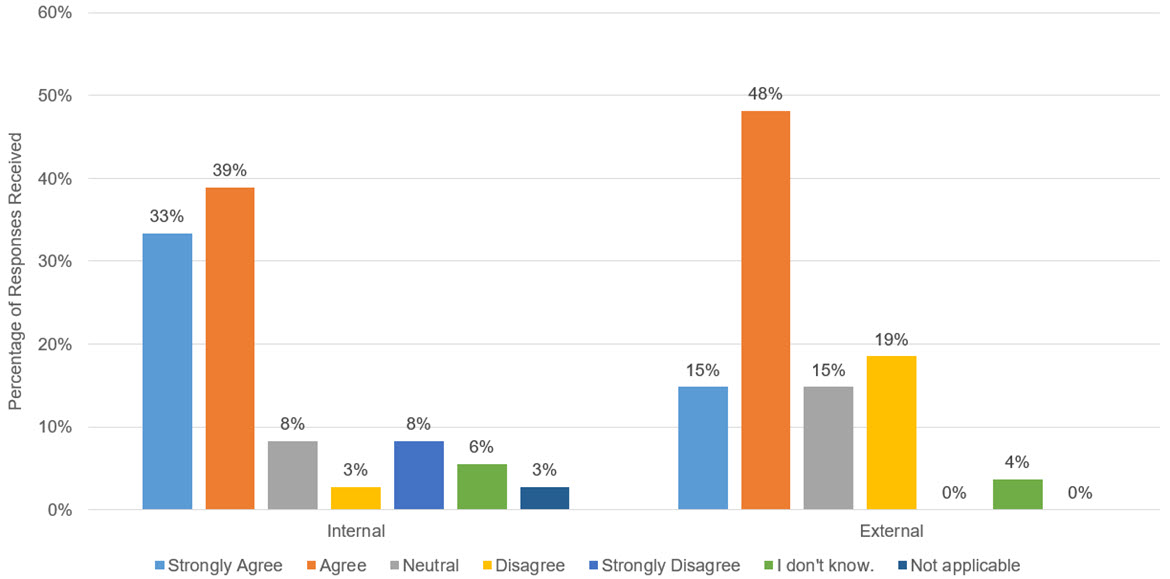
Text alternative for Figure 33 - First Nations and Inuit who access health infrastructure are equal partners in planning, developing, and monitoring to make sure it meets their needs and to achieve the best outcomes
Figure 33 is a bar chart that illustrates survey responses to the statement "First Nations and Inuit who access health infrastructure are equal partners in planning, developing, and monitoring to make sure it meets their needs and to achieve the best outcomes". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (33%), Agree (39%), Neutral (8%), Disagree (3%), Strongly Disagree (8%), I don't know (6%), and Not Applicable (3%). External (to ISC) responses were Strongly Agree (15%), Agree (48%), Neutral (15%), Disagree (19%), Strongly Disagree (0%), I don't know (4%), and Not Applicable (0%).
Source: Survey deployed by ISC Evaluation, 2022.
When asked specifically about their perception of the Cluster programs' collaboration to achieve service transfer, again responses varied, particularly depending on the specific program. Interviewees noted that there are opportunities for the programs to collaborate; however, there is minimal funding available to support sustainable planning in a wholistic manner across programs. The lack of sustainability suggests an inability to make lasting systemic changes. Please refer above to Finding #18 for additional details about opportunities to improve collaboration between Cluster programs.
Despite these challenges, it is important to note that the Cluster programs have achieved successful small-scale transfer of services in several communities by building capacity within those communities and continuing to provide support where needed. Interviews emphasized the relationship between building capacity in communities through health planning, participation in the Accreditation program, hiring community-based culturally and medically competent staff, maintaining safe health facilities in which to provide services, and building technological infrastructure to improve access to and quality of care. The Cluster programs are all focused on building the base elements required to bring First Nations and Inuit health services up to par to Canadian national standards as well as ensuring First Nations and Inuit have the support needed to make their health care systems safe and accessible. Interviewees also noted a current focus on building meaningful partnerships and relationships as opposed to achieving full-scale transfer. Regional representatives highlighted that they work with many organizations, committees, and nations to engage First Nations and Inuit in the design and delivery of services.
3.4 Efficiency
Evaluation Question: How cost effective is the design and delivery of the programs included in this health infrastructure cluster?
a. Are there ways to make them more cost effective?
b. Is the allocation of funding to and within each of the programs appropriate to achieve the expected outcomes?
Finding #21: The current level of funding is insufficient and unsustainable to support programs in the achievement of their intended objectives.
Most partners (74%) consulted throughout this evaluation highlighted a severe lack of funding to Cluster programs, and by extension, to people in First Nations and Inuit communities, to address health inequities and achieve intended program objectives. As noted in Finding #7 and more broadly in the Effectiveness section above, the Cluster programs have been able to make progress towards their intended objectives over the evaluation period; however, the breadth of the Cluster programs' impact was impeded by the lack of financial and human resources available. The following section describes some of the primary challenges related to the Cluster programs' funding levels.

Text alternative for Figure 34 - Program Annual Expenditures
Figure 34 is a line chart that illustrates program data representing the annual expenditures of each program within the Cluster for fiscal years 2015/16 through 2020/21. HPQM's program expenditures were $108,307,251.73 (2015/16), $111,311,407.76 (2016/17), $116,762,360.46 (2017/18), $132,531,552.65 (2018/19), $125,635,240.19 (2019/20), and $131,437,338.96 (2020/21). HSIF's program expenditures were $8,061,748.85 (2015/16), $19,586,573.25 (2016/17), $14,498,899.77 (2017/18), $37,661,336.53 (2018/19), $41,355,706.69 (2019/20), $40,365,229.49 (2020/21). Accreditation's program expenditures were $5,203,010.00 (2015/16), $5,329,828.00 (2016/17), $5,598,299.00 (2017/18), $6,333,099.00 (2018/2019), $5,684,666.00 (2019/2020), $6,143,294.10 (2020/21). HFP's program expenditures were $89,444,707.37 (2016/16), $167,948,252.00 (2016/17), $197,348,222.00 (2017/18), $172,439,142.63 (2018/19), $148,278,065.87 (2019/20), $149,189,767.62 (2020/21). eHealth's program expenditures were $24,367,982.00 (2015/16), $25,910,204.00 (2016/17), $26,874,347.00 (2017/18), $25,725,674.00 (2018/19), $28,038,392.55 (2019/20), $30,889,468.02 (2020/21). HHR's program expenditures were $5,651,730.26 (2015/16), $8,796,363.60 (2016/17), $5,808,989.19 (2017/18), $5,901,976.63 (2018/19), $2,722,648.94 (2019/20), $2,722,648.94 (2020/21).
Source: ISC Financial Records, retrieved 2023.
Throughout interviews, partners noted the lack of consideration made to changes in the economic state, particularly inflation, in funding allocations. Inflation results in a higher cost of living (COL) and a higher cost of materials, both of which impact the available resources to effectively address health needs (e.g., increase required salaries, price of equipment, etc.). This was made further evident in the evaluation's review of program expenditures over the period of the evaluation. As demonstrated in the graph above, funding levels for the Cluster programs have largely remained stagnant over the last six years.Footnote 119
In addition to the overall lack of increase funding to the Cluster programs year over year, the following program-specific challenges were noted:
HFP
In discussions with program representatives of the HFP, interviewees noted varying funding sources that have been allocated to support the program in more recent years, including from the 2021 Canada Human Rights Tribunal (CHRT) 41 Order, which outlines orders for Canada to provide funding towards the purchase and construction of capital assets for the delivery of First Nations child and family services and services associated with Jordan's Principle.Footnote 120Footnote 121 Further, it was noted that funding is received under the Indigenous Early Learning and Child Care (IELCC) Framework that is allocated towards minor capital projects. However, HFP partners highlighted the lack of sufficient consideration of changes in costs of construction and noted that the current economic state has not accurately been reflected in the program's annual funding allocations.
A significant (45%) number of interviewees emphasized the impact of unsustainable funding, with particular focus on the inability to invest in operations and maintenance activities. According to interviews, the majority of funding received under HFP is allocated towards capital projects, including minor repairs and major construction projects, with little available to allocate towards sustaining facilities over the long-term.
HSIF
Similar to the HFP, both internal and external partners noted a challenge with the sustainability of HSIF funding. For example, applicants submit proposals to access funding through HSIF. However, the funding is time-limited, meaning that people in First Nations and Inuit communities are required to use resources to regularly develop proposals to access additional funding for the purpose of continuing to make progress in achieving their intended objectives and meeting their respective community's needs. This also affects the ability of First Nations and Inuit to effectively plan for the long term, as it is only with sustainable funding that community-led projects and initiatives can be maintained and provide benefits for First Nations and Inuit over a longer time horizon.
HPQM
In interviews, it was noted by a select number of partners that HPQM funding is sometimes used as an incentive for First Nations and Inuit who have taken on greater control of health services. This results in less funding and resources being allocated to First Nations and Inuit who lack the capacity to develop a health plan. This poses a unique challenge as the communities who do not have a health plan in place or who may not exercise great amounts of control over their health service delivery are often the ones who are in greatest need of funding support for health planning activities in order to build a stronger foundation on which to deliver health services that meet the unique needs of their respective communities.
QIAP
The funding amount for the Quality Improvement and Accreditation Program in Budget 2018 was $22.5M across 2018-2021, with an ongoing $4.5M.Footnote 122 QIAP partners outlined that no new funding was received since 2017/2018, when funding to the Accreditation program was cut by 75%. A significant number of partners (43%) and most Program Leads (71%) highlighted that funding does not adequately support the QIAP or HPQM programs. Despite noted success, Program Leads shared that they have halted marketing and awareness efforts as the lack of funding results in an inability to meet the rising demand for accreditation activities.
HHR
While there are many health needs associated with HHR, funding for the program is not permitted to be allocated towards broader training areas, including: continuing education for regulated health professionals, curriculum development or modification, wages/salaries of community-based workers, and staff replacement costs to attend training.Footnote 123 Interviews with First Nations representatives noted that supporting these areas would be beneficial for First Nations in meeting their health human resource needs. Despite this, and similar to the QIAP, there continues to be a high demand for this program. However, due to limited program funding allocations, the HHR program has only been able to meet approximately 50% of the demand.
eHealth
Partners involved with the eHealth program emphasized that the funding levels available to allocate to First Nations are insufficient in the face of long-term and continuous expenses related to eHealth technologies. Interviewees noted that First Nations are often required to provide their own funds to be able to maintain implemented systems (i.e., EMR), despite having very limited resources to do so. Program partners highlighted that while there have been success stories in which First Nations have been able to successfully secure additional funding or self-fund maintenance activities, First Nations should not be required to be responsible for these costs, particularly when there are often many other critical health needs that First Nations are seeking to address.
It was further noted that access to funding can fluctuate as a result of changes in leadership roles, including political parties. Partners shared examples of making progress under one leader that is then diverted when the position is transitioned, demonstrating a variance in priorities and perspectives.
In addition to the program-specific funding challenges noted above, the following areas were also noted more broadly by interviewees as challenges:
- Cultural safety and humility: As aforementioned, allocating funding towards increasing access to a health facility or health services is not enough. People in First Nations and Inuit communities need to have access to culturally safe care in order to be comfortable seeking and receiving services. In interviews, it was noted by a select number of partners that even when adequate levels of funding for program activities are allocated, they often do not consider the additional activities required to integrate cultural or traditional practices in broader service delivery. Other program partners noted inadequate levels of funding to ensure requirements are met for culturally safe and quality care, such as occupational health and safety requirements and patient navigators.
- Needs-based funding: Based on a review of the standard terms and conditions for ISC transfer payments under the Health Infrastructure Support Authority (i.e., the program authority under which the Cluster programs fall within), funding recipients are allocated funding based on the conduct of a readiness assessment, including a General Assessment that is conducted to develop a risk profile for recipients which outlines expectations around the level of monitoring required, the type of plan expected, and the appropriate funding model to select. Funding is provided through one of four funding models, including:
- Set: Funding agreement with the least amount of flexibility where recipients deliver programs and services as set out by FNIHB. Recipients can only reallocate funds within the same budget activity with written approval by the Minister within the fiscal year reporting period.
- Fixed: Allows for funding to be reallocated to other functional areas within the same budget activity. Unexpended funding can only be carried forward to the next fiscal year to complete activities that had already been initiated.
- Flexible: The recipient establishes a multi-year work plan that includes a health management structure, priorities, objectives, activities, and a budgetary plan. Recipients are able to carry over program funding annually for the duration of the agreement, although any unspent funds at the end of the agreement must be returned.
- Block: The recipient establishes a health plan that includes a health management structure, priorities, objectives, activities, reporting requirements, and health programs and services. Recipients are able to reallocate funds across authorities and can retain any surpluses to reinvest in health priorities.
Funding is provided to support the development of these plans on the basis of estimates provided by the respective regions. It was noted by one stakeholder that in block agreements, population numbers are used to allocate funding amounts; however, when the agreement is being renewed, there is no opportunity to adjust the agreement amount to reflect a larger population or any new needs that have arisen. Further, they highlighted that population calculations often do not account for those who live off-reserve but still use services provided by First Nations.
There is a perception amongst partners that the allocation of funding can be improved to increase effectiveness of dollars. Particularly, it was noted that funding should be allocated on a needs-basis, rather than based on a per-capita formula. Interviewees emphasized that needs are not uniform across First Nations, and as such, one community may require a higher proportion of funding towards one particular health area, while another may not need as much in that same area but need more in yet another. Provincial governments may indicate certain overarching needs, for which funding is then secured and distributed based on population sizes, leaving First Nations to plan on the basis of what is received. Throughout interviews, a significant number of program representatives (43%) noted that the existing funding allocation formulas are not appropriate for the accurate measurement of need, as they tend to focus on metrics, such as population size, that are not always indicative of relevant health needs. Interviewees noted that this is not beneficial to allowing First Nations to highlight the core needs for which they require funding, nor is population size always indicative of greatest level of need.
Of note, the HFP introduced a needs-based prioritization framework during the evaluation period. Program representatives noted that previously, there was a challenge in the prioritization of funding, which historically resulted in allocation of funding towards communities who are ready but not the ones who exhibit the greatest needs, which is not necessarily accurate. To overcome this challenge, the program put in place a needs assessment framework with the purpose of implementing a more consistent process for evaluating, costing, and prioritizing major capital investments. The framework allows the program to better direct investments towards communities and projects of greatest need (e.g., projects that address life, health, and safety needs are designated as high priority).Footnote 124 There may be an opportunity for the other Cluster programs to share best practices, lessons learned, and knowledge with the HFP's approach to determine if there are aspects that can be adopted into their respective funding formulas to support needs-based funding allocations.
Case Study #11
Giishkaandago'lkwe Health Services (Fort Frances Tribal Area Health Services)
Region: Ontario | Program Focus: Health Planning; HSIF; HFP; eHealth
A lack of sustainable and long-term funding support presents many challenges for organizations. Some of these challenges were experienced by Giishkaandago'lkwe Health Services. A lack of permanent, adequate, physical office space poses many challenges related to supporting employees with adequate workspace, hosting Chiefs and other community members on-site, having a reliable space for storage, and collaboration with team members.
Decreasing funding has severely pressured the organization's operational budgets, whereby they experience difficulties in not only offering competitive wages to recruit and retain healthcare talent, but also a lack of long-term sustainable funding means that the organization is constantly being tasked with offering term positions and unstable employment for key functions of their operations, including payroll clerks.
Giishkaandago'lkwe had their nursing program and environmental health programs devolved to them. However, there have been major challenges associated with the lack of timeliness of annual funding along with the administrative burden of annually reapplying for funding. Additionally, the repositioning and/or adaptation of programming that is required to reapply for additional funding for a program that received funding in previous also contributed to the increase in administrative burden for the organization.
Overall, the cost-effectiveness and the Cluster's impact on outcomes could be improved if health infrastructure support programs were better supported. For example, accredited health centres have demonstrated efficiencies in overall program delivery, reducing costs and equipping health centres and First Nations with the right tools to address health needs in an efficient and effective manner. Additionally, and of note, the Evaluation of the BC Tripartite Framework Agreement on First Nations Health Governance (2019) emphasized that the FNHA's strategic position and partnerships with both the federal and provincial governments facilitated new investments from both levels of governments to support the transfer of FNIHB services to the FNHA. In particular, sufficiency of funding, both in magnitude and timeframe, are required to support a smoother process of service transfer.
The Cluster programs have continued to make progress towards the achievement of their respective intended outcomes despite limited increases to overall funding levels. However, the Cluster programs would be able to make more significant progress towards their objectives if there was sufficient funding to support doing so.
Finding #22: The level of human resources and the type of staff available to programs and First Nations is not sufficient to deliver the required health support services to First Nations.
A review of program data highlighted the annual number of FTE staff working in regions per Cluster program over the evaluation period.Footnote 125
Please note, after publication of this report, issues with FTE data reported for eHealth program were noted. This revised report has updated information related to eHealth and Quebec regional staff.
| Cluster Programs | Program FTEs and Year Over Year Percentage Change | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fiscal Year 2016/17 | Percentage Change | Fiscal Year 2017/18 | Percentage Change | Fiscal Year 2018/19 | Percentage Change | Fiscal Year 2019/20 | Percentage Change | Fiscal Year 2020/21 | Percentage Change | |
| HPQM | 35.64 | 10% | 30.61 | -14% | 23.00 | -25% | 27.60 | 20% | 32.20 | 17% |
| HSIF | 5.82 | -26% | 5.87 | 1% | 3.17 | -46% | 2.45 | -23% | 2.76 | 13% |
| QI&A | 8.36 | 18% | 4.00 | -52% | 2.35 | -41% | 3.22 | 37% | 5.00 | 55% |
| Health Facilities | Not applicable | Not applicable | Not applicable | Not applicable | 48.08 | Not applicable | 48.94 | 2% | 57.39 | 17% |
| eHealth | 27.58 | 0% | 22.88 | -17% | 20.69 | -10% | 22.21 | 7% | 24.46 | 10% |
| HHR | 1.50 | -6% | 0.02 | -99% | 0.31 | 1,724% | 0.31 | -100% | 0.00 | 0% |

Text alternative for Figure 35 - Number of Program FTEs by Cluster Program Fiscal Year 2015-16 to Fiscal Year 2020-21
Figure 35 is a bar chart that illustrates program data representing the Number of Program FTEs by Cluster Program for the fiscal years 2015-16 through 2020-21. FTEs for HPQM were 32.34 (2015/16), 35.64 (2016/17), 30.61 (2017/18), 23 (2018/19), 27.6 (2019/20), 32.2 (2020/21). FTEs for HSIF were 7.85 (2015/16), 5.82 (2016/17), 5.87 (2017/18), 3.17 (2018/19), 2.45 (2019/20), 2.76 (2020/21). FTEs for QIAP were 7.09 (2015/16), 8.36 (2016/17), 4 (2017/18), 2.35 (2018/19), 3.22 (2019/20), 5 (2020/21). FTEs for HFP were not applicable (2015/16), not applicable (2016/17), not applicable (2017/18), 48.08 (2018/19), 48.94 (2019/20), 57.39 (2020/21). FTEs for HHR were 1.6 (2015/16), 1.5 (2016/17), 0 (2017/18), 0.31 (2018/19), 0 (2019/20), 0 (2020/21). FTEs for eHealth were 27.66 (2015/16), 27.58 (2016/17), 22.88 (2017/18), 20.69 (2018/19), 22.21 (2019/20), 24.46 (2020/21).
Source: ISC Human Resources Program Data, retrieved 2024.
Throughout the evaluation period, the overall number of FTEs in the Cluster as a whole has increased by 59% since FY2015-16. However, when the data is broken down by program, it indicates significant variances of staff levels year over. This includes, most notably, the Health Facilities program, which has increased its number of FTEs by 19% since FY2018-19, while Health Human Resources has decreased by 100%.
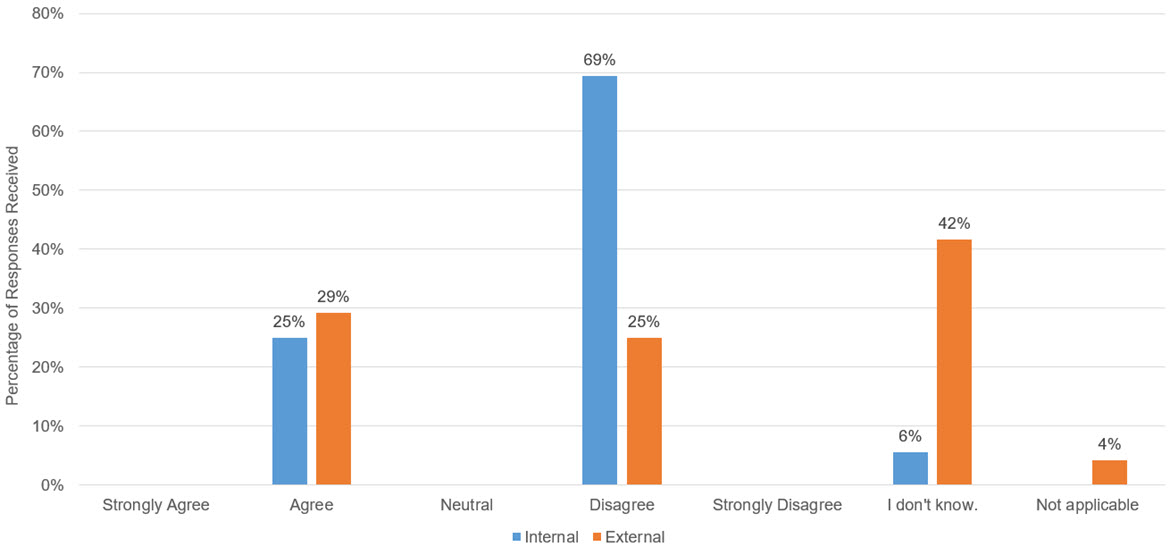
Text alternative for Figure 36 - Staffing is adequate in ISC Regional Offices to support health service(s) delivery
Figure 36 is a bar chart that illustrates survey responses to the statement "Staffing is adequate in ISC Regional Offices to support health service(s) delivery". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (0%), Agree (25%), Neutral (0%), Disagree (69%), Strongly Disagree (0%), I don't know (6%), and Not Applicable (0%). External (to ISC) responses were Strongly Agree (0%), Agree (29%), Neutral (0%), Disagree (25%), Strongly Disagree (0%), I don't know (42%), and Not Applicable (4%).
Source: Survey deployed by ISC Evaluation, 2022.
In order to understand the gap more clearly, both internal and external survey respondents were asked to indicate whether staffing was adequate in ISC regional offices, as well as directly in First Nations communities.
In alignment with the program data, internal respondents generally Disagreed (69%) that was adequate in ISC regions, while a smaller portion indicated that they Agreed (25%). External stakeholder responses were more varied, with 42% indicating that they did not know, 29% Agreed, and 25% Disagreed.
When asked the same questions regarding staffing within communities, both internal and external respondents were aligned in their responses; they Disagreed (67% and 63%, respectively). For internal respondents, the next most common response was 'I don't know' while for external respondents, it was 'Agreed'.Footnote 127
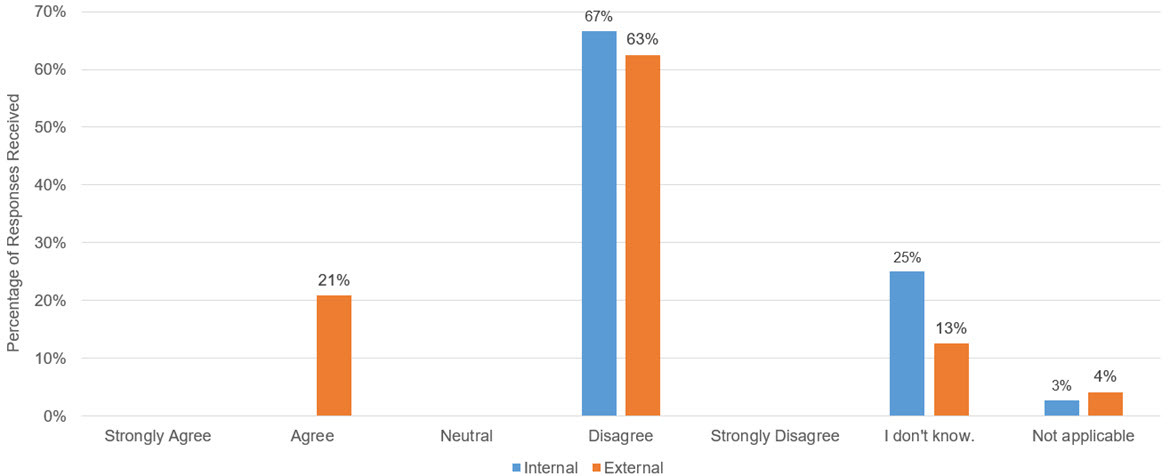
Text alternative for Figure 38 - Staffing is adequate in First Nations and Inuit communities to support health service(s) delivery
Figure 38 is a bar chart representing survey data that illustrates responses to the statement "Staffing is adequate in First Nations and Inuit communities to support health service(s) delivery". Responses were on a scale and include Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree, I don't know, and Not Applicable. Internal (to ISC) responses were Strongly Agree (0%), Agree (0%), Neutral (0%), Disagree (67%), Strongly Disagree (0%), I don't know (13%), and Not Applicable (4%). External (to ISC) responses were Strongly Agree (0%), Agree (21%), Neutral (0%), Disagree (63%), Strongly Disagree (0%), I don't know (13%), and Not Applicable (4%).
Source: Survey deployed by ISC Evaluation, 2022.
Interviews with First Nations representatives highlighted challenges faced in achieving adequate staffing (58%), including, most prominently, the lack of funding available to hire and retain staff. This was noted in all areas of health human resources, including frontline healthcare providers and health administration and management staff.
In the survey, respondents were asked to elaborate on what types of human resources would be required to adequately provide the services intended by the Cluster programs. Respondents highlighted the follow resource needs:
- Registered Nurses (RN)
- Home & Community Care (H&CC) Nursing Services
- Mental Health Support Workers
- Program Coordinators
- Specialized Health workers
- Doctors
- Data Analysts/Health Informatics
- IT & Cybersecurity Professionals
- Digital Health/EMR Systems Support
- Database and Health Administrators
- Receptionists/Intake Clerks
- Finance Professionals
- HR/Personnel Managers
- Training Managers
- Cultural Supports
- Patient Safety Professionals
Interviewees emphasized that the human resources required to address health infrastructure gaps extend beyond direct health care providers (i.e., nurses, doctors, etc.); they span across many skillsets and capabilities that are needed to sustain a wholistic health ecosystem.
Throughout interviews, partners emphasized the lack of capacity and shortage of labour in communities, highlighting that it is not uncommon for only one or two staff members being responsible for running a community’s entire health department.
Case Study #12
Southern Chiefs Organization (SCO)
Region: Manitoba | Program Focus: HSIF
SCO notes how the pandemic highlighted how little support was available in community and how the need for immediate on-the-ground response highlighted the presence of these gaps for provincial and federal governments. Some of these gaps included having enough staff to respond to the pandemic and having the physical space and infrastructure to appropriately store vaccines.
In order to provide aid services as efficiently as possible, SCO enacted an "all-hands-on-deck" approach whereby many staff members were repurposed to support with COVID-19 response measures. First Nations in Manitoba were praised for their response to COVID-19 and were often referred to as the regional center for aid efforts, including for their ability to vaccinate their communities and non-Indigenous individuals who work in communities represented by SCO.
Finding #23: While there are no closely comparable health 'clusters', best practices in improving the quality and access of health services for Indigenous peoples were highlighted in both interviews and literature review. This includes cultivating respectful and longstanding relationships, reducing siloes, and supporting First Nations and Inuit data sovereignty.
The evaluation conducted external research about frameworks, programs, and initiatives with similar objectives and target populations to the Cluster to assess best practices and lessons learned in the Cluster's design or delivery strategies. Based on literature review and further supplemented by interviews, the following initiatives were highlighted:
First Nations Health Authority in BC
Although the BC Tripartite Relations program was not formally evaluated as part of this Cluster evaluation, it was included with the intent to learn from its design and delivery model and glean best practices and lessons learned.
The transfer of health services and programming from FNIHB – BC Region to the FNHA is broadly seen as successful and noted through both interviews and literature review as a model for service transfer. The recently conducted Evaluation of the BC Tripartite Framework Agreement on First Nation Health Governance highlighted several factors that contributed to the success of the transfer, including:
- Strong partnerships between First Nations in BC, the FNHA, the federal government and the provincial government, including a high level of collaboration.
- Commitments from all parties towards cultural safety and humility, the 7 DirectivesFootnote 128, and the Vision and principles of the Framework Agreement.
- Flexibility in the approach to achieving successful service transfer.
- Dedicated and sufficient funding for various aspects of service transfer, such as dedicated funding for community engagement activities or for information management/information technology systems development and maintenance.
Key lessons learned in the transfer of health services of programming to the FNHA were highlighted in both the previously conducted evaluation and in interviews with program partners. They included the following:
- Service transfer does not occur overnight. The process and transition can take a long period of time to ensure all aspects of a successful service transfer have been considered, implemented, and matured (e.g., IM/IT systems, governance and organizational structures, etc.).
- Integration of various jurisdictions and levels of government is necessary for successful service transfer. In particular, there must be authentic buy-in from all key partners as well as clearly defined responsibilities and accountabilities that are actively committed to.
- The long-term sustainability of funding and resources is required to ensure service transfer can continue to be successful for years to come. Long-term planning efforts are required at various levels of community and government to better support the sustainability of health programs and services.
- Robust health-related data is required to support First Nations in advocating for targeted funding based on their needs and priorities.
Overall, the transfer to the FNHA was considered successful due to a variety of reasons. The two primary ones highlighted in the previously conducted evaluation and the interviews were the following: Firstly, it has allowed First Nations in BC to create a First Nations governance structure. It is through the emphasis on the importance of First Nations governance that allows First Nations in BC to be self-determining in the area of health services. A clearly established First Nations governance structure has also allowed for increased access to both federal and provincial funding in the area of health services. Secondly, the high degree of commitment from all levels of government was considered a great success, as it allowed a smoother process of service transfer in BC while remaining flexible and adaptable to the needs of BC First Nations. The relationships between the FNHA, BC First Nations, and various levels of government have been improved and there is a degree of trust that has been established.
National Aboriginal and Torres Strait Islander Health Plan (NATSIHP)
Australia's federal government developed the National Aboriginal and Torres Strait Islander Health Plan (NATSIHP) in partnership with Aboriginal and Torres Strait Islander peoples with the goal of achieving better health outcomes through the prioritization of community-controlled health services.
The plan emphasizes the importance of addressing the social and environmental factors that affect Indigenous health, ensuring health care delivery is culturally safe for Indigenous peoples, and achieving equality of health status and life expectancy between Aboriginal and Torres Strait Island people and non-Indigenous Australians by 2031.Footnote 129 The NATSIHP and its intended outcomes were developed to complement the National Agreement on Closing the Gap (the National Agreement), which was developed to address the inequalities experienced by Aboriginal and Torres Strait Islander people.
An Implementation Plan was developed to define the Australian Government's role in executing the NATSIHP. It set out twenty goals, including goals such as increasing the proportion of Aboriginal and Torres Strait Islander women attending at least one antenatal visit in the first trimester in their pregnancy, increasing the rate of Aboriginal and Torres Strait Islander children who have at least one annual health check, and reducing the rate of Aboriginal and Torres Strait Islander youth who smoke. The Implementation Plan also defined indicators for each goal, as well as historical data, data sources, projections, and any potential limitations.Footnote 130 The Australian Government considers the achievement of these twenty goals as success of the NATSIHP; however, it is also important to note that there were a series of strategies defined in the Implementation Plan that underpin the NATSIHP and its overall objective. These strategies can be considered as best practices for when federal governments are seeking to partner with Indigenous peoples when addressing health inequities, and include, but are not limited to:
- Meaningful partnership and engagement with Aboriginal and Torres Strait Islander peoples, including their representative bodies, throughout all aspects of the NATSIHP and its Implementation Plan, including planning, service delivery, and evaluation.
- Dedicated investments to build the capacity and capability of Aboriginal Community Controlled Health Organizations (ACCHOs) to ensure identified needs of Aboriginal and Torres Strait Islander peoples are met.
- Addressing social and cultural determinants of health, including improving school attendance and workforce participation as well as building safe communities.
- Establishing clear partnerships and accountability mechanisms, including assessing progress and performance of the plan on a regular basis.Footnote 131
New Zealand Māori Health Strategy – He Korowai Oranga
He Korowai Oranga focuses on a wholistic vision of Māori health. The strategy was first published in 2002 and is intended to provide an overarching framework for the federal government and the health and disability sector more broadly in New Zealand to achieve pae ora – or healthy futures for Māori. It was subsequently revised in 2014. Whakamaua: Māori Health Action Plan 2020-2025 was then published to provide a clear path forward for the federal government and the entire health and disability system to implement He Korowai Oranga.
Best practices and conditions for a successful realization of He Korowai Oranga include, but is not limited to:
- A commitment to Te Tiriti o Waitangi (Te Tiriti), the framework that describes the Crown's obligations in New Zealand's health and disability system as it pertains to Māori. This includes enabling Māori self-determination, providing adequate resources for Māori health and disability services, ensuring all health and disability services are provided in a culturally appropriate way, and ensuring Māori are co-designers with the Crown of the primary health system for Māori.
- Establishing meaningful Māori-Crown partnerships and relationships that are built on a foundation of trust and confidence.
- Enabling Māori leadership and participation in key governance mechanisms and decision-making processes, including building capacity for future Māori health and disability leaders.
- Cross-sector integration and a coordinated, whole-of-government approach to address social determinants of health and support the provision of culturally safe care.
- Establishing mechanisms to collect and use data in a meaningful way, including understanding differences in health outcomes and using the data to support decision-making innovation, and continuous improvement of the quality of care for Māori.
- Accountabilities of the federal government and other key partners are clearly defined, including transparent performance and reporting mechanisms.Footnote 132
Southcentral Foundation's Nuka System of Care
The Nuka System of Care is a model of Indigenous-owned healthcare that describes a wholistic health care system that is created, managed, and owned by Alaska Native people to achieve wellness in all aspects – physical, mental, emotional, and spiritual. It was developed by the Southcentral Foundation, a non-profit health care organization based in Alaska, and is the model on which the FNHA was based.
As part of the Nuka System of Care, Alaska Native people are 'customer-owners' of the health care system. Customer-owners are at the center of this model and focus is placed on building meaningful relationships with customers-owners in order to achieve improved health outcomes. This includes establishing mutual trust between service providers and customer-owners as well as collaborating with partners from various jurisdictions and sectors.
To ensure customer-owners design, implement, and maintain control of their own health care programs and services, Southcentral Foundation established multiple communication and feedback mechanisms to ensure the perspectives of customer-owners from over 200 tribes in Alaska are adequately captured. This includes surveys, a twenty-four-hour hotline, focus groups, and advisory committees. Functional committees, with members made up of Alaska Native representatives, have also been established to respond to customer-owner feedback and ensure there is a clear mechanism to use the feedback to continuously improve the system of care.Footnote 133
Through the Nuka System of Care and the emphasis on customer ownership and relationships, the Southcentral Foundation has directly contributed to a significant improvement in health outcomes, including a 42% reduction in emergency room use (illustrating a proactive approach to healthcare as opposed to reactive); a 36% reduction of days spent in hospital; a 75% reduction in staff turnover; a 25% increase in childhood vaccination rates; and 94% increase of patient reports of culturally safe experiences in healthcare.Footnote 134
In addition to the initiatives highlighted above, interviews conducted with both internal and external partners during this evaluation also highlighted the following best practices in the areas of data sovereignty, relationship building, knowledge sharing and collaboration:
- The importance of data collection was specified as valuable in order to understand changes over time. In particular, supporting First Nations and Inuit data sovereignty is required to ensure information that is shared truly reflects First Nations and Inuit needs and priorities, including access to culturally safe health care.
- The value of building respectful and longstanding relationships with First Nations was repeatedly emphasized in interviews, along with a clear understanding of the department's role. It was regarded that two-way feedback facilitates an understanding of what aspects are working well for First Nations and Inuit and what is not.
- Building communication mechanisms and networks for First Nations and Inuit and ISC staff alike to share knowledge, best practices, and lessons learned was highlighted as valuable in supporting continued progress. Interviews also emphasized the role that effective documentation of knowledge by both ISC staff and personnel in First Nations health services plays in supporting knowledge transfer and building expertise.
- Breaking down barriers between services, sectors, organizations, and levels of government is key to promoting a more wholistic view of health care service delivery for First Nations and Inuit. As described in previous sections of this report, there are opportunities for ISC programs to be better integrated to address social determinants of health.
4. Conclusions
4.1 Conclusions
4.1.1 Relevance
First Nation and Inuit have a complex and expansive list of health needs that need to be addressed by the programs in the Cluster and beyond to improve First Nations and Inuit access to and quality of health care services. People in First Nations and Inuit communities require health services that are identified based on specific community needs, in consideration of social determinants of health, cultural safety and humility, and level of integration across the health services continuum. In order to achieve this, First Nations and Inuit need the resources to overcome externally generated social and policy obstacles that impede access to adequate care.
Both internal and external interviews indicate that the objectives of the Cluster programs are well aligned with the identified health needs of First Nations and Inuit, as well as the Canadian Patient Safety and the Declaration of Cultural Safety and Humility. However, there are significant improvements required in the way the programs in the Cluster are designed and delivered to ensure achievement of these objectives through the Cluster programs.
The complexity and integration/relationship between health needs of First Nations and Inuit require an equally complex and comprehensive ecosystem of health services to adequately address them. The continued and exhaustive list of needs related to accessing health services, higher prevalence of critical medical conditions, and significant inequities within the broader social determinants of health indicate several priority areas. This is likely to create challenges in prioritization of resources and ability to make meaningful strides to any one goal, due to the abundance of focus areas.
The pandemic highlighted the severity of health needs of First Nations and Inuit as well as shortages and inequities related to appropriate health facilities, eHealth technologies, skilled community-based workers, and governance structures to manage public health crises. Consideration should be made to whether the resource allocation to Cluster programs is adequate to meet the increased demand of the post-pandemic health landscape.
The relevance of the programs, in regard to the needs they were designed to address, is evident. There was a notable trend across the country towards needs for appropriate and adequate health facilities, access to eHealth technologies, trained and educated community-based health care workers, accredited health centres, and improved collaboration between government levels to move towards self-government and autonomy. Yet, the level of need amongst these common areas differed by region and by specific community. Further, First Nations and Inuit have unique needs related to their population demographics and geographical locations. These variations imply that the Cluster programs would be most effective if designed with the appropriate level of flexibility to allow programs to adapt resource allocation to align with localized needs.
The need for both medically competent and culturally safe health care in First Nations and Inuit communities was evident and consistent. The objectives of the programs were aligned with the Declaration and Framework, in their intent. In particular, programs such as the HHR and QIAP work specifically to increase the presence of First Nations and Inuit health care professionals in community and build the appropriate expertise and governance frameworks to ensure high standards of quality in First Nations and Inuit health care. However, it was also evident that the integration of specific mechanisms to ensure patient safety and cultural humility were not necessarily prioritized in the design or delivery of the Cluster and instead fell to the people in First Nations and Inuit communities to find ways to create this alignment. The implications of this absence of intentional integration are significant, as the lack of access to medically and culturally safe care are foundational issues that contribute to several other areas of need. Therefore, a lack of progress here will create a consequent obstacle in progress in other key areas of need identified.
4.1.2 Effectiveness
Program partners noted key challenges that require improvement, particularly around program delivery and administration processes, performance measurement, and reporting. Areas for improvement highlighted included: access to sustainable long-term funding, an improved recognition of local needs, enhanced funding for and focus on training, and community awareness of programs. Further, challenges were raised in relation to performance measurement and reporting as a result of data limitations, a misalignment of western data-based reporting approaches to First Nations and Inuit ways of knowing, and the burden of reporting amidst already overcapacity and understaffed health centres in communities.
The value and impact of the Cluster programs, including improving access to and quality of health care for First Nations and Inuit was highlighted by most partners who participated in the evaluation. Interviews indicated that progress has been made towards empowering First Nations and Inuit to take on the planning and management of health services and building capacity and capabilities within communities to prepare for service transfer.
However, the limited resources, both financial and human, was highlighted as a prominent obstacle impeding the achievement of the Cluster programs' intended outcomes during the evaluation scope period. Additionally, further challenges were highlighted in the impact the pandemic had on timelines and resources, the lack of flexibility of program parameters compared to First Nations and Inuit health care needs, the inability to secure sustainable funding, and the turnover in staff as an impediment to building lasting relationships and achieving progress towards the Cluster programs' intended outcomes.
The global pandemic had significant impacts in the delivery of health services to First Nations including limiting both access in and out of communities during lockdown measures and diverting resources towards pandemic response and away from other existing health needs and priorities. However, positive impacts were also noted, including a notable increase in efficiency in both funding releases from the federal government and program delivery, as well as an increase in demand and appreciation of the value of the intended outcomes of programs, particularly eHealth and Accreditation. It also highlighted opportunities for innovation in program design and application of resources. The program spurred the consideration of lessons learned, particularly around emergency preparedness and key priorities in health services delivery.
The COVID-19 pandemic was a wake-up call to the health industry globally, but especially for non-First Nations and Inuit governments as the pandemic highlighted the health-related issues facing those in First Nations and Inuit communities. The crisis served as the ultimate representation of the value of appropriately governed health facilities with the expertise, capacity, and resources to have emergency preparedness and crisis management plans in place. It also allowed First Nations and Inuit to demonstrate what they are capable of when adequately supported. The ability of those in First Nations and Inuit communities, with support from ISC, to pivot and adapt rapidly in order to carry out the pandemic response in addition to meeting regular health needs was commendable. Programs were creative in leveraging new partners to provide added value to the pandemic response. The implications of the increased efficiency and innovation that were facilitated by the prioritization of the pandemic response (i.e., less red-tape, faster allocation of resources) are significant, highlighting that with access to resources, First Nations and Inuit can make significant progress in addressing their health needs. Moreover, the challenges faced by health services such as the inability to access communities in lockdown, labour shortages, or the lack of connectivity for virtual services, demonstrated the critical value of what the Cluster programs aim to achieve. Consideration should be made to identifying opportunities to reduce administrative burdens and increase flexibility of funding allocations to allow for efficient program delivery and innovative solutions.
Overall, the effectiveness of relationships between program partners varies significantly between program type and region due to factors such as region-specific agreements and funding levels. Relationships between ISC HQ and ISC Regions, ISC Regions and First Nations and Inuit, and ISC Regions and Provincial and Territorial (PT) governments were highlighted as the ones most in need of improvement, with partners citing challenges with consistent staff turnover, ineffective communication regarding funding, and lack of engagement. There is a need for increased, intentional collaboration amongst key program partners, with particular attention paid to clarifying roles and responsibilities between ISC HQ and ISC regions, and improved communications around service transfer (definition and clarity on how to effectively support it). Productive relationships between each Cluster program were noted to be rare, despite a shared ultimate outcome and certain thematic overlaps of services. There is an opportunity to increase the effectiveness and efficiency of the Cluster programs through enhanced collaboration and integration.
The importance of relationship building was a consistent trend throughout the evaluation. The challenges partners faced in sustaining effective relationships in the face of staff turnover, severely limited capacity, and communication barriers presents significant implications regarding the ability of the Cluster programs to achieve intended outcomes and ultimately transfer services.
Defining and understanding roles, responsibilities, and accountabilities of key partners are vital in building trusting and sustainable relationships. The lack of clarity of roles and responsibilities between ISC HQ and ISC Regions, and between ISC Regions and First Nations and Inuit can create misaligned expectations and tension between partners. The lack of clarity and effective communication around the definition of service transfer, the intended end-state, and path towards it among program partners also has significant implications to their ability to work together to achieve it. Without a clear vision of what program partners are working towards, it will be challenging to plan and implement a way forward. Consideration should be made to developing and distributing clear communication materials about the Departmental mandate to both internal and external partners (e.g., what do transferred services look like, how do First Nations and Inuit get there, what are the main priorities, etc.).
Though not operationally designed as a Cluster, there is a clear compatibility of the Cluster programs in regard to their objectives and desired outcomes. For example, in order to be accredited, a health centre must put in place a health plan, which is a key output of the HPQM program. Further, to ensure proper physical infrastructure is built in health facilities, eHealth technologies are often required at the onset. Despite this alignment, the programs were found to operate in siloes, with very limited collaboration across the spectrum when delivering programs. This implies an opportunity to improve efficiencies and achievement of progress towards objectives through increased, early collaboration between programs. Consideration should be made to identifying points of integration between programs (with each other as well as with other Departmental programming outside of the Cluster) and highlighting opportunities in shared regions of operation to work together to achieve common goals.
4.1.3 Service Transfer
The goal of service transfer is aligned to the overarching health needs of First Nations and Inuit; however, only once a certain level of capacity has been built and funding is sustainable for long-term planning.
Service transfer is a complex endeavour with many conditions required to achieve success, including effective relationships and buy-in from relevant partners, knowledge and expertise in health services delivery, access to and control of sustainable funding, and strong governance structures. Key themes in barriers towards successful service transfer noted include an insufficient level of funding, continuous turnover of ISC staff, ineffective or restrictive approaches to transferring services, and variances in stages of readiness of both communities and programs that are to be transferred. The individual programs in the Cluster each contribute to the building of necessary capacities to facilitate service transfer; however, while the Cluster has made strides towards achieving its immediate outcomes, there are significant gaps in the sustainability required to produce systemic results.
It is evident that while the intention of eventual service transfer is relevant to existing needs, there are critical barriers in place, impacting the programs' ability to support the achievement of the departmental mandate of service transfer. The apprehension of First Nations and Inuit to take control of services despite their desire for self-government is indicative of the gap in appropriate sustainable resources available to build adequate capacity among First Nations and Inuit. Consideration should be made to better defining the path to successfully transferred services, and the role the Cluster programs and their partners play in achieving their long-term, intended outcomes.
4.1.4 Efficiency
There is a lack of sufficient and sustainable resources (financial, human, and capital) to support the Cluster programs in the achievement of their intended objectives. Needs-based funding, instead of population-based funding, would be more effective in achieving Cluster program objectives. Key challenges noted within program funding included insufficient operations and maintenance (O&M) funding and a lack of consideration in annual funding allocations towards economic changes (i.e., inflation, cost of living). In addition to insufficient financial resources, concerns were raised around the lack of human resources, including insufficient number of staff and need for particular capabilities (e.g., specialized health workers, patient safety navigators, IT professionals and administrators) and infrastructure resources to meet capacity needs (e.g., medical equipment, technological infrastructure, etc.).
Despite the relevance of the Cluster, its effectiveness is dependant on the level of resources invested in actualizing its objectives. There is a misalignment in the scope of the outcomes and the resources available to programs, and in turn people in First Nations and Inuit communities, which may be a result of a lack of integrated strategic and operational planning. Consideration should be made to re-baselining the priorities of the Cluster programs as an ecosystem (e.g., logic model), assessing the feasibility of attaining objectives within the parameters of available resources, and identifying opportunities to increase efficiencies within programs to better optimize the limited resources available.
The challenges First Nations and Inuit face in recruiting and retaining qualified health care staff with the required medical and cultural expertise, particularly based in communities, has significant implications on the ability of programs to achieve their objectives and for First Nations and Inuit to sustainably take on transferred services. Establishing and maintaining effective health infrastructure supports requires skillsets and capabilities beyond primary health care roles (e.g., doctors, nurses) in order to provide wholistic services to First Nations and Inuit that meet modern standards for quality and access (e.g., data analytics, financial management).
5. Recommendations
- Leveraging existing needs assessments, engagement efforts, and consultations, develop a funding approach that addresses funding gaps and provides flexibility and sustainability to the programs evaluated.
- FNIHB works with First Nation and Inuit partners to co-develop and begin to implement a strategy – including identifying partners, approach and timing – to build capacity among Indigenous health leaders, health service providers, and supporting roles to increase opportunities for training and knowledge sharing between communities.
- To allow for uniform and flexible program application to equitably serve communities, FNIHB must:
- Perform an assessment of internal human resourcing to inform an internal human resources strategy in FNIHB that appropriately staffs and retains employees within the programs evaluated; and
- Create mechanisms to ensure program staff have common knowledge and understanding between and within evaluated programs and foster ongoing opportunities for knowledge exchange.
- In order to achieve a more wholistic and effective approach to service transfer, an alignment and integration between evaluated programs within FNIHB and ISC's broader vision of service transfer is required. It is recommended that FNIHB works with First Nations and Inuit, as well as ISC Strategic Policy Sector and Regional staff, collaborate to:
- Develop a workplan to communicate the evaluated programs' visions of transfer that are aligned with department's service transfer approach and vision; and
- Conduct an assessment that identifies commonality and redundancies between evaluated programs to support integration of programs and gradual transfer of services.
- FNIHB works with partners to develop a meaningful performance measurement strategy with the Chief Finances, Results and Deliver Officer Sector's (CFRDO) Results and Delivery Unit and supporting data collection and management strategy with Chief Data Officer (CDO) and Chief Information Officer (CIO) to support Indigenous data sovereignty in health services.
Appendices
Appendix A – Evaluation Matrix
Note that only those indicators for which 'Key Informant Interviews' is indicated as a line of evidence are assessed and discussed in this report.
| Line of Evidence | |||||||
|---|---|---|---|---|---|---|---|
| Evaluation Question | Indicators | Literature Review | Document Review | Key Informant Interviews | Surveys | Data Analysis | Case Studies |
| Relevance | |||||||
|
Evidence in document and literature review regarding the community health needs in First Nation and Inuit communities | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable |
| Perceptions of key informants regarding the community health needs in First Nation and Inuit communities | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which community health needs in First Nation and Inuit communities have evolved over time, including how the COVID-19 pandemic has impacted these community health needs | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Number of communities that have community health plans compared to all communities or those that identify a need | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Number of health facilities that desire accreditation and those that have achieved accreditation | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Evidence in document and literature review regarding the health needs of First Nations and Inuit communities in a COVID-19 environment | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable | |
|
Evidence in document and literature review regarding the extent to which the cluster of programs are aligned with the current health needs of First Nations and Inuit communities | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable |
| Perceptions of key informants regarding the extent to which the cluster of programs are aligned with the current health needs of First Nations and Inuit communities | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document and literature review regarding the extent to which the cluster of health programs support the principles of the Canadian Patient Safety and Quality Framework and the Declaration on Cultural Safety and Humility | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which the cluster of health programs support the principles of the Canadian Patient Safety and Quality Framework and the Declaration on Cultural Safety and Humility | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
|
Evidence in document and literature review regarding the extent to which the departmental goal of service transfer is aligned to the needs of First Nations and Inuit communities | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable |
| Perceptions of key informants regarding the extent to which the departmental goal of service transfer is aligned to the needs of First Nations and Inuit communities | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document review regarding the extent to which the cluster of health programs work together to achieve the department's objectives | Not applicable | Applicable | Not applicable | Applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which the cluster of health infrastructure support programs is the appropriate mix of programs to achieve the departmental goal of service transfer | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Effectiveness | |||||||
|
Evidence in program statistics of the achievement of performance targets for each program and the coverage of communities | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable |
| Evidence in document and program data review of increased integration of health services and systems (federal, provincial, territorial, municipal, community) (Health Services Integration Fund) | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which the integration of health services and systems have increased (federal, provincial, territorial, municipal, community) (Health Services Integration Fund) | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document and program data review that communities can manage and operate health programs and services (Health Planning & Quality Management) | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which communities can manage and operate health programs and services (Health Planning & Quality Management) | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Evidence in document and program data review that First Nations and health care providers have access to eHealth technologies (eHealth Infostructure) | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which First Nations and health care providers have access to eHealth technologies (eHealth Infostructure) | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in literature, document, and program data review that there is an increased number of Indigenous peoples who are pursing or have received education and training in health care services (Health Human Resources) | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Evidence in literature, document, and program data review that there is an increased number of Indigenous peoples who work in health care in their communities and integrate traditional medicine and healing (Health Human Resources) | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which there is an increased number of Indigenous peoples who work in health care in their communities and integrate traditional medicine and healing (Health Human Resources) | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the extent to which the quality of health services in First Nations and Inuit communities is improved and/or maintained (Quality Improvement & Accreditation) | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which the quality of health services in First Nations and Inuit communities is improved and/or maintained (Quality Improvement & Accreditation) | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the extent to which First Nations are support to plan, manage, and maintain their health facility infrastructure (Health Facilities Program) | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which First Nations are support to plan, manage, and maintain their health facility infrastructure (Health Facilities Program) | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the extent to which BC First Nations' health services are integrated with provincial health services and ISC (BC Tripartite) | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which BC First Nations' health services are integrated with provincial health services and ISC (BC Tripartite) | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
|
Evidence in document, literature, and program data review regarding the impact of the COVID-19 pandemic on the ability of the cluster of programs to support the health needs of Indigenous communities and organizations | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable |
| Perceptions of key informants regarding the impact of the COVID-19 pandemic on the ability of the cluster of programs to support the health needs of Indigenous communities and organizations | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in literature and document review regarding areas of improvement for the programs to be better able to deal with current or future pandemics or other similar health crises | Applicable | Applicable | Not applicable | Applicable | Not applicable | Not applicable | |
| Perceptions of key informants regarding the program aspects that need to be improved in order for the cluster of health infrastructure support programs to be better able to deal with current or future pandemics of other similar health crises | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Additional funding allocated to the programs in the cluster due to the COVID-19 pandemic | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the utility and/or impact of the additional COVID-19 funding, if any | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
|
Evidence in document, literature, and program data review regarding the extent to which the cluster of health programs supports service transfer | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable |
| Evidence in document, literature, and program data review regarding the extent to which services have been transferred | Applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the state of readiness of First Nations and Inuit health care systems to be independently designed, delivered, and managed by communities or independent institutions | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which the cluster of health programs supports service transfer | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which services have been transferred | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which the programs within the Cluster are contributing to systemic change in how the federal government delivers health services to Indigenous peoples | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
|
Evidence in document and program administrative data review regarding the effectiveness of program delivery and administrative processes | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable |
| Perceptions of key informants regarding the effectiveness of program delivery and administrative processes | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the clarity and adequacy of the communication of program delivery and administrative processes to key partners | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the clarity and adequacy of the communication of program delivery and administrative processes to key partners | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the extent to which roles and responsibilities of programs within the Cluster are clearly defined, well understood, and communicated | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which roles and responsibilities of programs within the Cluster are clearly defined, well understood, and communicated | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Evidence in document and program data review regarding the extent to which performance measures for each of the programs within the Cluster have been established | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which a performance measurement framework has been established for each of the programs within the Cluster and is being used to monitor and report on performance as well as support decision making | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the program delivery aspects that are working well, and which aspects need improvement | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding potential barriers to service transfer | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding necessary conditions for effective service transfer | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Evidence in document and literature review regarding potential barriers to service transfer | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable | |
| Evidence in document and literature review regarding necessary conditions for effective service transfer | Applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable | |
|
Perceptions of key informants regarding the nature of the relationships between program partners (e.g., ISC Headquarters, regional offices, Indigenous communities, etc.) and the extent to which the relationships are effective and productive | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable |
| Perceptions of key informants regarding the nature of the relationships between programs and the extent to which the relationships are effective and productive | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document review regarding the extent to which the programs in the Cluster work together to support service delivery | Not applicable | Applicable | Not applicable | Not applicable | Not applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which the programs in the Cluster work together to support service delivery | Not applicable | Not applicable | Applicable | Applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which the programs in the Cluster work together to support one another | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Efficiency | |||||||
|
Evidence in document and program data review regarding the extent to which the programs within the Cluster have performance measures in place to measure and monitor cost-effectiveness | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable |
| Perceptions of key informants regarding the extent to which the resources dedicated to each of the programs within the Cluster are adequate and optimized | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in documentation (e.g., program data, financial data) regarding the extent to which the resources dedicated to each of the programs within the Cluster are adequate and optimized | Not applicable | Applicable | Not applicable | Not applicable | Applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which funding is allocated efficiently and effectively to achieve the expected outcomes of the programs within the Cluster | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which funding is sufficient for programs within the Cluster to achieve their respective expected outcomes | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Perceptions of key informants regarding the extent to which resource allocation is sufficient to achieve the broader departmental goal of service transfer (in consideration of how the programs within the Cluster may or may not work together) | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | |
| Perceptions of key informants regarding opportunities to improve the delivery of the programs within the Cluster | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Unintended outcomes of the programs within the Cluster, and/or of the programs as they may or may not operate together to support service transfer | Applicable | Applicable | Applicable | Applicable | Applicable | Applicable | |
| Lessons learned in program design or delivery | Applicable | Applicable | Not applicable | Applicable | Applicable | Applicable | |
| Best practices in program design or delivery | Applicable | Applicable | Not applicable | Applicable | Applicable | Applicable | |
| Perceptions of key informants regarding best practices and lessons learned in the design or delivery of the programs within the Cluster | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
| Evidence in document review regarding the extent to which GBA+ was considered in the design or delivery of the programs within the Cluster | Not applicable | Applicable | Not applicable | Applicable | Not applicable | Not applicable | |
| Perceptions of key informants regarding the extent to which GBA+ was considered in the design or delivery of the programs within the Cluster | Not applicable | Not applicable | Applicable | Not applicable | Not applicable | Applicable | |
Appendix B – Key Informants
| Stakeholder Groups | Number of Interviewees | |
|---|---|---|
| Internal | ISC HQ Senior Management | 3 |
| ISC Regional Executives | 3 | |
| Program Leads | 7 | |
| ISC Regional Staff | 57 (7 focus groups) | |
| External | First Nations Representatives | 19 |
| Implementing Partners | 10 | |
| Subject Matter Experts | 4 | |
| Total | 103 | |
Appendix C – Survey Participants
| Respondent Stakeholder Group | Number of Participants | |
|---|---|---|
| Internal | ISC Regional Staff | 40 |
| External | First Nations Representatives | 16 |
| Implementing Partners | 18 | |
| Total | 74 | |
Appendix D – Cluster Logic Model

Text alternative for Cluster Logic Model
Appendix D is a diagram showing the overarching logic model for ISC's cluster of Health Infrastructure Support for First Nations and Inuit, created in July 2019 specifically for the program evaluation. The diagram starts at the top with specific programs: Health Planning an Quality Management, Health Services Integration Fund, Quality Improvement and Accreditation; eHealth Infostructure; Health Human Resources; BC Tripartite Relationship; and Health Facilities. The diagram continues with downward pointing arrows to indicate the activities of each program. It then describes the outputs, immediate outcomes, intermediate outcomes and ultimate outcomes.
Appendix E – Case Study Background Information
All information included in the Case Study Background Information tables was directly sourced from the relevant link(s) noted, as well as interview(s) with individual(s) from each organization.
The Selection Criteria used to choose organizations to request to engage in a case study included:
Geography
The case studies should include geographic representation from varying regions within Canada (e.g. Inuit Nunangat, North, West, East, Central) to ensure that the varying circumstances of First Nations and Inuit in each jurisdiction are considered as much as possible.
Program Representation
The case studies should include representation from all seven programs included in the scope of this Evaluation. While there may not be communities that access or benefit from all seven of the programs at once, the Evaluation Team will aim to select communities that have implemented at least two or more of the Cluster programs. This will allow the Evaluation Team to gain insight into how the programs may or may not work together and if there are opportunities to improve how the Cluster of programs is designed and delivered.
Service Transfer Continuum
Where possible, the Evaluation Team will work with program representatives to select communities that are at different stages along the 'service transfer continuum' (i.e. the Cluster's programs are primarily delivered by ISC and its implementing partners versus the Cluster's programs have been devolved and are being implemented by the community). This will allow the Evaluation Team to gain a better understanding of success factors and best practices in service transfer, potential barriers to service transfer, and approaches to address those barriers. The Evaluation Team will also work with program representatives to identify a variety of communities at varying levels of aggregation to determine and assess critical mass required to effectively deliver a program.
First Nations Representation
The case studies must include First Nations representation to ensure that the First Nations experience with the Cluster is considered.
Inuit Representation
The case studies must include Inuit representation to ensure that the Inuit experience with the Cluster is considered.
Organization: Onion Lake First Nation
Organization mandate: Onion Lake is a Cree Nation with Chief and Council, as well as a Board of Directors consisting of five members. One of the Onion Lake Board's objectives is improving the overall holistic health of the community. In addition to the community's commitment to holistic health, the Onion Lake First Nation formed an organization, the Onion Lake Group of Companies Corporation, which consists of nine companies.
Population: 7,000 total (5,000 living on-reserve and 2,000 married into the community or non-Indigenous employees) (2,000 consists of "Other" First Nations, non-First Nations married in and/or extended family, non-First Nations employees that work for the community, "Other" First Nations who work for the community)
Region: Treaty 6 Territory
Province: Saskatchewan and Alberta
Health Cluster Programs:
- Fiscal Year 2015-16: Health Planning; HSIF; eHealth
- Fiscal Year 2016-17: Health Planning; HSIF; eHealth
- Fiscal Year 2017-18: Health Planning; HSIF; eHealth
- Fiscal Year 2018-19: Health Planning; HSIF; HFP; eHealth
- Fiscal Year 2019-20: Health Planning; HSIF; HFP; eHealth
- Fiscal Year 2020-21: Health Planning; HSIF; HFP; eHealth
- Fiscal Year 2021-22: Health Planning; HSIF; eHealth
- Fiscal Year 2022-23: Health Planning; eHealth
First Nation/Inuit/others: First Nations
Relevant Links: Onion Lake Cree Nation
Service Continuum: Onion Lake First Nation has the following departments:
- Business Development Corporation
- Education
- Family Services
- Finance
- Health
- Housing
- Human Resources
- Lands
- Native Justice
- Onion Lake Energy
- Operations
- Social Development
- Sports & Rec
- Treaty Governance
- Treaty Land Entitlement
- Public Works
- Fire Rescue & Security
- Ambulance
Onion Lake First Nation took over full control of community health programming and some non-insured health programs and services, and ambulatory care. Additionally, they made agreements that they are to deliver at a local level. The Nation negotiated with the Province of Saskatchewan to establish a dedicated ambulance service for their community members. The Nation has also negotiated with previous regional health authorities before they were disbanded to form the one remaining Saskatchewan Health Authority, allowing the services to be negotiated at the provincial level.
Community health programming that is delivered by Onion Lake includes pre-and-post-natal care, x-ray medical imaging, a pharmacy, and a clinic department staffed with doctors and nurse practitioners. These initiatives have been supported in part by the Health Services Integration Fund. The Nation is currently developing their own health care system for primary health care delivery.
What is significant about this organization that makes it a good candidate to include as a case study in the Health Cluster Evaluation?
Provides community services both on and off reserve and to population that includes First Nations, non-Indigenous partners of First Nations, and non-Indigenous employees of the community.
Organization: Southern Chiefs' Organization
Organization mandate: The Southern Chiefs' Organization (SCO) was established in 1999 and represents 34 southern First Nation communities in Manitoba. The organization is an independent political forum that aims to protect, preserve, promote, and enhance First Nations peoples' rights, languages, customs, and traditions through the spirit and intent of the Treaty-making process. The organization works towards its objectives through a variety of program areas including health transformation, environment, justice, mental wellness, child and family services programs, among many others. The organization's website also provides easily accessible educational tools to increase awareness of First Nation history along with education, scholarships, and funding opportunities available. The website also provides resources to support First Nation communities.
Population: 83,000
Region: Headingley (Swan Lake First Nation)
Province: Manitoba
Health Cluster Programs:
- Fiscal Year 2015-16: HSIF
- Fiscal Year 2016-17: HSIF
- Fiscal Year 2017-18: HSIF
- Fiscal Year 2018-19: HSIF
- Fiscal Year 2019-20: HSIF
- Fiscal Year 2020-21: HSIF
- Fiscal Year 2021-22: HSIF
- Fiscal Year 2022-23: HSIF
First Nation/Inuit/others: First Nations
Relevant Links: Southern Chiefs' Organization Inc.
Service Continuum: SCO notes that they are in the planning and design phase for the Health Transformation service transfer and when data was collected for this evaluation, they had not actively had any ISC programming devolved to them. SCO calls for increased programming and funding responsibility as it leads the service transfer process. If organizations, including SCO, were not required to compete for funding from the same funding envelope, it is anticipated that an increased ability to deliver large aggregate programming and services to southern First Nations communities throughout Manitoba would be observed. The system as it currently operates does not support collaboration within the First Nations because often the provincial or federal governments are providing funding to both large organizations to carry out large system change opportunities and smaller entities to do some of that work which causes confusion and challenges about who is leading the work.
What is significant about this organization that makes it a good candidate to include as a case study in the Health Cluster Evaluation?
SCO represents 34 Southern First Nations in the Manitoba southern region.
Organization: Giishkaandago'lkwe Health Services (Fort Frances Tribal Area Health Services)
Organization mandate: Giishkaandago'lkwe Health Services (Fort Frances Tribal Area Health Services) works with ten Treaty 3 First Nations in the Fort Frances region to improve community health and wellness. The organization works with the communities it serves, partners, and founders to deliver on its mandate. Their mission is lifelong good health by leading innovative health care through the guidance of the seven grandfather teachings of the Anishinaabe. The organization is driven by the following seven values:
- Nibwaakaawin (Wisdom)
- Zaagiidiwin (Love)
- Aakodewewin (Bravery)
- Dibaadendiziwin (Humility)
- Minwaadendamowin (Respect)
- Gwekaadiziwin (Honesty)
- Dibwewin (Truth)
Population: 2,600
Region: Fort Frances
Province: Ontario
Health Cluster Programs:
- Fiscal Year 2015-16:
- Fiscal Year 2016-17:
- Fiscal Year 2017-18:
- Fiscal Year 2018-19:
- Fiscal Year 2019-20: HSIF
- Fiscal Year 2020-21: HSIF
- Fiscal Year 2021-22: HSIF
- Fiscal Year 2022-23: Health Planning; HSIF
First Nation/Inuit/others: First Nations
Relevant Links: Giishkaandago'ikwe Health Services
Service Continuum: Giishkaandago'lkwe Health Services provides a variety of healthcare related services including infant and child development; palliative care; a mental health and addictions program including a 10-bed treatment program; a Home and Community Care program, which includes diabetes and foot care clinics as well as home and healthcare nursing programming; long-term care; homemaking assessments; and environmental and community health programming. Giishkaandago'lkwe is also increasingly supporting rural First Nations through their Jordan's Principle program and mental health and addictions programming.
Giishkaandago'lkwe has had their Environmental Public Health programming devolved to them and has since hired a water quality analyst and performed water testing and operations, created and enacted policies and procedures related to physical infrastructure work (septic fields, coding, animal bites), and education and community planning efforts to increase awareness and education of their water system.
What is significant about this organization that makes it a good candidate to include as a case study in the Health Cluster Evaluation?
Giishkaandago'lkwe works with ten Treaty 3 First Nations and also currently operates their Environmental Public Health programming after having this devolved to them.
Organization: File Hills Qu'Appelle Tribal Council
Organization mandate: File Hills Qu'Appelle Tribal Council (FHQTC) is a political and service organization that aims to protect, implement, and enforce inherent Treaty Rights, promote self determination, and develop communities for the 11 Nations it serves. The File Hills Qu'Appelle Tribal Council is working towards a governance transition. A governance transition for the File Hills Qu'Appelle Tribal Council means transitioning towards inclusion of Indigenous culture into governance structures. This transition is working towards more community engagement and enforcement of Inherent and Treaty rights.
Population: 15,000+
Region: Fort Qu'Appelle
Province: Saskatchewan
Health Cluster Programs:
- Fiscal Year 2015-16: Health Planning; HSIF
- Fiscal Year 2016-17: Health Planning; HSIF
- Fiscal Year 2017-18: Health Planning; HSIF
- Fiscal Year 2018-19: Health Planning; HSIF
- Fiscal Year 2019-20: Health Planning;
- Fiscal Year 2020-21: Health Planning;
- Fiscal Year 2021-22:
- Fiscal Year 2022-23:
First Nation/Inuit/others: First Nations
Relevant Links: File Hills Qu'Appelle Tribal Council
Service Continuum: FHQTC operates a plethora of programs and services, including education, pre-employment services, childcare licensing, communications, Indigenous Skills and Employment Training Strategy programming (ISETS), sports and recreation, training and employment, leads and resources, restorative justice, technical services, human resources, a Women's Commission, a Youth Strategy Council, a Knowledge Keepers Council, health services, and a Lifespeakers Council for members of the 11 Nations that the Council serves.
What is significant about this organization that makes it a good candidate to include as a case study in the Health Cluster Evaluation?
FHQTC jointly owns the only First Nations hospital in Canada, All Nations Healing Hospital (ANHH). FHQTC provides administration and is responsible for the operations of the ANHH. The All Nations Healing Hospital serves 15 First Nations, 11 of which are represented by the Tribal Council. The hospital has a busy emergency room, laboratory services, a low-risk birthing unit, acute services clinics, and multiple clinical programs, including Women's Health Services and the Rising Bear Healing Center which also offers Chronic Kidney Disease care and satellite dialysis services. The FHQTC Health Services Department also operates clinical services, including Red Wolf, a harm reduction program with mental health and addictions support, as well as opioid replacement therapy programming and services related to Hepatitis C and HIV, Jordan's Principle programming, public health programming, community health nursing, rehabilitation therapies, environmental health services, a chronic disease program, home healthcare, diabetes healthcare, and research and health planning and management teams.
Both organizations are independently accredited by Accreditation Canada and I December of 2022 FHQTC Health Services was Accredited with Exemplary Standing.
Organization: First Nations of Québec and Labrador Health and Social Services Commission/Commission de la santé et des services sociaux des Premières Nations du Québec et du Labrador
Organization mandate: The First Nations of Quebec and Labrador Health and Social Services Commission (FNQLHSSC) is a non-profit organization and was created in 1994 by the Chiefs of the Assembly of First Nations Quebec-Labrador. FNQLHSSC focuses on the planning and implementing of culturally appropriate preventative health and social services programs in support of First Nations communities.
Population: Non-treaty First Nations of Quebec and two Innu bands in Labrador
Region: Québec
Province: Québec
Health Cluster Programs:
- Fiscal Year 2015-16: Health Planning; HSIF; eHealth
- Fiscal Year 2016-17: Health Planning; HSIF; eHealth
- Fiscal Year 2017-18: Health Planning; HSIF; eHealth
- Fiscal Year 2018-19: Health Planning; HSIF; eHealth
- Fiscal Year 2019-20: Health Planning; eHealth
- Fiscal Year 2020-21: Health Planning; eHealth
- Fiscal Year 2021-22: Health Planning; eHealth
- Fiscal Year 2022-23: Health Planning; eHealth
First Nation/Inuit/others: First Nations
Relevant Links: First Nations of Québec and Labrador Health and Social Services Commission; Commission de la santé et des services sociaux des Premières Nations du Québec et du Labrador
Service Continuum: The FNQLHSSC offers support to improve access to adequate services for children, seniors and families; cultural services to promote community well-being; governance and community engagement; health and wellness services; income security and social inclusion; psychosocial support; and support for research and information resources.
What is significant about this organization that makes it a good candidate to include as a case study in the Health Cluster Evaluation?
Represents 43 communities
Appendix F – Works Cited
- Accreditation Canada. (2019, May 23). Accreditation Is An 'Invaluable Process' that First Nations Communities Should Undertake, says Esk'etemc Advanced Practice Nurse. (link not available)
- Accreditation Canada. (2020, July 13). Information for the Public - Improving Quality Heath Care Across Canada.
- Accreditation Canada. (2019, May 23). Accreditation Is An 'Invaluable Process' that First Nations Communities Should Undertake, says Esk'etemc Advanced Practice Nurse. (link not available)
- Aetonix. (n.d.). 4 Diseases Impacting Health on First Nations in Canada.
- Allen, L., Hatala, A., Ijaz, S., Courchene, E. D., and Bushie, E. B. (2020). Indigenous-led Health Care Partnerships in Canada. Canadian Medical Association Journal, 192(9).
- Arthritis Society Canada. (n.d.). The Truth about Arthritis.
- Asthma Canada. (2022). 2021 Annual Report (PDF).
- Australian Government Department of Health. (2015). National Aboriginal and Torres Strait Islander Health Plan 2013-2023 (PDF).
- Australian Institute of Health and Welfare. (2015). Implementation Plan goals for the Aboriginal and Torres Strait Islander Health Plan 2013-2023 - Technical companion document (PDF).
- BC Mental Health and Substance Use Services. (2021). How Everyday Racism Affects Everyday Mental Health. (2021). BC Mental Health and Substance Use Services.
- Canadian Aids Society. (n.d.). Aboriginal People.
- Canada Mortgage and Housing Corporation. (2022). Canada's Housing Supply Shortage: Restoring Affordability by 2030.
- Canada Mortgage and Housing Corporation. (2018). Examining Escalating House Prices in Large Canadian Metropolitan Centres (PDF).
- Canadian Patient Safety Institute. (2020). The Canadian Quality and Patient Safety Framework for Health Services (PDF). (2020). Canadian Patient Safety Institute.
- Centre for Diseases Control and Prevention. (2020). Emergency Water Supply Planning Guide for Hospitals and Healthcare Facilities. Centre for Diseases Control and Prevention.
- Department of Health. (2015). Implementation Plan for the National Aboriginal and Torres Strait Islander Health Plan 2013-2023 (PDF).
- Diabetes Canada. (2023). Indigenous Communities and Diabetes. (2023). Diabetes Canada.
- Employment and Social Development Canada. (2016). Thinking About Aging in Place.
- First Nations Health Authority. (2022). FNHA's Policy Statement on Cultural Safety and Humility (PDF). First Nations Health Authority.
- First Nations Health Authority. (n.d.). Traditional Wellness and Healing. (n.d.). First Nations Health Authority.
- First Nations Information Governance Centre. (n.d.). The First Nations Principles of OCAP. (n.d.). First Nations Information Governance Centre.
- First Nations Inuit Health Branch & First Nations Health Authority. (2021, June 25). Report on the Analysis of Accreditation in First Nations Health Services (PDF).
- Gottlieb, K. (2013). The Nuka System of Care: improving health through ownership and relationships. International Journal of Circumpolar Health, 72(1), 21118.
- Government of British Columbia. (2020). In Plain Sight: Addressing Indigenous-Specific Racism and Discrimination in B.C Health Care (PDF).
- Government of Canada Actions to Address Anti-Indigenous Racism in Health Systems. (2021). Indigenous Services Canada.
- Government of New Zealand Ministry of Health. (2020). Whakamaua Māori Health Action Plan 2020-2025 (PDF).
- Heidinger, L. (2022). Violent Victimization and Perceptions of Safety: Experience of First Nations, Métis and Inuit women in Canada. Statistics Canada.
- Homeless Hub. (n.d.). Substance Use and Addiction. (n.d.). Homeless Hub.
- House of Commons Canada. (2022). The Effects of the Housing Shortage on Indigenous peoples in Canada: Report on the Standing Committee on Indigenous and Northern Affairs (PDF). (2022). House of Commons Canada.
- Hypertension Canada. About Us. (n.d.).
- Indigenous Services Canada. (n.d.). Health Services Integration Fund (HSIF) Annual Project Report (PDF).
- Indigenous Services Canada. (n.d.). e-Health Program Year-End Report (PDF).
- Indigenous Services Canada. (2020, February 11). Departmental Plan 2020-2021.
- Indigenous Services Canada. (2020, February 17). eHealth.
- Indigenous Services Canada. (2022, February 17). 2021 Canadian Human Rights Tribunal 41: Order.
- Indspire. (2015, February). Creating Positive Outcomes: Graduation and Employment Rates of Indspire's Financial Award Recipients (PDF).
- Indigenous Services Canada. (2020). eHealth.
- Indigenous Services Canada. (2022, February 17). 2021 Canadian Human Rights Tribunal 41: Order.
- Indigenous Services Canada. (2020, October). Indigenous health management and initiatives.
- Indigenous Services Canada. (2022, August 10). Health Services Integration Fund.
- Indigenous Services Canada. (2021). Transition 2021 Minister Hajdu Indigenous Services Canada overview - Book 1. (2021). Indigenous Services Canada.
- Indspire. (2015, February). Creating Positive Outcomes: Graduation and Employment Rates of Indspire's Financial Award Recipients (PDF).
- Mental Health Literacy. (n.d.). Suicide. (n.d.). Mental Health Literacy.
- Northern Health Indigenous Health. (2016). Declaration on Cultural Safety and Humility. Northern Health Indigenous Health.
- O'Hara, P. Social Inclusion Health Indicators: A Framework for Addressing the Social Determinants of Health. (2006). Homeless Hub.
- O'Neill, A. (2014). Canada - Inflation rate 2014-2024 | Statista.
- Public Health Agency of Canada. (2018). Key Health Inequities In Canada: A National Portrait – Executive Summary Public Health Agency of Canada.
- Public Health Agency of Canada. (2021). CPHO Sunday Edition: The Impact of COVID-19 on Racialized Communities.
- Public Health Agency of Canada. (2019). Prevalence of Chronic Diseases Among Canadian Adults. (2019). Public Health Agency of Canada.
- Public Service Commission of Canada. (2016). Employment Equity. Public Service Commission of Canada.
- Statistics Canada (2023, February). Building construction price indexes, percentage change, quarterly.
- Statistics Canada. (2022). Criminal Victimization of First Nations, Métis and Inuit people in Canada, 2018 to 2020.
- Statistics Canada. (2020). Economic Impact of COVID-19 among Indigenous People.
- Statistics Canada (2023, January, 6). Employment by Indigenous group and occupation.
- Statistics Canada. (2017, October 25). First Nations population by provinces and territories, Canada, 2016.
- Statistics Canada. (2022). Housing conditions among First Nations people, Métis and Inuit in Canada from the 2021 Census.
- Statistics Canada. (2022). Indigenous Peoples – 2021 Census Promotional Material. (2022).
- Statistics Canada. (2021). Projections of the Indigenous populations and households in Canada, 2016 to 2041.
- Statistics Canada. (2022, September 21). The Daily — Indigenous population continues to grow and is much younger than the non-Indigenous population, although the pace of growth has slowed.
- Statistics Canada. (2019, June 28). Suicide among First Nations people, Métis and Inuit (2011-2016): Findings from the 2011 Canadian Census Health and Environment Cohort (CanCHEC).
- Treasury Board Secretariat of Canada. (2023). Departmental Results Report Summary.
- Treasury Board Secretariat of Canada. (2023). GC InfoBase.
- Women and Gender Equality Canada. (2022). Gender-based Analysis Plus (GBA Plus).
- World Health Organization. (n.d.). Social Determinants of Health.