Evaluation of the Healthy Living Program
ISC Evaluation
September 28, 2022
PDF Version (918 Kb, 82 pages)
Table of contents
- List of Acronyms
- Executive Summary
- Management Response and Action Plan
- 1.0 Introduction
- 2.0 Healthy Living Program Overview
- 3.0 Evaluation Methodology
- 4.0 Key Findings: Relevance
- 5.0 Key Findings: Effectiveness
- 6.0 Key Findings: Efficiency
- 7.0 Key Findings: Sub-programs
- 8.0 Summary of Best Practices & Lessons Learned
- 9.0 Cross Cutting Themes
- 10.0 Conclusions
- 11.0 Recommendations
- Appendix A: Evaluation Issues and Questions
- Appendix B: Logic Model
- Appendix C: Logic Model Mapping
- Appendix D: Summaries of Sub-Programs
- Aboriginal Diabetes Initiative (ADI)
- Canada's Tobacco Strategy (CTS)
- Nutrition North Canada Nutrition Education Initiatives (NNCNEI)
List of Acronyms
- ADI
- Aboriginal Diabetes Initiative
- CBRT
- Community-Based Reporting Template
- CHP
- Community Health Plans
- CIRNAC
- Crown-Indigenous Relations and Northern Affairs Canada
- CTS
- Canada's Tobacco Strategy
- FNIGC
- First Nations Information Governance Centre
- FNIHB
- First Nations and Inuit Health Branch
- FTCS
- Federal Tobacco Control Strategy
- HC
- Health Canada
- HL
- Healthy Living
- ISC
- Indigenous Services Canada
- KII
- Key Informant Interview
- MRAP
- Management Response and Action Plan
- NIDA
- National Indigenous Diabetes Association
- NNC
- Nutrition North Canada
- NNCNEI
- Nutrition North Canada Nutrition Education Initiatives
- PHAC
- Public Health Agency of Canada
- RHS
- Regional Health Survey
- SDOH
- Social Determinants of Health
- TB
- Treasury Board
Executive Summary
The overall purpose of the evaluation is to examine the Healthy Living Program (HL) and its constituent programs, as outlined in the Five Year Evaluation Plan at Indigenous Services Canada (ISC), and further to the Treasury Board (TB) Policy on Results.Footnote 1 The evaluation was undertaken to provide a neutral, evidence-based assessment on the following domains: relevance, effectiveness, and efficiency of the HL Program managed by the First Nations and Inuit Health Branch, ISC (FNIHB-ISC). The program includes: the Aboriginal Diabetes Initiative; Canada's Tobacco Strategy (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component);and Nutrition North Canada Nutrition Education Initiatives. The policy areas within the HL program: Nutrition, Chronic Disease Prevention, and Injury Prevention were not included in this evaluation. The evaluation also sought to highlight best practices, challenges, lessons learned, and recommendations to strengthen the HL Program and its sub-programs. It also presents findings in the context of climate change, service transfer, and early impacts of the COVID-19 pandemic on the HL Program.
Background
The Healthy Living Program funds and supports culturally relevant community-based health promotion and disease prevention programs and services in First Nations and Inuit communities. Activities include promoting healthy behaviours and creating supportive environments in the areas of healthy eating, food security, physical activity, tobacco use, and chronic disease prevention, management and screening.
This evaluation focuses on the Healthy Living Program and its constituent programsFootnote 2, hereafter referred to as sub-programs:
- Aboriginal Diabetes Initiative (ADI) aims to reduce type 2 diabetes in First Nations and Inuit communities through health promotion and disease prevention programs, services and activities delivered by community diabetes workers and health service providers.
- Canada's Tobacco Strategy (CTS)Footnote 3 - The Federal Tobacco Control Strategy (FTCS) – First Nations and Inuit component was a knowledge development initiative that began in 2014-15 and continued through the timeframe of this evaluation. It supported the development and implementation of comprehensive, holistic, culturally appropriate tobacco control projects that were focused on reducing non-traditional tobacco use, while maintaining respect and recognition for traditional forms and uses of tobacco within communities.
- Nutrition North Canada (NNC) Nutrition Education Initiatives funded through ISC support culturally appropriate retail and community-based nutrition education activities in eligible isolated northern First Nations and Inuit communities. Activities focus on increasing knowledge of healthy eating and developing skills in the selection and preparation of healthy store-bought and traditional food.
Evaluation Scope and Methodology
This evaluation covers the period from Fiscal Year 2013-14 to 2018-19 further to the Treasury Board requirements and includes each of the three Healthy Living sub-programs managed by FNIHB-ISC. The evaluation was undertaken to provide a neutral and evidence-based assessment of relevance, effectiveness, efficiency, lessons learned, and best practices, for the following activities: Aboriginal Diabetes Initiative, Canada's Tobacco Strategy, and Nutrition North Canada Nutrition Education Initiatives. Moreover, although not part of the original scope, the evaluation also incorporated more recent data and actions taken by ISC to address additional factors impacting programming, especially in the context of service transfer, climate change, and the COVID-19 pandemic.
The evaluation focused solely on First Nations communities. Due to a request by Inuit Tapiriit Kanatami for a distinctions-based approach for conducting evaluations, the Inuit element of the Healthy Living Program will be evaluated at a date to be determined.
The evaluation was conducted in-house by the ISC Evaluation Directorate. It relied on a mixed-methods approachFootnote 4 that included the following lines of evidence: a document and literature review; 19 key informant interviews with FNIHB-ISC staff (including national and regional office staff); 1 key informant interview with non-ISC government staff; 9 key informant interviews with Indigenous partner organizations (Tribal Councils, First Nations Health Service Organizations, etc.); 1 key informant interview with a non-Indigenous partner organization; 2 key informant interviews with representatives from First Nation communities and; an online survey of 168 individuals working in/with First Nations communities.Footnote 5
As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were not possible and were instead replaced by remote video/telephone interviews through various communication platforms.
Main Findings
Relevance:
The program remains relevant as the Regional Health Survey, conducted by the First Nations Information Governance Centre, reported that nearly three-fifths (59.8%) of First Nations adults reported having at least one known chronic health condition.Footnote 6 The federal government has a clear mandate to continue to address the greater risks and lower health outcomes associated with chronic diseases among First Nations individuals, families and communities. Budget 2018 laid out the renewal of the Tobacco Strategy, highlighted the significant gaps in health outcomes between Indigenous and non-Indigenous people, and highlighted the higher diabetes prevalence rate faced by Indigenous peoples. Additionally, Budget 2016 allocated funds to expand NNC, to support all isolated northern communities.
Effectiveness:
One of the strengths of the Healthy Living Program lies in its design and delivery model being unique to each community, allowing for communities to define their own needs and priorities. As a result of the diversity that exists in programming across communities and in targeted activities, it is difficult to determine if the program is effectively reaching all community members in all regions it operates in. It was noted that in key informant interviews that although harder to reach groups were not excluded from programming, it was unclear if all or most communities are engaging in tailored strategies to specific demographics (working age population, 2SLGBTQIA+ peoples, or at-risk youth). A concern noted by key informant respondents regarding some harder to reach clientele, includes programming activities implemented during standard operating hours, making it difficult for the working age population to attend activities during the day.
The majority of key informant interview respondents did not feel there were particular groups being left out of programming, there was also limited description of strategies or targeted programming for harder to reach populations which may be due to the fact that key informant interview respondents were not involved in delivering programs directly at the community level.
The HL sub-programs, particularly the Aboriginal Diabetes Initiative (ADI) and the NNC Nutrition Education Initiatives, complement each other well. Some survey respondents noted that since staff members were often responsible for multiple Healthy Living sub-programs there was inherently collaboration. There are many linkages with other government programs outside of Healthy Living (e.g., Non-Insured Health Benefits program) and with partner organizations. For example, across Federal government departments, the HL Program works with Health Canada for Canada's Tobacco Strategy and with Crown-Indigenous Relations and Northern Affairs Canada (CIRNAC) for Nutrition North Canada. The FNIHB National Office works and collaborates with both the Assembly of First Nations (AFN) and Inuit Tapiriit Kanatami (ITK) to inform the Healthy Living program.
However, a consistent challenge faced by the evaluators was the lack of available and adequate data to properly assess the achievement of the program's progress towards immediate and intermediate outcomes. With the program requiring less detailed reporting from communities as a result of diverse funding agreements, there is often an absence of specific and robust program performance data to effectively speak to the program's stated outcomes. Evaluations can help to fill this void by collecting additional data, both qualitative and quantitative, as feasible. Part of the challenge for this evaluation was due to the fact that the evaluation was conducted during the COVID-19 pandemic. This directly impacted the evaluation's team ability to conduct site visits and engage communities in a more fulsome manner.
Efficiency:
The most consistently reported challenge from partners and ISC national and regional staff across all sub-programs is a lack of funding particularly in the human resource areas. Funding constraints have a negative impact on recruiting and retaining the right community-level talent, and access to professional development training opportunities are limited. Funding has been stagnant (i.e., not keeping up with inflationary pressures, and the increased needs of the Program) for many years, leading to unmet needs of the program and little to no increase in salaries at the community levels, contributing to high turnover rates, and vacant positions.
Collection of data on indicators for the HL Program is primarily the responsibility of individual communities under the FNIHB funding agreements between FNIHB and individual communities. However, while some communities report on health-related indicators, not all communities do report, or report to the full extent. Throughout interviews, key informants expressed the importance of collecting and utilizing the community-based reporting template (CBRT)Footnote 7 to not only fulfil funding requirements, but also to provide a snapshot of the community's health and well-being in order to tailor community health priorities. There is also an expressed need from partner organizations to further improve the CBRT, as it does not collect information at a sufficiently detailed level for communities to effectively track performance and achievement of results.
Aboriginal Diabetes Initiative:
Since the 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development programs, this evaluation has found that overall, considerable progress has been made to suggest that the ADI has delivered meaningful results in community-based health promotion and primary prevention. However, according to the First Nations Information Governance Centre (FNIGC), "nearly three-fifths (59.8%) of First Nations adults, one-third (33.2%) of First Nations youth, and more than one-quarter (28.5%) of First Nations children have reported having one or more chronic health conditions. Among First Nations children, the number of reported conditions shows a significant decrease from the Regional Health Survey (RHS) Phase 2 (2008/10)."Footnote 8 Of note is that diabetes continues to remain to be the most noted chronic health condition reported by the FNIGC among First Nations adults.
Strong efforts were also made by communities to bring attention to traditional physical activities and reducing sedentary time, which can prevent and/or reduce chronic diseases such as type 2 diabetes. However, there exists varying gaps in the level of screening and management effectiveness across regions.
Key informant interview respondents noted that communities lack proper screening tools, such as access to specimen collection and lab licensure, as well as access to provincial health data.Footnote 9 As well, current capacity building and training efforts are on-going for staff supporting the ADI. Specifically, both key informant interview respondents and survey respondents are interested in building their own capacity to better support clients and families with managing and improving their mental health. They are both also interested in having access to training that goes beyond the biomedical component of type 2 diabetes. The engagement of regional partners at their respective regional community of practice groups, which key informant interview respondents have referred to as "working groups" has been successful.
The evaluation notes a few key challenges that may hinder the ADI from potentially meeting needs and priorities, including the impact of funding constraints, staffing challenges, technological disadvantages faced by some clients, and the impact of food insecurity.
Canada's Tobacco Strategy:
As of 2017-18, under the FTCS, 56% of First Nations and Inuit communities had access to tobacco control activities.Footnote 10 A number of successes were demonstrated, for example: a doubling in the number of indoor and outdoor smoke-free spaces in communities; 173 new smoking-related resolutions passed at the local level; increased participation of community members in smoking cessation programs/interventions, with the overall smoking cessation rate surpassing estimated cessation rate among other segments of the general Canadian population.Footnote 11
The survey indicated that 53% of respondents agreed or strongly agreed that Canada's Tobacco Strategy was operating effectively to reduce commercial tobacco use. Through key informant interviews, cessation efforts were identified as being a major challenge. Survey respondents also noted major challenges in retaining staff, promoting community engagement, and engaging individuals before they begin smoking. In addition, given the important cultural and spiritual roots of tobacco in many First Nations practices, tobacco cessation research has shown that culturally appropriate interventions bolster the effectiveness of Indigenous tobacco programming.
Nutrition North Canada (NNC) Nutrition Education Initiatives:
The recent Horizontal Evaluation of NNC found that nutrition education initiatives funded through FNIHB were a key successFootnote 12. The growth in participation in community-based nutrition education initiatives demonstrates that more people are acquiring knowledge and skills to eat healthy. The evaluation also found that there is a higher demand for certain types of activities such as traditional food knowledge and skills, as well as retail-based nutrition knowledge and awareness.
Many key informant interview respondents and survey respondents expressed concerns around the eligibility for Nutrition Education Initiatives. Funding is currently dependent on the First Nations community meeting eligibility criteria for the NNC subsidy administered by CIRNAC. While the nutrition education initiatives function as a component of Nutrition North Canada, key informant interview respondents expressed that nutrition education remains relevant for all communities and expressed that the current eligibility criteria does not meet the needs of many communities. Survey and key informant interview respondents also expressed concerns about inadequacy in funding for Nutrition Education Initiatives given the high prices of food in the north and the travel expenses for community health workers that service multiple communities.
Climate Change:
The effects of climate change on the HL Program are potentially significant, especially in the context of remote and isolated communities. There are two elements to consider in terms of climate change effects as they related to the Healthy Living Programs: impacts on the food supply chain, and changes in the availability of traditional or country foods as a result of changes to the environment and ecosystems (e.g., animal migration pattern changes, temperatures changes, extreme weather conditions such as fires and floods). Both of these elements have the potential to impact the availability of nutritious foods that are important elements of the ADI and NNC Nutrition Education Initiatives, as well as food security itself in remote, isolated and northern communities.
Climate change has an impact on food security, and as a result can impact the HL Program. Many community-based activities supported through HL sub-programs seek to improve access to and availability of nutritious food, for example by incorporating healthy store bought and traditional foods, and supporting gardening activities. Survey respondents and key informant interview respondents noted that climate change is causing a less reliable food supply chain, as once reliable ice roads used for transport of foodstuffs are increasingly impassable or are in operation for a shorter period of time due to late freeze-up/ early melting. Additionally, changes in animal migration patterns, extreme weather conditions and temperature changes have had an impact on the local availability of plants and animals therefore increasing food security challenges.
Service Transfer:
Many communities across all regions are incrementally moving towards flexible funding arrangements and while this is a positive step in the service transfer continuum, there remain hurdles to transferring financial responsibilities to communities directly. Most significantly, key informant interview respondents cited that the role that ISC provides in terms of financial oversight (i.e., management tools, databases, etc.) is not yet being transferred to community health directors and staff, which is an important administrative aspect of service transfer. This factor impedes the ability of ISC regional offices to adapt to changing community need-based priorities.
Best Practices:
The evaluation presents several best practices that were highlighted by ISC key informant interview respondents both at national and regional offices. Of the list of best practices presented in the evaluation, these initiatives stood out: the inclusion of traditional tobacco practices and land-based activities; the establishment of intra-regional ADI working groups, regional-specific; and various best practices such as regional diabetes coordinators and food security coordinators. As well, the evaluation compiled general guiding principles as shared by key informant interview respondents with regards to lessons learned in community programming design.
Early Impacts of COVID-19:
Although not within the original scope, the evaluation investigated the early impacts of the COVID-19 pandemic on the Healthy Living Program. COVID-19 health restrictions heavily impacted the undertaking of this evaluation. In particular, the resultant travel-restrictions affected the evaluation team's inability to conduct site visits and directly interview end-users. As well, the availability of respondents (both survey respondents and key informant interviews) was another limiting factor. This is important contextual information to better understand how the program has evolved to address the challenges and stresses brought upon by COVID-19. All evaluations conducted during the timeframe of March 2020-2021, have included early impacts of COVID-19 on programming. Future evaluations will endeavour to look at the full breadth of Covid-19 impact. Key informant interview respondents addressed the following themes in the context of COVID-19: effects on planned Healthy Living activities; challenges relating to the sub-programs; and any unintended impacts as a consequence of ISC's COVID-19 pandemic response. The effects of the COVID-19 pandemic on the Healthy Living program, and associated sub-programs, have been notable. COVID-19 brought several challenges to HL Program delivery, including pivoting activities to online platforms. While this has caused access and participation challenges for some community members, it has also allowed for various clients who would not otherwise attend targeted activities to participate in online activities.
Recommendations:
Based on the findings of this evaluation report, it is recommendedFootnote 13 that ISC:
- Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus); and gradual service transfer.
- ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer.
- Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program.
- Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level.
Management Response and Action Plan
Project Title: Evaluation of the Healthy Living Program
1. Management Response
Indigenous Services Canada, First Nations and Inuit Health Branch (ISC-FNIHB) acknowledges and concurs and/or partially concurs with the recommendations outlined in the report of the evaluation of the Healthy Living Program conducted by Indigenous Services Canada's Evaluation Directorate.
For all recommendations, ISC-FNIHB recognizes the importance of committed and dedicated action towards self-determination of Indigenous Peoples and towards service transfer. ISC-FNIHB is supporting First Nations to influence, manage and increase control over health programs and services that affect them and improve access to quality health services. While supporting these shifts, ISC-FNIHB continues to work with First Nations partners and communities in advancing their priorities, for example, supporting training and capacity building efforts in regions, and facilitating access or linkages to healthy living services, supports and resources (e.g., nutrition, food security). We will work with partners to examine options for sustainability of funding, incorporating traditional practices and knowledge transfer of best practices. ISC-FNIHB is committed to actively participating in discussions with First Nations partners, including the Assembly of First Nations, to determine where we go from here as a collective to address these issues.
ISC-FNIHB recognizes that persistent data gaps undermine overall health and wellness as well as effective service delivery across the Department. Data challenges exist within the program and this is a broader challenge across the sector. Addressing data challenges is a cross-cutting, interconnected issue and is a priority of the whole Department. Therefore, ISC-FNIHB partially agrees with Recommendation 1 as an individual program only holds some of the levers towards implementing this recommendation. We will undertake incremental work in the development of a data strategy outlined in Recommendation 1, to improve the availability of Healthy Living performance data at the community, regional and national levels. We will direct our efforts to undertake a gaps analysis and update the data collection instruments for Healthy Living aligning to the Departmental Results Framework. We will work within current Departmental efforts to ensure a cohesive and unified approach to First Nation data across all ISC sectors. This approach aligns with ISC's current mandate, which is predicated on the understanding that Indigenous control leads to better outcomes for Indigenous Peoples, and data is no exception.
It is important to note that this evaluation covers the period from Fiscal Year 2013-14 to 2018-19. As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were instead replaced by remote video/telephone interviews through various communication platforms using a mixed-method approach. The Department recognizes that this evaluation was undertaken during the height of the COVID-19 pandemic, when many Healthy Living programs and services were reduced or paused, and funding recipients/communities diverted resources to help address critical pandemic-related needs. Ultimately, the timing of the evaluation process significantly limited participation in this evaluation, especially at the community level. As regular programming and services begin to ramp up, ISC-FNIHB will build on what was heard during the evaluation by working with its First Nations partners and communities to identify needs and supports required to resume and strengthen programming.
The evaluation report identifies several cross-cutting topics such as service transfer and performance measurement, which implicate not only the Healthy Living Program but the Department as a whole. With this in mind, the Action Plan is focused on collaboration with First Nations partners, ISC sectors and other federal departments.
ISC-FNIHB intends to initiate implementation of the recommendations immediately. An annual review of the Management Response and Action Plan will be conducted by
ISC Evaluation and shared with the ISC Performance Management and Evaluation Committee (PMEC) to monitor progress and activities.
| Recommendations | Actions | Responsible Manager (Title / Sector) |
Planned Start and Completion Dates | |
|---|---|---|---|---|
| 1. Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus); and gradual service transfer. | We __partially__ concur. (do, do not, partially) |
Dr. Tom Wong, Chief Medical Officer and Director General, Office of Population and Public Health (OPPH), First Nations and Inuit Health Branch (FNIHB), Indigenous Services Canada (ISC) Robin Buckland, Chief Nursing Officer, Director General, Office of Primary Health Care, FNIHB, ISC |
Start Date: October 2022 |
|
| ISC-FNIHB partially concurs with this recommendation as this is a sector-wide issue and aligns with broader Departmental efforts to transform the existing approach to Indigenous data across all sectors (e.g., health, education, child and family services). ISC-FNIHB will
Action 1.1: Undertake scoping and gaps analysis of data used for Healthy Living Program. (Q1 2023-24) Action 1.2: Engage Indigenous expert(s) to advise on indicators for Healthy Living related outcomes. (Q2 2023-24) Action 1.3: Develop Options for updating Healthy Living indicators and Data Collection Instruments. (Q3 2023-24) Action 1.4: Update Performance Information Profiles and Data Collection Instruments for Healthy Living. (Q4 2023-24) |
Completion: March 31, 2024
|
Status: As of: (September 16, 2022) |
||
| 2. ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer. | We __do___ concur. (do, do not, partially) |
Dr. Tom Wong, Chief Medical Officer and Director General, Office of Population and Public Health (OPPH), First Nations and Inuit Health Branch (FNIHB), Indigenous Services Canada (ISC) Robin Buckland, Chief Nursing Officer, Director General, Office of Primary Health Care, FNIHB, ISC |
Start Date: |
|
To support this recommendation, the Healthy Living Program will:
|
Completion:
|
Status: As of: (Insert Update Here) |
||
| 3. Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program. | We __do___ concur. (do, do not, partially) |
Dr. Tom Wong, Chief Medical Officer and Director General, Office of Population and Public Health (OPPH), First Nations and Inuit Health Branch (FNIHB), Indigenous Services Canada (ISC) | Start Date: October 2022 |
|
To support this recommendation, the Healthy Living Program will:
|
Completion:
|
Status: As of: (Insert Update Here) |
||
| 4. Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level. | We __do__ concur. (do, do not, partially) |
Dr. Tom Wong, Chief Medical Officer and Director General, Office of Population and Public Health (OPPH), First Nations and Inuit Health Branch (FNIHB), Indigenous Services Canada (ISC) | Start Date: October 2022 |
|
To support this recommendation, the Healthy Living Program will:
|
Completion:
|
Status: As of: (Insert Update Here) |
1.0 Introduction
The overall purpose of the evaluation was to examine the Healthy Living Program and its constituent sub-programs, as outlined in the Five Year Evaluation Plan of Indigenous Services Canada (ISC), further to the Treasury Board (TB) of Canada Policy on Results. The evaluation focused on the following three sub-programs of the Healthy Living Program suite: Aboriginal Diabetes Initiative (ADI), Canada's Tobacco Strategy (CTS) (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component), and Nutrition North Canada (NNC) Nutrition Education Initiatives. The Healthy Living Program and its sub-programs are supported and delivered through the First Nations and Inuit Health Branch (FNIHB) within ISC.Footnote 14 The evaluation covers the fiscal years 2013-14 through 2018-19, but also includes program activities undertaken from April 2019 up to and including fiscal year 2019-20.Footnote 15 The total funding allocated to the HL Program (including sub-programs and policy areas) from 2013-14 to 2018-19 was approximately $426 million.
2.0 Healthy Living Program Overview
2.1 Program Description
The Healthy Living Program funds and supports culturally relevant community-based health promotion and disease prevention programs and services in First Nations and Inuit communities. Activities include promoting healthy behaviours and creating supportive environments in the areas of healthy eating, food security, physical activity, tobacco, and chronic disease prevention, management and screening. The Healthy Living Program evaluation focuses on the three sub-programs:Footnote 16 ADI, CTS, and NNC Nutrition Education Initiatives. The policy areas within Healthy Living of Nutrition, Chronic Disease Prevention and Injury Prevention were not included in the evaluation.
Aboriginal Diabetes Initiative (ADI)
The ADI aims to reduce the prevalence of type 2 diabetes in First Nations and Inuit communities. ADI funding supports community-led health promotion and disease prevention programming, services and activities delivered by community workers and health service providers. During the time frame of this evaluation, ADI was the only sub-program within the Healthy Living Program funded universally, with all communities having access to ADI funding. The program consists of four components:
- Community-based health promotion and primary prevention;
- Screening and management;
- Capacity building and training; and,
- Knowledge mobilization.
The ADI program activities offered in each community vary based on local needs, priorities and capacity.
Canada's Tobacco Strategy (CTS)Footnote 17
The First Nations and Inuit component of the Federal Tobacco Control Strategy (FTCS) was a project-based knowledge development initiative that began in 2014-15 and continued through the timeframe of this evaluation. The FTCS provided proposal-based funding that supported the implementation of 16 projects and 3 strategies, reaching approximately 56% of First Nations and Inuit communities. The FTCS supported the development and implementation of comprehensive, holistic, culturally appropriate tobacco control projects that focused on reducing commercial tobacco use, while maintaining respect and recognition for traditional forms and ceremonial uses of tobacco within First Nation communities. The FTCS was guided by the World Health Organization's Framework Convention on Tobacco Control, and included a comprehensive approach to tobacco control, organized around 6 essential intervention elements, which included: 1) protection; 2) reducing access to tobacco products; 3) prevention; 4) education; 5) cessation, and; 6) research and evaluation.
The projects actively participated in a community of practice, a forum to share knowledge, lessons learned, successes/promising practices towards the reduction of commercial tobacco.
A case study with early findings of the First Nations and Inuit Component of the FTCS (from 2014-15 and 2015-16) was included in the evaluation of the FTCS horizontal initiative that was completed by the Office of Audit and Evaluation of Health Canada and the Public Health Agency of Canada in 2017Footnote 18.
The FTCS was renewed in 2018 and renamed Canada's Tobacco Strategy (CTS). CTS is a Health Canada-led comprehensive strategy to help Canadians who smoke to quit or reduce the harms of their addiction to nicotine and protect the health of young people and non-smokers from the dangers of tobacco use. The main themes of the renewed CTS are:
- Help Canadians quit tobacco;
- Protect youth and non-tobacco users from nicotine addiction;
- Support Indigenous-led approaches towards reducing commercial tobacco use; and
- Strengthen science, surveillance and partnerships.
Through CTS, ISC provides funding to support Indigenous communities across Canada for the development and implementation of distinct First Nations, Inuit, and Métis approaches to reduce commercial tobacco use. This approach supports self-determination of First Nations, Inuit and the Métis peoples to identify needs and priorities of individuals, families, communities, and supports Indigenous control over culturally appropriate service design and delivery.
Although the evaluation period coincided with the previous FTCS, it will be referred to as the renamed CTS throughout the remainder of the report acknowledging that key differences exist between the strategies in terms of funding distribution and approach.
Nutrition North Canada Nutrition Education Initiatives
Nutrition North Canada is a Government of Canada program that helps make nutritious food and some essential items in isolated eligible northern communities through a retail subsidy and a Harvester's Support Grant delivered through, Crown-Indigenous Relations and Northern Affairs Canada (CIRNAC), and through NNC Nutrition Education Initiatives supported by Indigenous Services Canada (ISC) and the Public Health Agency of Canada (PHAC).
NNC Nutrition Education Initiatives are funded through ISC to support culturally appropriate retail and community-based nutrition education activities in eligible isolated northern First Nations and Inuit communities. Activities focus on increasing knowledge of healthy eating and developing skills in the selection and preparation of healthy store-bought and traditional or country foods. Communities decide which activities to undertake based on their local needs and priorities. NNC Nutrition Education Initiatives were included in the scope of the Horizontal Evaluation of NNC for the fiscal years 2012-13 to 2017-18, published in 2020Footnote 19.
At ISC, FNIHB is responsible to provide the NNC Nutrition Education Initiatives funding and support through the Healthy Living Program to all the First Nations and Inuit communities eligible for the program.
2.2 Program Objectives and Expected Outcomes
The objective of the Healthy Living Program is to address the greater risks and lower health outcomes associated with chronic diseases and injuries among First Nations and Inuit individuals, families, and communities.The following outlines the immediate, intermediate, and ultimate outcomes and objectives of the program, according to the program's logic model:
Immediate Outcomes
- First Nations and Inuit have capacity to support Healthy Living programming.
- First Nations and Inuit have access to Healthy Living programming.
- First Nations and Inuit have knowledge of Healthy Living issues and practices.
Intermediate Outcomes
- First Nations and Inuit are engaged in healthy behaviours.
Ultimate Outcome
- First Nations and Inuit Individuals and communities are healthier.
The logic model for the Healthy Living Program can be found in Appendix B.
In addition, the Healthy Living Program is in alignment with the following Calls to Action released by the Truth and Reconciliation Commission in June 2015Footnote 20:
Call to Action #18: We call upon the federal, provincial, territorial, and Aboriginal governments to acknowledge that the current state of Aboriginal health in Canada is a direct result of previous Canadian government policies, including residential schools, and to recognize and implement the health-care rights of Aboriginal people as identified in international law, constitutional law, and under the Treaties.
Call to Action #19: We call upon the federal government, in consultation with Aboriginal peoples, to establish measurable goals to identify and close the gaps in health outcomes between Aboriginal and non-Aboriginal communities, and to publish annual progress reports and assess long-term trends. Such efforts would focus on indicators such as: infant mortality, maternal health, suicide, mental health, addictions, life expectancy, birth rates, infant and child health issues, chronic diseases, illness and injury incidence, and the availability of appropriate health services.
Call to Action #20: In order to address the jurisdictional disputes concerning Aboriginal people who do not reside on reserves, we call upon the federal government to recognize, respect, and address the distinct health needs of the Métis, Inuit, and off-reserve Aboriginal peoples.
2.3 Program Management and Key Partners
Program Management
FNIHB staff at the National Office within the National Capital Region lead strategic, program policy development and planning in support of the Healthy Living program, working with FNIHB regional offices and First Nations and Inuit partners at the national level (i.e., National Indigenous Organizations). The core responsibilities of the National Office include: program framework design; the national program funding allocations for sub-programs; national program monitoring; data collection and analysis; reporting and evaluation; provision of advice and/or guidance on program delivery; and working with FNIHB Regions and First Nations and Inuit partners to identify and address gaps in Healthy Living programming and services. The National Office may also issue and manage funding arrangements for national partners and stakeholders.
The FNIHB regional offices play a lead role in supporting communities with program delivery by working with First Nations and Inuit partners at the regional and local levels. The regional offices are also responsible for the management of funding arrangements, program performance monitoring, and information roll-ups. With the exception of the Northern Region, regions also support communities with program delivery when needed or requested by funding recipients or communities. There is a wide variation in how each region operates relating to the Healthy Living program. Consequently, the information collected from the regions for this evaluation varied and may not necessarily be comparable from one region to another.
The FNIHB Northern Region works directly with the territorial governments and self-governing First Nations in Yukon and selected communities within Northwest Territories. In Nunavut and the remainder of Northwest Territories, the FNIHB Northern Region works directly with territorial governments to negotiate funding arrangements for health programming, and ensures that First Nations partners are engaged in decision-making. Each territory is responsible to administer the funds to communities and organizations such as First Nations band councils, health authorities, Inuit associations, and voluntary and non-profit organizations. Programming is targeted to the entire population in each territory, not only First Nations. As such, the Healthy Living Program in the North has unique reporting templates used to gather performance measurement information that will be used to support evaluation efforts where applicable.
The communities, Tribal Councils or other Indigenous health organizations are funded through funding arrangements to support the implementation and delivery of the Healthy Living Program. Community or Tribal Council implementation and support is unique and based on the needs, and priorities of the communities or tribal councils/organizations and often includes implementing a variety of healthy living activities, building internal capacity through the hiring, managing and training of community program staff, providing office space and program tools and resources, and working collaboratively with other programs and partners.
Program Partners
First Nations communities are diverse in terms of culture, language, geographical location, population size, health needs, priorities, level of funding from FNIHB, access to provincial health services, and their capacity to manage their own services. As such, communities or Tribal Councils may modify programming to address these factors in order to better meet their specific health priorities and needs. The variations in programming may influence what data is collected as well as the potential impact of the programs and services.
To support program and service delivery, the Healthy Living Program collaborates with a number of other partners and stakeholders. For example, the Healthy Living Program works with:
- Indigenous partners and organizations at national and regional levels; and
- Other FNIHB program and service areas such as Healthy Children, Youth and Families and Mental Wellness; and
- Other federal departments such as Health Canada, Public Health Agency of Canada, Crown-Indigenous Relations and Northern Affairs Canada, and Agriculture and Agri-Food Canada.
FNIHB's Senior Management Committee is the main decision-making forum for the Branch on issues related to policy development and priority setting. It includes representation from senior management at national office and regional offices and representatives from the Assembly of First Nations (AFN) and Inuit Tapiritiit Kanatami (ITK).
3.0 Evaluation Methodology
3.1 Scope and Evaluation Issues
This evaluation covers the period from Fiscal Year 2013-14 to 2018-19 further to the Treasury Board requirements and includes each of the three Healthy Living sub-programs managed by FNIHB-ISC. The evaluation was undertaken to provide a neutral and evidence-based assessment of relevance, effectiveness and efficiency of the Healthy Living Program, including, Aboriginal Diabetes Initiative, Canada's Tobacco Strategy (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component), and Nutrition North Canada Nutrition Education Initiatives. The evaluation also sought to highlight best practices, challenges, lessons learned and recommendations to strengthen the Healthy Living Program and its sub-programs. The policy areas within Healthy Living of Nutrition, Chronic Disease Prevention and Injury Prevention were not included in this evaluation. Moreover, although not part of the original scope, the evaluation also incorporates more recent data and actions taken by ISC to address additional factors impacting programming, especially in the context of service transfer, climate change and the COVID-19 pandemic.
The evaluation focused solely on First Nations communities. Due to a request by Inuit Tapiriit Kanatami for a distinctions-based approach for conducting evaluations, the Inuit element of the Healthy Living Program will be evaluated at a date to be determined. Additionally, as responsibilities for federal health programs have been transferred to the First Nations Health Authority through the British Columbia Tripartite Framework Agreement on First Nation Health Governance, British Columbia does not fall within the scope of the evaluation.
The evaluation was conducted through the lenses of Gender Based Analysis Plus (GBA Plus) and the federal commitment to Truth and Reconciliation with Indigenous Peoples. The evaluation includes the above Healthy Living activities and initiatives undertaken in all jurisdictions across Canada, with the exception of British Columbia, and to a limited extent in the North, as outlined above.
3.2 Evaluation Design and Methods
The evaluation was conducted in-house by the ISC Evaluation Directorate. It relied on a mixed-methods approach that included the following lines of evidence:
- A document and literature review;
- Key Informant Interviews:
- 19 key informant interviews with FNIHB-ISC staff (including national and regional office staff);
- 1 key informant interview with non-ISC government staff;
- 9 key informant interviews with Indigenous partner organizations (Tribal Councils, First Nations Health Service Organizations, etc.);
- 1 key informant interview with a non-Indigenous partner organization;
- 2 key informant interviews with representatives from First Nation communities; and;
- Online Survey:
- an online survey of 168 individuals working in/with First Nations communities. Of the survey respondents who responded to the question on what their role was in the Healthy Living Program, 80% identified themselves as the following, in descending order of frequency: community health workers, health directors/managers, dietitians/nutritionists, and nurses. A variety of roles were mentioned by the remaining 20%, including mental wellness workers, social workers and a range of other roles, with each being mentioned by only one individual.)
As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were not possible and were instead replaced by remote video/telephone interviews through various communication platforms. The pandemic also directly impacted the evaluators' ability to interview community partners. Given that many community partners were involved in the response to COVID-19, the evaluators were unable to fully engage them as planned. However, partner responses were given heavy weight when reporting results.
3.3 Limitations
Table 1 below outlines the limitations encountered during the implementation of the selected methods for this evaluation and the corresponding mitigation strategies that the evaluation team utilized to ensure that the evaluation findings are reliable and have been validated.
| Limitation | Mitigation Strategy |
|---|---|
| An important limitation of this evaluation is that the program performance data only partially provides outcome level data and reporting requirements vary across communities. As a result, there is a lack of available comprehensive and consistent program performance data at the immediate and intermediate levels. In addition, there is a lack of data that would allow for the monitoring and analysis of GBA Plus. | The evaluation sought to collect primary data as best it could, given the significant data collection constraints during the COVID-19 emergency response. Where possible, the evaluators also utilized available secondary data. Evaluations rely heavily on program performance data as a foundational source of evidence to assess program effectiveness. Evaluations triangulate performance data with other primary and secondary sources of qualitative and quantitative data to formulate objective, fact-based findings and recommendations. |
| The COVID-19 pandemic prevented travel to communities, and subsequently there was limited ability to conduct site visits to both regions and communities. This resulted in an inability to collect data from end-users/clients of HL programming, which in turn resulted in the use of secondary data, for example the Regional Health Survey, which provides a holistic picture of program results, but it is not specifically focussed on the HL program. | The evaluation team conducted virtual interviews with key informants at several different levels of the program: national office, regional office and at the community level where sub-programs are implemented. As well, the evaluation team distributed an electronic survey which received responses from all regions involved in the HL Program across Canada. |
| As a result of the COVID-19 pandemic, there were fewer responses in key informant interviews and the online survey from respondents that were supporting the CTS and NNC sub-programs. | Additional secondary data was utilized to complement survey responses and provide further analysis. |
| This evaluation took place during the transition from projects under the previous project based FTCS – First Nations and Inuit Component to the current CTS with funding integrated with other Healthy Living funding and which also has coincided with the COVID-19 pandemic. | The evaluation acknowledges that the First Nations and Inuit component of the Federal Tobacco Control Strategy was a knowledge development initiative that began in 2014-15 under the FTCS and continued through the timeframe of this evaluation in 2018-19. Thus, given the transition, the scope of this evaluation does not capture the renewed CTS, announced in Budget 2018. |
| Owing either to the COVID-19 pandemic or for other reasons including perhaps a stronger ADI presence in communities, there was limited online survey engagement from First Nations communities supporting the CTS and NNC.Footnote 21 | ISC national and regional offices were included as units of analysis to provide further analysis where there was limited CTS and NNC survey engagement. |
3.4 Indigenous Engagement
The evaluation employed FNIHB-ISC's engagement protocol, which calls for National Indigenous Organizations (in this case, the Assembly of First Nations) to review evaluation documentation at various stages of the process (methodology report, preliminary findings, and draft evaluation report) and comment/provide suggestions on the evaluation methodology, questions to be asked to help promote culturally appropriate evaluations for FNIHB programs. Additionally, regional Indigenous partners (e.g. health partnership tables, tribal councils) were engaged by FNIHB-ISC regional offices on a less-formal basis to provide supplementary input on community selection and evaluation methodology, which was then shared with the evaluation team.
3.5 Organization of the Findings
While this evaluation viewed the Healthy Living Program as a holistic entity, the key focus was, to a greater extent, on the performance of each of the three individual sub-programs, as there is little overlap amongst them from a management and operational perspective. For example, ADI is universally funded, whereas the NNC Nutrition Education Initiatives target eligible isolated northern communities. Also in contrast, with the transition from the FTCS to CTS, there was a switch from project-based funding to on-going funding. Of note is that a greater number of survey respondents acknowledged being involved with ADI than with either the CTS or NNC Nutrition Education Initiatives. As such, many of the evaluation's findings are sub-program-specific, as opposed to program-wide. Findings 1-11 may be considered to cross-cut two or more Healthy Living sub-programs, while the remainder are specific to each of the three sub-programs.
4.0 Key Findings: Relevance
4.1 Program Relevance
Finding 1: The Healthy Living Program remains relevant. Current and ongoing health issues contributing to the need for the Healthy Living Program include: deep rooted health inequities faced by First Nation communities and the impact of the social determinants of health on programming.
The Healthy Living Program continues to remain relevant as the Regional Health SurveyFootnote 22 conducted by the First Nations Information Governance Centre (FNIGC), reported that "nearly three-fifths (59.8%) of First Nations adults, one-third (33.2%) of First Nations youth, and more than one-quarter (28.5%) of First Nations children have reported having one or more chronic health conditions. Among First Nations children, the number of reported conditions shows a significant decrease from the RHS Phase 2 (2008/10)."Footnote 23 Of note is that diabetes continues to remain to be the most noted chronic health condition reported by the FNIGC among First Nations adults.
In July 2018, Diabetes Canada released their Diabetes 360 Report: A Framework for a Diabetes Strategy for CanadaFootnote 24, highlighting the significant health-crisis impacting close to 11 million Canadians that are living with prediabetes or diabetes. The Report states that, "for First Nations peoples, the risk of being diagnosed with diabetes is up to 80% and in some subgroups within this population, it is even higher."Footnote 25 For example, diabetes prevalence is 3-5 times greater for First Nations peoples living on-reserve, than non-First Nations Canadians. In addition, the rates of complications from diabetes are also higher for First Nations on-reserve than non-First Nations Canadians.Footnote 26 In contrast to the general Canadian population (in which the prevalence is predominately higher in men than women), First Nations women bear a heavier diabetes burden than First Nations men, across most age groups. In fact, Indigenous individuals that are diagnosed at an increasingly younger age, have greater severity at diagnosis, and experience poorer treatment outcomes in comparison to the general Canadian population."Footnote 27
Prevalence of smoking amongst First Nations adults also remains relatively high, with the Regional Health Survey Phase 3 reporting that more than half (53.5%) of First Nations adults smoked cigarettes, with 40% saying they smoked on a daily basis.Footnote 28 Phase 2 of the Regional Health Survey reported that 56.9% of First Nations adults smoked cigarettes.Footnote 29 While this presents a small decrease in use, the three phases of the Regional Health Survey reported relatively stable prevalence of smoking in First Nations adults.Footnote 30 Comparatively, 14.8% of the general Canadian population smoke.Footnote 31
In addition to the high prevalence rates of diabetes and smoking, three factors that contribute to the disproportionate health inequities in First Nations communities are notable. First, health inequities are deeply rooted in the historical relationship between First Nations communities and the health systems. In particular, the impacts of colonization have resulted in "a legacy of environmental dispossession, degradation of the land, substandard living conditions, inadequate access to health services, social exclusion and a dislocation from community, language, land and culture. These policies have been clearly linked to adverse health consequences for individuals and community."Footnote 32
Second, the complex, inter-related nature of social determinants of health contributes to the serious health challenges that many First Nations communities continue to face. The Public Health Agency of Canada (PHAC) recognizes that health is determined by the complex inter-related nature of social determinants of health between social and economic factors, the physical environment and individual behaviour. PHAC has identified twelve social determinants of health: gender, culture, health services, income/social status, social support networks, education/literacy, employment and working conditions, social environments, physical environments, personal health practices and coping skills, healthy child development, and biology/genetic endowmentFootnote 33. In fact, 70% of online survey respondents either agreed or strongly agreed, that the Healthy Living sub-programs paid appropriate attention to integrating various social determinants of health, such as income, education level, and the physical environment Examples of this include: the HL Program taking into consideration different income levels when recommending healthy food purchases to clients, introducing targeted education activities to various age groups (elementary students, high school students etc.) and recommending physical activities that are available to those individuals living on-reserve.
Lastly, the inequitable distribution of economic resources combined with other social determinants of health has further contributed to food insecurity challenges faced by First Nations communities. Food insecurity challenges can be linked to the inadequate intakes of several nutrients, likely contributing to the disproportionate health inequities faced by First Nations communities. The First Nations Food Nutrition and Environment Study (2008-2018)Footnote 34, found that, on average across all regions, 37% of all participating households on-reserve were food insecure, while regional prevalence ranged from 30.8% to 45.5% or up to more than 5 times higher than the prevalence of household food insecurity in the general Canadian population (which was 8.8% in 2017-18)Footnote 35. For example, the PHAC has reported that First Nations peoples have a high prevalence of type 2 diabetes with 19%, double that of the general population. Additionally, the Canadian Journal of Public Health has reported that "a majority of First Nations households are not able to achieve a healthy diet either from the traditional food systems within their territory due to external considerations now compounded by the climate crisis, or from the market foodsystem due to financial constraints that limit access to diverse and high-quality market foods."
4.2 Mandate
Finding 2: The federal government has a clear mandate to continue to address the greater risks and lower health outcomes associated with chronic diseases among First Nations individuals, families and communities.
The organization of Canada's health care system is largely determined by the Canadian Constitution. Roles and responsibilities are divided between the federal, provincial and territorial governments.
- Generally, provinces and territories have primary jurisdiction over the administration and delivery of health care services in their respective jurisdictions. Provinces and territories receive transfer payments from the federal government to provide universally accessible and publicly insured health services to all residents, including Indigenous Peoples.
- The federal government is responsible for enforcing the general standards provided in the Canada Health Act, respecting provincial health insurance plans. As well, Parliament has exclusive legislative authority for "Indians, and Lands reserved for the Indians" (Constitution Act, 1867, Section 91(24)).
- Indigenous communities also play a key role in the delivery of health services and programming.
It is important to note that the Canada Health Act, 1984, outlines the intent of Canadian health care policy in general and describes the conditions under which provincial and territorial governments qualify for the Canada Health Transfer. Further, section 3 of the Canada Health Act, 1984, states that Canadian health care policies are intended to ensure the physical and mental well-being of Canada's residents, and to facilitate reasonable access to health care, including Indigenous Peoples.
First Nations health jurisdiction is complex in nature. While the Constitution Act, 1867, and the Indian Act, 1876, identify jurisdictional responsibilities regarding Indigenous health care services, there is currently no legislation in place that provides clarity on the roles and responsibilities of different levels of governments in health care for Indigenous Peoples. It is important to note that under section 91 of the Constitution Act, 1867, the federal government has power to enact health legislation based on its "peace, order and good government" powers (e.g., laws pertaining to quarantine and national emergencies). In 2021, the Minister of Indigenous Services Canada was mandated to "co-develop distinctions-based Indigenous health legislation, backed with the investments needed to deliver high-quality health care for all Indigenous Peoples", which would improve access to high-quality, culturally relevant health services. Multiple streams of engagement are currently underway.
At present, the federal government provides health services to First Nations and Inuit as a matter of policy, as guided by the 1979 Indian Health Policy as well as the Indian Health Transfer Policy. The Indian Health Policy was adopted during a period of transition for FNIHB whereby FNIHB began to shift more towards helping communities gain more direct control over community-based health services rather than providing direct health care services. The Indian Health Policy also recognizes the interdependent nature of the Canadian Health system and identifies that two of the most significant federal roles are in public health activities on reserves and health promotionFootnote 36. Further, the Indian Health Policy describes the importance of reinforcing relationships between multiple levels of government and increasing the capacity of Indigenous communities to "play a positive and active role within the Canadian health care system"Footnote 37. As a result of the Policy, the federal government no longer directly provides services to First Nations people in the Northwest Territories, nor to the four Inuit regions: in Nunavut, the Inuvialuit Regional Settlement in the Northwest Territories, Nunavik in Quebec, and Nunatsiavut in Newfoundland and Labrador. Instead, federal government funding flows through transfer agreements with territorial governments and self-governments/land claim agreements.
During the Healthy Living evaluation timeframe, the Prime Minister implemented a recommendation from the Royal Commission on Aboriginal Peoples (1996) by dissolving Indigenous and Northern Affairs Canada, and replacing it with two new departments: Indigenous Services Canada (ISC) and Crown-Indigenous Relations and Northern Affairs Canada (CIRNAC). In 2017, Indigenous Services Canada assumed control of the First Nations and Inuit Health Branch, which was transferred from Health Canada. The Department of Indigenous Services Act (2019), provides for a legislative mandate for Indigenous Services Canada to work towards the transfer of departmental responsibilities and collaborate with Indigenous partners in all aspects of service delivery, including health.
In addition to the creation of the new ISC Department, the 2017 mandate letter to the Minister of Indigenous Services stated as one of the top priorities: "Lead work to create systemic change in how the federal government delivers health services to Indigenous Peoples in collaboration with the Minister of Health and the Minister of Crown-Indigenous Relations and Northern Affairs. Specifically, I would ask that you take an approach to service delivery that is patient-centred, focused on community wellness, links effectively to provincial and territorial health care systems, and that considers the connection between health care and the social determinants of health."Footnote 38
Budget 2018 also laid out the renewal of the Tobacco Strategy. The budget called for distinctions-based approaches and stated that, "the Government of Canada recognizes that a distinctions-based approach is needed to ensure that the unique rights, priorities and circumstances of First Nations, Inuit and the Métis Nation are acknowledged, affirmed and implemented."Footnote 39 In line with this, the FTCS was redesigned as CTS and included a distinctions-based, Indigenous-specific component. ISC key informant interview respondents (national and regional) noted that distinctions-based approaches have and will better equip the program to meet the needs of communities.Footnote 40 The 2018 budget also highlighted the significant gaps in health outcomes between Indigenous and non-Indigenous people and the higher diabetes prevalence rate faced by Indigenous peoples.Budget 2018 specifically states that "infant mortality rates of First Nations and Inuit children are up to three times higher, diabetes rates are up to four times higher (than Indigenous people)…this gap in health outcomes can be narrowed, and providing access to quality health care close to home is an essential part of that change."Footnote 41 The 2016 federal budget also "allocated $64.5M over five years, beginning in 2016-17, and $13.8M per year ongoing to expand Nutrition North Canada (NNC) to support all northern isolated communities. This included funding to also expand NNC Nutrition Education Initiatives, managed by FNIHB, to newly eligible First Nations communities."Footnote 42
5.0 Key Findings: Effectiveness
A consistent challenge faced by the evaluators was the lack of available and adequate outcome-specific data to properly assess the achievement of both the program's immediate and intermediate outcomes. Part of this challenge was due to the evaluation being conducted during the COVID-19 pandemic, which directly impacted the evaluation's team ability to conduct site visits and thus to collect end user/client data from HL Program recipients.
Collection of data on indicators for the HL Program is obtained from various sources including what is reported by communities or funding recipients depending on the type of funding agreement they are in. With the move towards more flexible funding arrangements, many of which (flex and block funding) allow First Nations communities to allocate health-related funds as they see fit given the realities and context within their communities, the potential could exist for even less reporting on health-related indicators by communities. Consequently, the main source of data relating to the health-related indicators under the HL Program are: the community-based reporting template (CBRT)Footnote 43, a data collection tool that is utilized by some communities depending on their funding agreement type; and the national Regional Health Survey undertaken by FNIGC approximately every four to five years. While this survey is significant, it is limited in providing specific Healthy Living outcomes. As such, the evaluation relied on triangulated data sources from the Regional Health Survey (RHS), administrative data as well as limited qualitative and quantitative evidence provided by key informant interviews and survey responses. Challenges around data and reporting are further expanded on in section 6.5 below.
5.1 Overall Achievement of Expected Immediate Outcomes
Immediate Outcome #1: First Nations and Inuit have capacity to support HL programming
An important component of enhancing the knowledge, skills and abilities of community workers is access to appropriate training and professional development opportunities. Both key informant interview respondents and survey respondents identified the importance of community staff accessing capacity building opportunities to better meet the needs of the local community.
The 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development, identified staff retention as a challenge in building community capacity, an issue that this evaluation has also noted continues to persist. Community-based capacity is increasing, however the high turnover of community-based staff is slowing that progress in some communities, whilst other communities have ongoing staff shortages to adequately deliver the sub-programs of the Healthy Living Program. Staff turnover has cost implications for communities with regards to training and capacity building as communities are often losing corporate memory, and there exists a constant need to train new staff.
Twenty-nine percent of survey respondents (n=92) indicated that training was sufficient, while 36% agreed that training is only somewhat sufficient to help them perform their jobs. At least 11% of survey respondents felt that training was not sufficient to support them in delivering Healthy Living sub-programs and 24% were not sure. Specific to the ADI program, 51% of survey respondents (n=80) agreed or strongly agreed that the ADI is succeeding in supporting efforts with regards to capacity building and training, 24% disagreed or strongly disagreed that the ADI is succeeding in supporting efforts with regards to capacity building and training and 25% were neutral.
A notable achievement of the ADI sub-program was the strong engagement of regional partners at their respective regional community of practice groups, which key informant interview respondents have referred to as "working groups." Key informant interview respondents across all regions expressed a high degree of satisfaction with this participatory working method and stated that the opportunities to build strategic partnerships with other colleagues at the national, regional and community levels have been beneficial.
As many key informant interview respondents noted, there is a strong desire for professional development opportunities, however the lack of appropriate funding has impacted the availability of professional development training opportunities for staff to further upgrade their skills and gain valuable knowledge across the sub-programs.
As a response to the COVID-19 pandemic, there was an increase in the participation of staff in remote communities accessing online training opportunities. This uptake was viewed by ISC key informant interview respondents as a positive, cost-effective means for staff to access training opportunities without having to physically travel to training sites. The community planning and program componentsFootnote 44 in the 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development, also concluded that Health Directors were making efforts to provide remote training opportunities for staff in remote communities in response to the inadequate training fundsFootnote 45.
Immediate Outcome #2: First Nations and Inuit have access to HL programming:
Access to the HL programming refers to the extent to which First Nations are able to offer the sub-programs in their communities, and for those that offer programs in their communities, the extent to which services were accessible for community members.
Funding arrangements are not program specific, rather they depend on the type of funding arrangement negotiated with the community or funding recipient. For example, in each community that the HL programming operates in, all the sub-programs (i.e., NNC, ADI, and CTS) can be found to be in the same funding arrangement.Footnote 46 However, the NNC Nutrition Education Initiative is only eligible in isolated northern communities based on the Crown Indigenous and Northern Affairs Canada (CIRNAC) determined eligibility criteria for the overall NNC program. Many key informant interview respondents, including ISC national and regional staff and community health staff, expressed concerns that the eligibility for Nutrition Education Initiatives funding was dependent on the First Nations community meeting eligibility criteria for the Nutrition North Canada subsidy administered by CIRNAC. If the community does not qualify for subsidies under CIRNAC, the community also loses eligibility for ISC funding for Nutrition Education Initiatives. Communities expressed the continued need for nutrition education after communities no longer qualify for the Nutrition North Canada subsidy, stating that nutrition education remains relevant.
Participation in the Healthy Living Program is open to all community members. At the same time, 36% of survey respondents (n=114) agreed or strongly agreed that the Healthy Living Program was reaching all community members (22% were neutral, 35% disagreed or strongly disagreed, 7% did not know). Impressively, from 2013-2014 to 2017-2018, the community-based reporting template (CBRT) has been reported to maintain strong client access levels. For example, the CBRT reported that 91.2% of First Nations communities provided HL Programs in 2017-2018 and 88.9% First Nations communities delivered physical activities in the same year (table 1).
| 2013-2014 CBRT | 2014-2015 CBRT | 2015-2016 CBRT | 2016-2017 CBRT | 2017-2018 CBRT | ||
|---|---|---|---|---|---|---|
| 1 | % of First Nations communities providing Healthy Living programs | 89.1% | 92.1% | 92.5% | 94.7% | 91.2% |
| 2 | % of First Nations communities that deliver physical activities | 86.2% | 87.6% | 88.1% | 91.6% | 88.9% |
| 3 | % of First Nations and Inuit communities that deliver healthy eating activities under the Aboriginal Diabetes Initiative | 87.8% | 88.2% | 90.3% | 92.6% | 88.5% |
Specifically regarding the ADI sub-program, key informant interview respondents highlighted that it is often difficult to engage with the working age population, given that programming typically occurs primarily during the standard working hours. Targeted programming that accommodated clients' schedules could improve participation of this group. It was also noted that in many cases, the same group of individuals consistently participates in the Program.
As of 2017-18, 56% of First Nations and Inuit communities had access to tobacco control activities,Footnote 47 1578 new smoke-free spaces, and 129 new smoking-related resolutions.
In many cases, and as a result of the COVID-19 pandemic, the HL Program has successfully pivoted to providing programming online by leveraging communications technology and social media (for example, cooking classes delivered via Facebook rather than in-person). This has also allowed for new clients who would not otherwise have access to targeted activities to attend online activities. While this has worked effectively in some areas, there continues to remain accessibility challenges for community members living in remote areas with limited internet access.
Immediate Outcome #3: First Nations and Inuit have knowledge of HL issues and practices:
Due to the COVID-19 pandemic, the evaluation team was unable to conduct direct site visits for this evaluation. However, relevant to this outcome, the RHS reports that 59.2% (2015-16) of First Nations adults with diabetes, attended a diabetes clinic. The pandemic also directly impacted the evaluators' ability to interview community partners and thus determine the achievement of this outcome. In addition, since many community partners were involved in the response to COVID-19, the evaluators were unable to fully engage them as planned. That being said, limited qualitative and quantitative evidence was provided in the key informant interview and survey responses presented throughout this evaluation, that suggests that First Nations and Inuit have knowledge of HL issues and practices.
5.2 Operational EffectivenessFootnote 48
Finding 3: Both key informant interview respondents and survey respondents reported that the Healthy Living Program is operating effectively, however the flexibility of the program to tailor to each community's needs makes overall effectiveness difficult to determine.
Key informant interview and survey respondents reported that the Healthy Living Program is operating effectively. In fact, 54% of survey respondents (n=91) stated that the quality of the Healthy Living Program and sub-programs has improved or significantly improved over the last five years. Some of the reasoning for this improvement included increased communication between community health representatives, continuity of the program and relationship building with clients over time. However, a majority of survey and key informant interview respondents identified a need for additional funding as a primary challenge. The funding constraints limited access to screening and management tools, training opportunities, and salary increases, which has led to difficulties in retaining ADI community-based program staff.
The previous evaluation noted that the HL Program was responsive to community health needs and priorities, allowing communities to tailor sub-programs to meet their needs. The survey respondents stated that many staff believe that the sub-programs are operating effectively. This includes 58% of the survey respondents that indicated they were involved in the ADI sub-program (n=79), 53% of survey respondents involved in CTS sub-program (n=30) and 52% of survey respondents involved in NNC Nutrition Education Initiatives sub-program (n=25) who either strongly agree or agree that the programs are operating effectively.
Given the flexibility in programming and services across regions, it has been challenging to determine the programs overall effectiveness and the extent to which expected outcomes have been met as described in the logic modelFootnote 49. An ISC key informant interview respondent articulated the challenge that evaluators faced by stating that "The extent to which [the program is] achieving these priorities is at the discretion of the community. Some First Nations are investing more in training or building knowledge capacity. Others are investing more in developing programming to deliver".
5.3 Community-Led Program Design
Finding 4: The Healthy Living program's community-led design adds strength to its ability to target the specific community in which it is operating.
One of the strengths of the Healthy Living Program lies in its design and delivery model being unique to each community, allowing for communities to define their evolving health needs and health priorities.Footnote 50 As a result of the diversity that exists in programming across communities and in targeted activities, it is difficult to determine if the program is effectively reaching all community members in all the regions where it operates. It is also unclear if a GBA Plus assessment was conducted at either the national or regional levels to support programming. Given that a GBA Plus analysis was not made available to evaluators, this evaluation will instead highlight the engagement and participation of various demographics in program activities, as well as opportunities or challenges that may exist. It is also unclear if all or most communities are engaging in strategies to reach harder to reach groups (i.e. working age population, 2SLGBTQIA+ peoples, or at-risk youth). A number of survey respondents reported that it is common to have the same clients attending different targeted program activities and/or accessing program services. Although there have been great improvements made by the program to reach all community members, there are still challenges in reaching those most in need of services.
When survey respondents (n=114) were asked about the degree to which the Healthy Living Program was reaching all community members, only 36% of survey respondents agreed or strongly agreed. Of note, 75% of survey respondents agreed or strongly agreed that there are service gaps that affect clients from accessing programming, services and activities, with 65% of survey respondents agreeing or strongly agreeing that there are efforts underway to close those gaps. There are various factors that contribute to gaps in services, including resource constraint challenges, hiring and retaining staff, and remoteness of some communities. For example, key informant interview respondents and survey respondents identified the service gap of the need to incorporate culturally relevant approaches in programming. This service gap was also mentioned in the previous 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development. Many community leaders and staff have indicated that there is "a growing recognition in their communityof the health and well-being benefits of their traditional activities and diets, and indicated thatsteps were being taken to incorporate language programming, traditional teachings, traditional foods, and other traditional aspects into programming"Footnote 51. For the ADI and the NNC Nutrition Education Initiatives specifically, key informant interview respondents highlighted the need for culturally relevant practices and resources to be more directly integrated into programming, as well as to promote integrated healthcare models whereby various healthcare providers (i.e., registered dietitians and nurses) collaborate to a greater extent than at present.
In key informant interviews, respondents have expressed that they actively employ various strategies to reach as many individuals as possible in their communities. For example, some communities have collaborated with other event organizers in their communities to promote diabetes awareness and education to a mass audience, while other communities have in the past provided incentives to clients for their attendance (i.e., prizes). A regional ISC employee in a key informant interview highlighted the potential reach of the program, stating that the "Healthy Living programs have the potential to reach everyone in the community – from the well population to the very sick; from babies to Elders – across the lifespan". They noted that some communities have gone to great lengths to include harder-to-reach populations in their programming by "providing child-care, transport and prizes for participating like food vouchers or food".
Key informant interview respondents have also acknowledged that it is easier to reach seniors, individuals that are unemployed, and homemakers in accessing and participating in programs and services. To better accommodate participant needs and increase the attendance of harder-to-reach groups, it was suggested by a key informant interview respondent that educational pamphlets for Elders can be translated in local languages, peer-led learning opportunities for youth should be increased, and access to exercise therapists for individuals with varying physical limitations should be provided.
It is difficult for many communities delivering Healthy Living programming to reach the 30 to 50 year-old age group to access and participate in program services, since they are either likely engaged in work or child-rearing activities during the programs' standard operating hours. Since many program activities take place during the day, it is less likely for individuals to take time off work to attend. As highlighted by a key informant interview respondent: "The challenge is timing. Not everyone can reach sessions at 2 p.m.. How do we effectively reach people when people are working? It makes for a long day to offer programming at 7 p.m., but I see the value in prevention".
COVID-19 brought several challenges to the delivery of the Healthy Living Program, including pivoting activities to online platforms. While this has caused access and participation challenges for some community members, it has also allowed for new clients who otherwise would not have attended targeted activities to participate in online activities. One key informant interview respondent underscored the COVID-19 related challenges, stating: "I think there have been great improvements to reach out to all community members, but it is still not often reaching those most in need of services. I also feel there has been improvement in collaboration and this will ultimately reach more members. I do, interestingly, see a different uptake since COVID in that different members are joining in local programming via Zoom verses the "usual" group that join events in person".
5.4 Complementarity among Healthy Living Sub-Programs
Finding 5: Healthy Living sub-programs, particularly the Aboriginal Diabetes Initiative and the Nutrition North Canada Nutrition Education Initiatives, complement each other well.
ISC key informant interview respondents, both in the national and regional offices spoke to the complementarity of the Healthy Living sub-programs. The sub-programs inherently focus on lifestyle factors that increase the risk for chronic disease, be it nutrition, smoking, or exercise. One ISC regional office key informant interview respondent stated that "prevention is prevention, every single health program should overlap." Many survey respondents also noted that collaboration was key to delivering holistic care.
The Healthy Living sub-programs, particularly the ADI and the NNC Nutrition Education Initiatives, complement each other well. 61% percent of survey respondents (n=114) agreed or strongly agreed that the program areas within Healthy Living are collaborating, with some survey respondents noting that this is often the case, since staff members were often responsible for multiple Healthy Living sub-programs. The majority of national and regional ISC key informant interview respondents, who worked on ADI and NNC Nutrition Education Initiatives spoke to their complementarity. For example, a national office key informant interview respondent expressed that: "With ADI and NNC, they are the perfect complement. In Manitoba region, and other regions as well, NNC and ADI were amalgamated. There is one worker for both or two workers that worked closely together. They amalgamate cooking classes, or land activities, or going into schools. There are also joint events and trainings for the workers." This sentiment was also corroborated by the previous Healthy Living Evaluation.
Survey respondents have also underscored the complementarity and strong linkages between ADI and NNC Nutrition Education Initiatives in the survey, stating: "ADI and NNC work well together, and it's great that the funding can overlap in many ways to support similar projects" and "The ADI and NNC try to work together at times doing workshops on healthy cooking and harvesting and preparation of tradition foods off the land". ISC regional key informant interview respondents noted the importance of addressing food security to tackle diabetes prevention and management, with one regional key informant interview respondent stating, "there is a clear aspect of ADI that is food security related". Survey respondents also highlighted the complementarity that exists between ADI and CTS: "Often times, Diabetes and Tobacco Cessation programs go hand in hand together to meet the needs of the client. Often times with prevention, we want to support and educate a diabetic smoker to help quit their use of commercial tobacco so that they don't get secondary conditions such as hypertension or cancer, and help a smoker reduce their use or quit so that they don't become a type 2 diabetic and to adapt healthier choices such as eating better, exercising, self-care, stress reduction etc".
Outside of the program itself, there are many linkages across levels of government and with partner organizations. Within the department, Healthy Living is complemented by the Non-Insured Health Benefits program which offers several diabetes treatment supports including medications, blood glucose test strips, medical supplies, and equipment (medical devices, medical transportation, etc.). Across government, the Healthy Living Program works both with Health Canada on CTS and CIRNAC for NNC. The FNIHB National Office works and collaborates with both the Assembly of First Nations and Inuit Tapiriit Kanatami to inform the Healthy Living program.
6.0 Key Findings: Efficiency
6.1 2014 Healthy Living Evaluation
Finding 6: The First Nations and Inuit Health Branch (FNIHB) has reported that the recommendations from the previous 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development have been addressed and implemented.
The 2014 Cluster Evaluation covered both the Healthy Child Development and the Healthy Living ProgramFootnote 52, and as such the recommendations within referred to both program areas. Responsible for the implementation of the Management Response Action Plan (MRAP), FNIHB has reported that the recommendations have been addressed and implemented.
The evaluation identified three recommendations which were approved by Health Canada's Deputy Minister in February 2015 (FNIHB was previously part of Health Canada). Below are the status of each of those recommendations last reported in January 2018:Footnote 53
| Recommendation | Actions |
|---|---|
| 1. Improve collaboration efforts with stakeholders, partners and other service providers that ensure sustained partnerships and program integration. | a. The Chronic Disease Prevention and Management (CDPM) Framework was reviewed with the AFN, approved and completed in September 2017; and, b. The Oral Health Strategic Action Plan (OHSAP) was approved in July 2015. |
| 2. Sustain efforts to support improved program and service access and quality. | a. A costing model for the cluster HL/HCD programs including an examination of provincial and territorial costing models and a discussion of major cost drivers (e.g., population growth) and their implications for service delivery was completed in March 2016; and, b. Standards for Healthy Living, (includes Chronic Disease Prevention, Oral Health) and Healthy Child Development; and, c. Work was started but cancelled. Developing core standards at the Branch-level is to resume once engagement with partners is clear and options are developed for moving forward. |
| 3. Streamline and implement improved performance measurement. | a. A Healthy Living / Healthy Child Fact Sheet was completed and published in April 2015; and, b. The data collection strategy for Healthy Living was completed that included an updated Logic Model approved in March 2016 and updated [performance] indicators were approved in March 2016 and updated in July 2017. |
6.2 Program Management Structures and Division of Responsibilities
Finding 7: The current program management structures and division of responsibilities between national, regional, and community levels allows for the Healthy Living Program to achieve desired results.
The Healthy Living program management structure is organized as such: FNIHB staff at the National Office within the National Capital Region lead strategic, program policy development and planning, working closely with FNIHB regional offices and First Nations partners at the national level (i.e., National Indigenous Organizations). FNIHB Regional Offices play a lead role in supporting communities with program delivery as requested by working with First Nations partners at the regional and local levels. They are also responsible for the management of funding arrangements, program performance monitoring, and information roll-ups. Finally, the FNIHB Northern Region works directly with the territorial governments and self-governing First Nations in Yukon and selected communities within Northwest Territories to negotiate funding arrangements for health programming, and ensures that First Nations partners are engaged in decision-making. There is a wide variation in the Healthy Living management structures and operations at the regional levels.
FNIHB's Senior Management Committee is the main decision-making forum for the Branch on issues related to policy development and priority setting. This committee consists of representation from senior management at both the national and regional offices and representatives from the Assembly of First Nations. In addition to this committee, The HL Program collaborates with national and regional First Nations organizations and other stakeholders to ensure that there is representation in the program decision-making.
The communities or Tribal Councils are funded through funding arrangements to support the implementation and delivery of the Healthy Living Program. Community or Tribal Council support includes building their internal capacity through the hiring and managing of community program staff, providing office space and program resources to staff, and working with regional offices to provide training for local staff.
Key informant interview respondents at both ISC national and regional levels have highlighted that the current program management structures and division of responsibilities between national, regional, and community levels allows for the Healthy Living Program to achieve desired results. Specifically, the variation in management structures at regional levels has allowed for some regional offices to develop responsive and flexible structures that meet the needs of the communities they support. In addition to the management structures creating a conducive environment for the HL Program to operate and achieve desired results, the evaluation also inquired about best practices that have improved the overall efficiency of the program as it relates to the program governance and management.
Many ISC national and regional key informant interview respondents and survey respondents have shared best practices that have improved the efficiency of the HL Program including (but not limited to):
- Territorial governments have established community wellness and health divisions which are entirely First Nations led. They have their own body of knowledge and expertise in-house and are well known in their communities;
- Communities taking on the lead role of implementing sub-programs, and receiving capacity building and other support from regional offices as needed; and;
- Maintaining strong relationships between regional offices and community staff.
Additionally, Indigenous partner organizations have also highlighted that having access to additional mentorship support from their respective regional offices may potentially improve the overall efficiency of the HL Program
6.3 Community Health Planning Process
Finding 8: The community health planning process is viewed by Indigenous partner organizations and community health representatives as an effective process which allows communities to drive their own needs and priorities.
The community health planning processes aim to meet the unique health needs of First Nations and Inuit communities. This process are not unique to the Healthy Living Program and are in fact processes that FNIHB implement across programs. Several key informant interview respondents highlighted that they have robust community health planning processesFootnote 54 in place and are well integrated in many community-level activities, focusing on encouraging the collaboration of multi-disciplinary teams, and allowing communities to drive their own needs and priorities. Regional offices have noted in key informant interviews that they often receive diverse community health plans (CHP), since the plans often reflect the communities' capacity and resources. In the survey, some respondents spoke to the importance of the CHP and addressing community needs, with one respondent stating that "each of the Health Programs are part of our work plans that we plan based on what is available funding-wise...they are designed to complement each other as a whole in addressing the community's needs based on what we can afford to do". Encouraging communities to drive their own needs is an important aspect of the CHP process, a survey respondent expressed that: "our community health plan has identified chronic disease as a priority area and goals and objectives have been set to meet these".
Key informant interview respondents have shared best practices that have been employed to increase the efficacy of community health plans as it relates to the HL program. These include (but are not limited to):
- Utilizing dietitians and diabetes nurses to support stronger linkages between need and priorities of communities and ensuring the voices of communities are more present throughout activities;
- Ensuring the inclusion of the social determinants of health; and
- Including the community in the development of the community health plans and ensuring consistent community representation for an extended period of time, as it helps to retain corporate knowledge.
78% of survey respondents (n=78) agreed that the Healthy Living Program was well incorporated into the community health planning process in their respective communities. There was a mixed response from survey respondents on whether they were aware of the incorporation of HL sub-programs in community health plans. Some respondents highlighted they were intimately involved in the process and worked towards identifying community priorities vis a vis HL sub-programs, while other respondents were either not aware or not involved in the plan development (i.e., employed by a Tribal Council).
6.4 Financial Resources
Finding 9: Access to adequate financial resources has impacted the program's ability to recruit and retain staff and provide sufficient capacity development opportunities for staff.
Two barriers facing many of the communities delivering the Healthy Living sub-programs are access to adequate financial resources and the provision of additional training opportunities. Funding constraints have a negative impact on both the recruitment and retention of community-level talent, and access to financial resources to support professional development training opportunities for staff are limited. Funding has been stagnant (i.e., not keeping up with inflationary pressures, and the increased needs of the program) for many years, leading to unmet needs of the program and little to no increase in salaries at the community levels, contributing to high turnover rates and vacant positions. The lack of financial and human resources faced by communities, has also impacted the program's potential loss of corporate/ institutional knowledge when, for example, when staff depart.Footnote 55
A significant number of key informant interview respondents highlighted the impact of inadequate financial resources on continuing programs, with one key informant interview respondent stating that "from a community point of view, the funds haven't increased over time. There's not enough funding for program delivery. The other challenge is the constant turnover of staff. Often times, the salary is not competitive and staff turnover is a problem in the delivery of the program".Similarly, a survey respondent acknowledged the human resource impact on the program, stating that "staff turnover makes it difficult to continue programming over a long period". Other respondents have suggested an increase in funding would allow for communities to have access to in-house professionals, with one key informant interview respondent stating that it would be beneficial to "not have people needing to travel out to see health professionals if they could see their own dietitians in the community. There isn't funding for it currently and it makes it a challenge for people to achieve their goals and follow the best practices when you don't have those resources available". Sharing a similar response, one survey respondent shared a similar perspective on the need for in-house professionals:"working out of a tribal council and needing to travel to communities to provide professional support. Having professional staff working out of each clinic would be much more successful". Additionally, an ISC regional key informant interview respondent expressed that "major staff turnover means that a constant need for [re-]education, [since] the new staff don't have an adequate understanding of the program or base knowledge to be able to transfer it out. The fact that they wear many hats especially in smaller communities, so they're pulled between many programs".
The survey (n=92) indicated that 29% of the respondents felt that training was sufficient, while 36% agreed that training is only somewhat sufficient to help them do their jobs. At least 11% of staff felt that training was not sufficient to support them in delivering HL programs and 24% did not know. For example, survey respondents also suggested the need for a wide variety of training that is relevant to the type of work staff are engaged in. Survey respondents also identified a need for traditional-based training, physical activity training, trauma-informed approaches, nutrition-based training including cooking skills, withdrawal and support (addictions), gardening, and mental health training.
An increase in program funding would also allow for communities to focus on implementing a holistic and comprehensive approach to addressing chronic disease, rather than a focusing on individual risk factors. Moreover, an overall consensus exists in health care literature that chronic disease management and primary care that promotes wellness, screening, and other preventive care results in improved outcomes and lower overall health care costs.Footnote 56 This could be an area for further analysis that the evaluation was not able to conduct.
Key informant interview respondents also expressed concerns about inadequacy of funding for Nutrition Education Initiatives given the high price of food in the North, and the travel expenses for workers that service multiple communities. Ultimately, these high food prices make cooking classes, and other engagement sessions expensive, and increase program costs. Additional funding is also needed to facilitate training for staff.
Prior to 2018-19, the CTS operated through proposal-based funding which presented problems in staff retention and medium and long-term program planning. With the transition from the FTCS to CTS in 2018-19, the program adopted a distinctions-based approach. This included a switch from proposal-based funding to on-going funding. It is presumed that consistent funding will reduce staff turnover as salaries will be able to be anticipated for the upcoming years. A national office key informant interview respondent highlighted the importance of stable funding for CTS: "It takes persistence, involvement of leadership and partnerships. It's important to have consistent funding, so projects are going from year to year knowing what their future would look like".
Despite a move away from proposal-based funding, respondents from the regional offices highlighted that the CTS remains insufficiently funded, especially in regards to staffing requirements. Regional staff noted that frontline health care workers are busy with other priorities, and that funding is required to support health care workers assigned specifically to the tobacco program.
6.5 Performance Measurement Systems
Finding 10: Performance measurement systems exist to collect data for the Healthy Living program. However, the administrative data tools are not performing optimally and there are some important gaps in supporting Indigenous-led data management at the community, regional, and national levels.
"We need to be able to compare efficiencies over a 5 year period… We need a good tool to collect health data, and this tool needs to take a community portrait. So they know about the individual level but we don't have a community portrait. I can't say if it's working well or not, because we don't have the data at either the national/regional level. I'm wondering: do we have enough health data to say it's working or not? I don't think so".
The program relies on a number of data sources to track and measure performance. Some of this data is collected directly through the program, while other data is made available through external sources, such as the Regional Health Survey. Below are the various data points available to the program and the challenges associated with them.
- The community-based reporting template (CBRT)Footnote 57 is a reporting requirement associated with certain contribution agreements between First Nation communities and FNIHB. The CBRT encompasses several program areas, such as healthy child development, communicable disease control and management, home and community care, mental wellness, and healthy living. The CBRT was first developed in 2008-2009, and since then it has undergone several iterations. For the 2018-2019 reporting period, 314 communities in Canada completed the HL Program's CBRT reporting requirement. This includes communities in Alberta, Saskatchewan, Manitoba, Ontario, Quebec, and Atlantic regions. As a result of the diverse funding agreements across sub-programs, reporting requirements vary from community to community, and not all communities are required to use the CBRT as a reporting tool.Footnote 58 Throughout key informant interviews, community workers expressed the importance of collecting and utilizing the CBRT to not only fulfil their funding requirements but also to provide a snapshot of the community's health and well-being. Conversely, there is also an expressed need from partner organizations to further improve the CBRT, as it does not collect information at a sufficiently detailed level for communities to effectively track performance and achievement of results. For example, based on CBRT reporting in 2015-16, 93% (n=317) of communities held healthy eating awareness/education sessions, 91.5% (n=270) reported offering the same session in 2017-18, and in 2018-19 it was reported that 91% (n=314) of the communities that reported to deliver HL program, held healthy eating awareness/education sessions. CBRT data collected from communities may not be sufficiently detailed enough to support communities in systematically collecting and utilizing quantitative data to better tailor programming to their own health needs and priorities.
As well, the CBRT data collected is not inclusive and it does not have comprehensive data for all performance indicators across all communities. Key informant interview respondents have also called for increased performance measurement systems to support client information management, with one respondent stating: "having a database that supports the tracking of client information for our small community…many of our clients have a physician so our involvement is limited outside of promotion and primary prevention." Challenges around data limitations were also corroborated by the previous 2014 Evaluation of FNIHB's Healthy Living and Healthy Child Development Community Planning Program Components,Footnote 59 which concluded that: "performance measurement has improved, particularly for measuring intermediate and long-term outcomes. However, focus on performance indicators and data collection that support immediate outcomes, specifically the reach and access of HL and HCD programs could be enhanced to better support program monitoring, for planning and reporting".
- A significant secondary data point for the HL Program is obtained through the First Nations Regional Health Survey (RHS), a large cross-sectional survey administered by the First Nations Information Governance Centre (FNIGC)Footnote 60, a non-profit First Nations organization. The RHS is the only national First Nations health survey in Canada and produces important innovations in computer-assisted interviewing, culturally appropriate questionnaire content, sampling, and field methods. The survey was administered in 2002-03, 2008-10 and in 2015-16 among First Nations populations living on-reserve and in northern communities. The RHS is also the first national survey that explicitly implements the First Nations principles of OCAPFootnote 61. The RHS collects information from the majority of First Nations on-reserve communities on a select range of topics and by age cohorts - children (0-11 years), youth (12-17 years) and adult (18 years and older). The 2019 National Report of the First Nations RHS employs 64 indicators that have been tracked and gradually refined and expanded for over 20 yearsFootnote 62. Of particular note for the HL programming, the survey collects high level information on diabetes, physical activity, food security, nutrition, health and chronic conditions. While the RHS is a robust mechanism for monitoring high level health outcomes every five years, it is typically available only at the national level and does not provide sufficient details about what is working and what is not at the sub-program and regional and community levels and specific Healthy Living outcome level data.
- Additionally, the NNC Nutrition Education Initiatives utilize an annual reporting template completed by eligible funding recipients. Communities collect and report data related to NNC Nutrition Education Initiatives programming, specifically on nutrition knowledge and awareness among clients, retail-based nutrition knowledge and awareness, food skills development, traditional food knowledge and skills, and healthy food access. For example, during the 2018-19 reporting period, 4,700Footnote 63 activities were delivered by First Nations and Inuit funding recipients and in total there were 49,000Footnote 64 participants that attended nutrition activities. The limitation of this data collection tool was not determined by the evaluators.
6.6 Funding Arrangements
Finding 11: The current funding modelsFootnote 65 for the Healthy Living sub-programs are appropriate as they meet the needs and priorities of communities.
"Funding arrangements create short term projects delivered in separate program activities. One aspect of health is dealt separately from other aspects of health, such as physical, and mental, which translate into program delivery such as nutrition and mental health, and traditional practices are relatively absent from programming".
The ADI program funding arrangement varies across regions, with most communities having flexible or block funding contribution approaches. Some key informant interview respondents have expressed that block funding is preferred as it allows for greater flexibility and reduces reporting burdens. There are also a few communities that are in set contribution agreements (less flexible in how funding is utilized). A key informant interview respondent explained that some communities prefer set contribution agreements over funding agreements that allow for more financial flexibility, because set contribution agreements ensure that funds are specifically earmarked for the ADI. Thus, set contribution agreements allow for some communities to ensure funds are utilized for a specific program as opposed to utilizing funds to meet potentially changing community priorities and needs. Key informant interview respondents supporting ADI and CTS have reported that while the funding arrangements are appropriate, the current funding amounts are inadequate and do not match their needs, emphasizing in key informant interviews the challenges this creates in retaining professional staff and the overall impact in the delivery of services.
Across NNC eligible communities, the funding model varies. For example, the recent Horizontal Evaluation of Nutrition North Canada states that in some cases, the funding is directly provided to communities while in other cases, funding arrangements are provided to other governments (i.e., tribal councils, territorial governments, etc.) to support various eligible communities. With the NNC Nutrition Education Initiatives, ISC and the Public Health Agency of Canada (PHAC) provide funding and support to eligible communities for the delivery of retail and community-based nutrition education activities. Communities then decide which NNC nutrition education activities they wish to implement based on their own needs and priorities.
With the transition from the FTCS to CTS in 2018-19, the program adopted a distinctions-based approach (this is discussed in further detail in Finding 9). Despite a move away from proposal-based funding, key informant interview respondents highlighted that the program remains insufficiently funded, especially in regards to staffing requirements. They note that since front line health care workers are busy with other priorities, additional funding is required to support health care workers assigned specifically to the tobacco program.
7.0 Key Findings: Sub-programs
7.1 Aboriginal Diabetes Initiative (ADI)
7.1.1 Operating Effectively
Finding 12: The ADI has made progress to foster a high level of satisfaction among community partners
Since the 2014 Evaluation of the First Nations and Inuit Healthy Living and Healthy Child Development, this evaluation has found that overall, considerable progress has been made to suggest that the ADI has delivered meaningful results in community-based health promotion and primary prevention.
Throughout this evaluation, evidence was collected to assess the program's operational effectiveness related to the prevention and management of type 2 diabetes, which is presented below. In addition, this particular finding also focusses on how the ADI is supporting efforts with regards to the four components of the programFootnote 66.
The online survey of ADI staff (n=79), demonstrates that 58% of survey respondents either agreed or strongly agreed that the ADI is operating effectivelyFootnote 67 in the prevention and management of type 2 diabetes (23% were neutral and 18% disagreed or strongly disagreed, 1% did not know).
When survey respondents were asked to rate the extent to which the ADI is succeeding in supporting efforts of the four program components, the majority of the survey respondents agreed or strongly agreed that efforts have been made. Of the 79 respondents that completed the online survey:
- 76% agreed or strongly agreed that the ADI was succeeding in community based health promotion and primary prevention;
- 58% agreed or strongly agreed that the ADI was succeeding in screening and management activities;
- 51% agreed or strongly agreed that the ADI was succeeding in capacity building and training; and
- 62% agreed or strongly agreed that the ADI was succeeding in knowledge mobilization and sharing.
Throughout the evaluation, evidence was also collected to assess the achievement of the programs four components, which are presented below.
Community-based health promotion and primary prevention:
"It [type 2 diabetes] is a manageable disease and there needs to be education and awareness around this. [We] need to look at the needs of the community and the reality that there probably isn't an Indigenous person in Canada that hasn't been touched by diabetes. There are varying levels of trauma that go along with that".
The community-based health promotion and primary prevention component focusses on a range of culturally appropriate activities to promote health and prevent diabetes, create supportive environments, and increase healthy behaviours. Key informant interview respondents confirmed that there is a strong focus on delivering promotion and prevention, because of the foundational role it plays in the overall design and delivery of the ADI, and that many communities are strong in delivering this component.
Flexibility in program design also allows communities to implement activities that match the local needs, priorities, and realities. One key informant interview respondent reflected on the importance of flexible program design, stating: "I think it is important to further support and encourage communities to determine their own priorities and follow that path with appropriate supports. Communities are the best people to tell you about their community, their needs, and experiences".
While there exists diversity in the activities that are implemented across regions, there are also notable similarities as well. For example, promotion and prevention activities implemented across regions largely focused on delivering services related to the following key areas: diabetes awareness, healthy eating, and physical activities. Furthermore, in many of the communities implementing diabetes awareness efforts focused on: building and maintaining relationships with community members, developing and delivering culturally appropriate education and activities to community members, developing education materials taking into account various individual literacy levels, and including traditional practices and approaches in activities.
Strong efforts were made by key informant interview respondents to promote the integration of traditional physical activities and reduce sedentary time, which can prevent and/or reduce chronic diseases such as type 2 diabetes. During the 2018-2019 reporting year, of the 314 communities that reported delivering Healthy Living programmingFootnote 68 :
- 93% reported offering physical activity awareness activities;
- 75% reported offering sports and recreation activities;
- 76% reported offering traditional physical activities; and
- 61% reported offering walking clubs;
The online survey also highlighted that of the 80 survey respondents:
- 76% of agreed or strongly agreed that the ADI is succeeding in supporting efforts with regards to community-based health promotion and primary prevention;
- 15% disagreed or strongly disagreed that the ADI is succeeding in supporting efforts with regards to community-based health promotion and primary prevention;
- 9% of the respondents were neutral.
Screening and management:
"There are huge barriers to screening in most communities. (Community partner) doesn't have the money to afford laboratory services in their community".
Screening and management includes complications-screening initiatives, diabetes education, and complications prevention such as foot care programming and diabetes self-management. Screening and management efforts and activities vary from community to community depending on their needs and priorities.
There is varying capacity in the level of screening and management effectiveness across regions. Of the 302 communities that responded to the diagnostic screening questionFootnote 69 asked in the CBRT, 54% reported that they delivered diagnostic screening during the 2018-19 reporting period. During that same reporting period, of the 299 communities that responded to the non-diagnostic screening questionFootnote 70, 83% reported to have delivered non-diagnostic screening. In interviews with key informants, respondents have noted that certain communities lack proper screening tools, such as access to specimen collection and lab licensure, as well as access to provincial health dataFootnote 71. Specifically, some key informant interview respondents have expressed that they lack an A1C screening station that will allow them to conduct a blood test to assist in the diagnosing of type 2 diabetes. A minority of these key informant interview respondents have also noted that the lack of available screening stations has meant that available physicians are spending more time seeing clients that are in need of a blood test. While some communities lack the proper screening tools, other key informant interview respondents note that cost can play a role in the frequency of screening activities in communities. For example, one health clinic respondent stated: "we are screening and have been able to do A1C tests in [the] community…we have a scale on the computer that shows effects of their lifestyle and visually show them what the consequences could be. I think this has been really rewarding because people are more likely to get on board. Screening has been limited because of costs – tests are expensive so we can only do so many".
The online survey (n=80) highlighted that:
- 58% of survey respondents agreed or strongly agreed that the ADI is succeeding in supporting efforts with regards to screening and management;
- 16% disagreed or strongly disagreed that the ADI is succeeding in supporting efforts with regards to screening and management;
- 26% of the respondents were neutral.
In addition to the online survey, the CBRT reports that during the 2018-2019 reporting year, of the 314 communities that have reported delivering an HL Program, 94% provided diabetes information sessions/workshops and 78% reported to have developed resource material. As well, of the 307 communities that responded to the diabetes clinics and training question, 93% have provided diabetes education clinics and training to their community members and 78% provided diabetes foot care clinics.
Capacity building and training:
Capacity-building opportunities are widely viewed as providing community health representatives with the knowledge and skills to support program delivery. Specifically, the ADI continuing education opportunities support health professionals and para-professionals working with communities in diabetes awareness, health promotion, and foot care. In addition, regional multi-disciplinary teams provided subject-matter expertise to communities on diabetes, physical activity, and nutrition.
Current capacity building and training efforts are on-going for staff supporting the ADI. Most key informant interview respondents noted that staff are keen in building upon their training repertoire. Specifically, staff noted interest in building their capacity to support clients and families with managing and improving their mental health and in having access to training that goes beyond the biomedical component of type 2 diabetes.
While staff working in remote communities often face the additional challenge of accessing and attending trainings in-person, some trainings are now being offered online as a response to the COVID-19 pandemic, thereby allowing staff working in remote communities to participate in online trainings. There has been concern expressed by some key informant interview respondents regarding the availability of funding for ADI training, particularly the funding availability for ADI staff to attend trainings (discussed further in section 6.4), while for others, communities had earmarked ADI training dollars this is not a concern for them as they earmarked some funding dollars for staff to attend training(s)/conference(s).
The online survey highlighted that of the 80 survey staff respondents :
- 51% of survey respondents agreed or strongly agreed that the ADI is succeeding in supporting efforts with regards to capacity building and training;
- 24% disagreed or strongly disagreed that the ADI is succeeding in supporting efforts with regards to capacity building and training;
- 25% of the respondents were neutral.
Knowledge mobilization/ sharing:
Knowledge mobilization/sharing refers to the sharing of information to support communities in their programming and services, including but not limited to: sharing promising and best practices and latest trends in research, as well as clinical practice guidelines.
"There are some little pieces of info and ideas that come around - but overall we find there is not a lot of training on ideas for supporting prevention, screening and management in the community. In some ways, this is good so that we are more flexible and focus on what our community needs, but in other ways, it would be nice to have more information coming around. More knowledge sharing between communities would be excellent, maybe some teachings from elders, etc."
The engagement of regional partners at their respective regional community of practice groups, also known as "working groups", has been successful as noted by many key informant interview and survey respondents. In interviews across all regions, key informants have expressed a high degree of satisfaction with their many respective working groups, recognized the importance of tailoring activities to community needs and priorities, and expressed that the opportunities to build strategic partnerships with other colleagues at the regional and community levels have been beneficial for their work.
The National Indigenous Diabetes Association (NIDA), a leader in knowledge and mobilization and sharing, offers many resources on their website, as well as organizes conferences and networking opportunities for staff supporting the ADI. Prior to COVID-19, community partners in many regions reported meeting in person with their colleagues in their respective region, often for knowledge sharing opportunities. However, as a result of COVID-19 travel restrictions, many have pivoted to hosting meetings online. Below are some comments expressed by key informant interview respondents from various regions regarding the effectiveness of knowledge management in their respective regions:
- "I have to say the ADI regional program is awesome. We get together as a group and address barriers to the province. And as a result we have a gestational diabetes manual and a paediatric orientation manual that incorporate culture and are very comprehensive".
- "I participate in the provincial diabetes educator group, this is great to keep me abreast, and to be able to talk to the people that are delivering the one-on-one care and discuss new developments in diabetes (medication, shorter needles etc.). They also have case study discussions, and this certainly enhances my knowledge".
- "Every year, they have a conference/training, so they'll do workshops for a day or two and then presentations. That's when all diabetes coordinators come together and share best practices".
- "The ADI working group is such a key success in our region, the coordinators themselves love to come together. They're always working on some project to move forward these challenges in the community".
The online survey highlighted that of the 79 respondents that completed the online survey:
- 62% of survey respondents agreed or strongly agreed that the ADI is succeeding in supporting efforts with regards to knowledge mobilization/sharing (between programs and communities);
- 15% of survey respondents disagreed or strongly disagreed that the ADI is succeeding in supporting efforts with regards to knowledge mobilization/sharing (between programs and communities);
- 21% of the respondents were neutral;
- 2% did not know.
7.1.2 ADI Key Challenges
Finding 13: There are a few key challenges that may hinder the ADI from potentially meeting needs and priorities, including the impact of funding constraints, staffing challenges, technological disadvantages faced by some clients, and the impact of food insecurity.
A number of key challenges were identified in the document review, in interviews with key informants, and in survey responses. Below is a list of the key challenges that communities face as they work to deliver the ADI.
"What does become a little bit challenging is not necessarily the disparities but the uniqueness of each of the regions and their needs".
- Funding concerns: A lack of adequate funding (this is further discussed in section 6.4) is a concern for many key informant interview respondents. Specifically, respondents expressed that stagnant program funding impacts human resource capacity concerns, capacity building opportunities available to staff supporting ADI efforts, and hinders the program's ability to develop further. Recruitment and retention of ADI staff is a challenge faced by many of the survey respondents, with one individual stating: "[there is] not enough funding given to hire an actual Certified Diabetes Educator and a dietitian, and you really do need both professions working side by side to ensure the clients full needs are being met".
There exists strong interest for professional development opportunities among key informant interview and survey respondents, this was also a finding that was highlighted in the previous 2014 Healthy Living Evaluation. For example, a key informant interview respondent highlighted the funding challenge vis-à-vis capacity building, stating: "our base funding for all those positions really just covers our salaries and admin fees. We rely on additional funding to do other capacity building opportunities". Furthermore, both national and regional ISC staff key informant interview respondents also corroborate this finding, expressing that their communities lack adequate funding to be able to support health staff in further upgrading their skills and knowledge.
To address this funding challenge, some key informant interview respondents have focused on taking an innovative approach with capacity building and seeking additional resources that may be available to them. For example, the bi-annual diabetes conference hosted by the National Indigenous Diabetes Association (NIDA), has had to seek additional funding from external sponsors to meet conference needs. Another key informant innovatively organized trainings for ADI staff, offering an annual telehealth education session, in which a medical officer provides various education sessions to staffFootnote 72. Many key informant interview respondents have expressed a strong desire for staff to have access to supplemental training. With one such respondent stating that "training is an expressed need. As with anything funding is always a challenge, such as the ability to pay for training and actually get things done". There is interest for the following training opportunities in the following topics (not a comprehensive list): diabetes, physical education, and mental health training.
"It may be hard to recruit those people to some of those communities that are fairly remote. I think it can also be really exhaustive for staff working in those programming areas, burnout is really common, and with that comes a lack of motivation and I think that has a lot to do with it".
- The remoteness of some First Nations communities has impacted program delivery in some communities, and this is further corroborated by key informant interview respondentsFootnote 73. While nursing stations and health centres service remote communities, the program continues to face challenges, including the recruitment and retention of health professionals. A key informant interview respondent highlighted the impact of reaching participants in remote communities and the associated travel cost, stating "higher cost in travel, living in the north and the projects in the north don't get any additional funding for those challenges…remoteness factor does play a factor in reaching all population groups especially those that are farther away". While it is undeniable that remote communities face increased program costs vis-à-vis non-remote communities, key informant interview respondents have suggested that this is not necessarily a limitation of the program, but rather recognition of the uniqueness in needs and environmental considerations to make for each region and community. An ISC key informant interview respondent further highlighted the uniqueness challenges faced by remote communities, citing structure and capacity as challenges.
- Regional and Provincial Health Authorities: The ability for communities to access their health data and/or electronic charting from both provincial and/or regional health authorities is an ongoing challenge faced by clients and many ADI staff workers. Key informant interview respondents have highlighted that the interaction and relationship with health authorities in accessing client files is difficult for many communities, as there are both financial and jurisdictional challenges preventing staff from accessing client health charts in the eHealth system (i.e., viewing client's bloodwork results and prescriptions). A key informant interview respondent highlighted that "communities access to electronic charting, even if they are seeing someone in a nearby community, such as the homecare nurse or the foot care nurse, (they) can't see what their A1C is even though that's something they should be reporting on". The evaluation also identified a best practice in Nova Scotia in which the ADI staff collaborate with provincial health authorities to obtain access to their clients' health data for treatment purposes. They are also using the data received to drive their own health priorities and planning.
- Digital Disadvantage: As a consequence of the COVID-19 pandemic, many communities pivoted to providing activities and services online. However, some key informant interview respondents highlighted that digital disadvantagesFootnote 74 can negatively impact some client's abilities to participate in program activities and/or communicate with service providers. One key informant interview respondent noted that "a lot of providers are giving appointments on [MS] Teams or Zoom but if the community's internet is not adequate, they can't access people that way". Key informant interview respondents shared that significant effort was put into ensuring clients had access to services during the pandemic and maintaining communication with clients. One such key informant interview respondent shared that "through COVID, I text people. Some people only have phone out capabilities or run out of money half way through the month. It has been a real difficulty to talk to people and share. So, communication has been a real difficulty throughout the process (COVID)".
- Food Insecurity: The impact of food insecurity is a key challenge faced by many of the communities that the ADI operates in. This is further discussed in section 9 of this report.
7.2 Canada's Tobacco Strategy (CTS)
7.2.1 Traditional Tobacco Practices
Finding 14: While the evaluation did not yield adequate information to provide conclusive findings on the effectiveness of the ISC component of the Canada's Tobacco Strategy during the timeframe of this evaluation, Indigenous-led reporting showed success around key indicators towards outcomes. The integration of traditional tobacco practices is reported to be successful in this evaluation and in past reports.
The renewed Federal Tobacco Control Strategy (FTCS) was rebranded as the Canada Tobacco Strategy (CTS) in the 2018 Budget. The First Nations and Inuit component of the CTS is a knowledge development initiative that began in 2014-15 under the FTCS and continued through the timeframe of this evaluation. It supported the development and implementation of comprehensive, holistic, culturally appropriate tobacco control projects that were focused on reducing non-traditional tobacco use, while maintaining respect and recognition for traditional forms and uses of tobacco within communities. The approach was organized around six essential intervention elements: 1) Protection; 2) Reducing access to tobacco products; 3) Prevention; 4) Education; 5) Cessation; and, 6) Research and Evaluation. The initiative focused on establishing comprehensive tobacco control approaches and interventions, and in disseminating successes and knowledge acquired among First Nations and Inuit communities. It is important to note that as a result of the COVID-19 pandemic, there were fewer responses in key informant interviews and the online survey (n=43/115) from respondents who self-identified as being involved in the CTS sub-program. To mitigate for this limitation, additional secondary data, including was utilized to complement survey responses and provide further analysis.
As of 2017-18, under the FTCS, 56% of First Nations and Inuit communities had access to tobacco control activitiesFootnote 75. Under the former FTCS, which was project-based, ISC supported the implementation of 16 projects and 3 strategies, reaching 386 of 689 First Nation and Inuit communities (approximately 56%). In 2017-18, the results were: an increase in the number of indoor and outdoor smoke-free spaces from 640 to 1225; the passing of 173 new smoking-related resolutions at the local level; and an increase in participation of community members in smoking cessation programs/ interventions, with 74% of individuals who completed a cessation program/ intervention either reporting reduced tobacco use (24%) or quitting commercial tobacco use (3.0%)Footnote 76. This cessation rate is considered a significant success and surpasses estimated cessation rates among other segments of the general Canadian population.
Overall, the survey indicated that 53% of respondents (n=30) agreed or strongly agreed that CTS was operating effectively to reduce commercial tobacco use. As well, when asked on the survey, the extent to which respondents believed that CTS was successful in implementing the essential intervention elements, survey respondents reported the following (n=32):
- 22% of respondents reported success in reducing access to commercial tobacco use (44% were neutral);
- 31% reported success in preventing use of commercial tobacco (38% were neutral);
- 65% reported success in tobacco education (26% were neutral);
- 44% reported success in commercial tobacco cessation (34% were neutral); and
- 25% reported success in research and evaluation (50% were neutral).
Through key informant interviews, cessation efforts were identified as being a major challenge. In fact survey respondents also highlighted challenges pertaining to cessation efforts, stating: "everyone is at their own pace when it comes to reducing or quitting their use of Commercial Tobacco. In some cases, it is hard to meet individual needs as we don't have nicotine replacement therapy readily available and sometimes it is hard for rural clients to get into their family physicians or to get the follow-up they need. Clients often relapse or give up on quitting". Another survey respondent expressed that "in this region, smoking is still virtually epidemic: over 40% of people smoke, and children and youth start smoking at very young ages. We still need to de-normalize smoking. Also, most smokers are not open to trying to quit with NRT (nicotine replacement therapy) or medications; (or) they prefer to use "willpower". The Regional Health Survey found that when asked why smokers quit, nearly two-thirds (65.2%) said they had quit because they chose a healthier lifestyleFootnote 77.
Survey respondents also noted major challenges in retaining staff, promoting community engagement, and engaging individuals before they begin smoking. A survey respondent suggested that it may be important to engage individuals before they are even ready to quit smoking: "members only participate in activities when they are ready to quit. Trying to have participants even if they aren't ready so when they are they know what to expect or see for services". Key informant interview respondents highlighted the increased use of vaping and cannabis and they have suggested that this be included in program activities.
Tobacco use by First Nations peoples has a rich tradition going back millennia. The First Nation and Inuit Community of PracticeFootnote 78, that helped to inform the Future Federal Tobacco Control in Canada provided their views on sacred Tobacco: "For many First Nations people, natural tobacco is considered a powerful traditional medicine that brings people together. It can be used in a positive way, to give blessings, while fishing and hunting, and to ask guidance from knowledge keepers. Natural tobacco is often given back to Mother Earth or to the water or simply carried in bundles. It is one of the four natural medicines the First Nation peoples hold most sacred. As First Nations are revitalizing their culture after hundreds of years of colonization and assimilation policies, sacred tobacco is a medicine that is helping many on the healing journey. Respecting tobacco as the Creator intended is helping individuals to respect their mind, bodies, and spirit". Traditional tobacco is completely different from commercial tobacco sold today and used by First Nations peoples for ceremonial purposes. Additionally, the First Nations Information Governance Centre reports that "habitual or recreational cigarette smoking, as a non-traditional use of commercial tobacco, has been cited as the most common form of tobacco misuse today"Footnote 79. Given the important cultural and spiritual roots of tobacco in many First Nations, tobacco cessation research has shown that culturally appropriate interventions bolster the effectiveness of Indigenous tobacco programming. According to Habash et al (2021), many First Nations people believe that "tobacco is a sacred plant that has spiritual and medicinal purposes. Unlike commercial tobacco, the growth, use and purpose of sacred tobacco have specific culturally based protocols that are deeply rooted in First Nations' traditions"Footnote 80. This understanding of tobacco use, is pertinent to delivering programming that effectively meets the needs of community. A literature scan of smoking intervention programs for Indigenous Peoples found that the programs must be tailored for those it is targeting, incorporate the views and suggestions of key members of the population, and involve Indigenous health care workers whenever possible. The RHS found that 74% of First Nations youth aged 12-17 who did not smoke also stated that traditional teachings were either somewhat or very important to themFootnote 81. They also cited connections to spirituality as a protective factor for youth as those who placed higher importance on traditional cultural activities reported higher emotional competence, which was found to reduce smoking ratesFootnote 82.
7.3 Nutrition North Canada Nutrition Education Initiatives (NNCNEI)
7.3.1 Program Eligibility Requirements
Finding 15: The flexibility of the Nutrition North Canada Nutrition Education Initiatives is a contributing factor in the program's success, despite challenges reported with the program's eligibility requirements.
The overall goal of the NNC - Nutrition Education InitiativesFootnote 83 is to complement existing NNC programs with a nutrition focus by supporting retail and community-based nutrition education initiatives. In doing so, the NNC - Nutrition Education Initiatives aims to encourage and increase knowledge of healthy eating habits and develop skills for the selection and preparation of healthy foods in fully eligible First Nations and Inuit communities. NNC – Nutrition Education Initiative is community driven, with programming varying from community to community. The program is flexible, allowing for communities to choose the types of activities that serve their needs. From annual program reporting, between 2013-14 and 2018-19, funding recipients delivered almost 18,000 nutrition education activities such as promotion of healthy food knowledge, food skills development, in-store taste tests and grocery store tours, and traditional food harvesting and preparation. In 2018-19 aloneFootnote 84, at the community level, over 4,000 nutrition education activities were delivered to more than 44,000 participants, and an estimated 70% of funding recipients indicated that community members had increased their knowledge of healthy eating and skills and were choosing and preparing healthy food.
Approximately half (52%) of survey respondents agreed or strongly agreed that the NNC Nutrition Education Initiatives were operating effectively (n=25). As well, survey respondentsFootnote 85 and key informant interviewees reported successes in the integration and promotion of traditional foods in the Nutrition North Canada Nutrition Education Initiatives programming and working closely with the ADI program. Access to traditional foods and supporting knowledge transfer/exchange is important to the development of food sovereignty in all communitiesFootnote 86. This includes cooking with traditional foods in cooking classes, planting and maintaining community gardens, and promoting traditional hunting practices. This is in-line with the recommendations from the First Nations Food, Nutrition and Environmental Study which supports the promotion of traditional food systems to tackle issues of food security/sovereigntyFootnote 87. The study found traditional foods to have multiple core values for First Nations, both cultural, spiritual, and traditional, and called for the support of First Nations-led healthy food educationFootnote 88. During the 2018-19 data collection period, the CBRT reports that among the communities that reported delivering a HL program (n=314), 57% provided school-based feeding programs, 63% provided food vouchers, 51% provided good food boxes, 65% provided community gardens, 40% provided grocery store tours, 91% provided healthy eating awareness/education, 79% provided tradition harvesting/food preparation, and 89% provided cooking session/classes.
The recent Horizontal Evaluation of Nutrition North CanadaFootnote 89 found that given the nature of initiatives funding, inadequate data collection and reporting makes it difficult to attribute particular results of Nutrition Education Initiatives to the NNC program. However, it did report that the growing incidences of participation suggest that there is widespread interest in healthy eating. Thus, it can reasonably be concluded that participants are likely acquiring knowledge and skills to eat healthier. As another way to attribute probable program success, the relationships between the program funding and the extent of participation was highlighted in the evaluation, suggesting that increased investment expanded education initiatives to more communities (see figure below)Footnote 90.
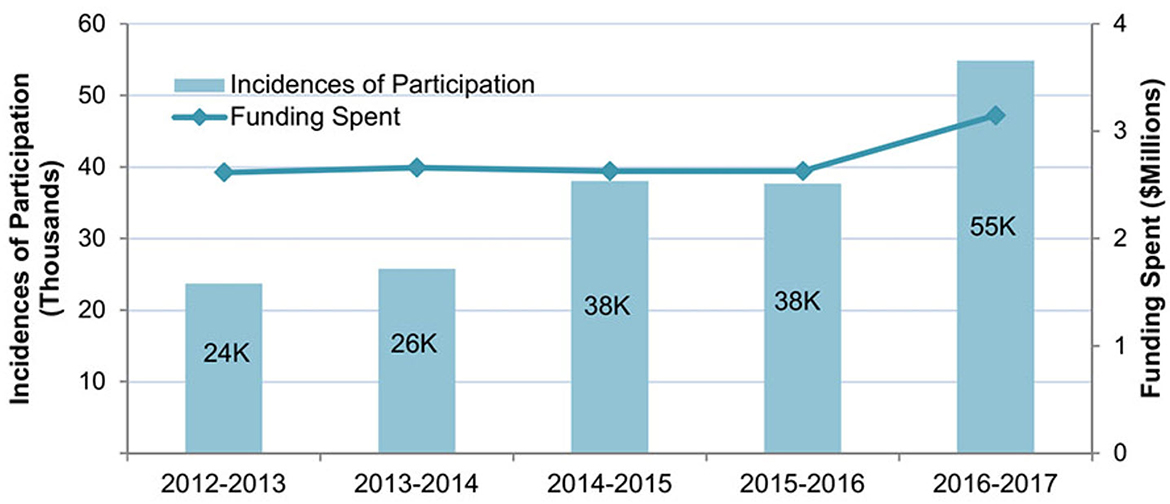
Text alternative for Figure 1: Incidences of Participation Relative to Funds Spent on Nutrition Education Initiatives Funded by NNC between 2012-13 and 2016-17
Figure 1 is a mixed line and bar graph that compares the incidences of participation relative to funds spent on nutrition education initiatives funded by Nutrition North Canada (NNC) between 2012-13 and 2016-17.
In 2012-13, the NNC program spent $2,614,280 and had 24,000 participants. In 2013-14, the NNC program spent $2,659,880 and had 26,000 9participants. In 2014-15, the NNC program spent $2,626,323 and had 38,000 participants. In 2015-16, the NNC program again spent $2,626,323 and had 38,000 participants. In 2016-17, the NNC program spent $3,145,573 and had 55,000 participants.
The evaluation found that there is a higher demand for certain types of activities such as traditional food knowledge and skills and retail-based nutrition knowledge and awareness. The evaluation of Nutrition North CanadaFootnote 91 also found that activities where food was offered were often the most favoured, be it cooking classes or food tasting, and that targeted cooking classes for school children and Elders were often successful.Footnote 92
Many key informant interview respondents expressed concerns around the eligibility for Nutrition Education Initiatives. Funding is currently dependent on the First Nations community meeting eligibility criteria for the NNC subsidy administered by CIRNAC. Key informant interview respondents expressed that the NNC - Nutrition Education Initiatives remains relevant for all communities. Key informant interview respondents also expressed that the current eligibility criteria does not meet the needs of many communities with one partner organization respondent, with one stating: "some of our drive-in communities are four-plus hours from a town with a grocery store and because they're not fly-in, they're not eligible for Nutrition North". Key informant interview respondents also expressed the needs to expand the eligibility criteria to allow for a wider range of communities to receive this program.
With the increasing prices of food in the north, coupled with travel expenses for community workers that service multiple communities, key informant interview respondents have all expressed concerns regarding the inadequacy of funding for the NNC Nutrition Education Initiatives. Ultimately, these high food prices make cooking classes, and other engagement sessions expensive for the program. When asked what the key challenges in delivering NNC Nutrition Education Initiatives were, many survey respondents highlighted funding concerns, for example: "lack of funding, can't hire full-time staff",insufficient funding", and "staffing and housing for contractors who travel here". Additional funding was also noted to be required to facilitate training for staff.
8.0 Summary of Best Practices & Lessons Learned
8.1 Best and Preferred Practices
A number of best and preferred practicesFootnote 93 have been identified for the Healthy Living program. Contributing to the success of these best practices (to varying degrees) have been the following key principles:
- A flexible program design and delivery allows staff to implement culturally relevant activities to the local community and its members;
- A flexible program design and delivery allows for increased accessibility and better engagement from community members;
- Activities rooted in community-led design and delivery have a higher rate of success and positive outcomes;
- Encouraging the roll out of the HL program across multiple service providers (doctors, hospitals, community groups);
- A significant number of community partners have suggested that having an Indigenous cultural support worker would greatly enhance the inclusion of cultural/ traditional teachings and practices in HL sub-programs at the community level;
- Encouraging partnerships with other ISC programs/ services that would create more opportunities for increased collaboration and for natural partnerships to take hold with the aim of having less communities working in silos; and;
- Lastly, integrating a chronic disease approach in HL sub-programs, and focusing on implementing a holistic approach to addressing chronic disease.
8.2 General Best Practices Identified
The following best practices (not exhaustive) are a collection of practices identified by key informant interview respondents that have shown success in the delivery of the Healthy Living Program and that have the potential to be implemented across the HL sub-programsFootnote 94.
Incorporating Traditional Tobacco Practice
- The integration of traditional tobacco into the program was the most widely reported best practice by regional and community partners in key informant interviews relating to CTS. This includes growing and harvesting tobacco, providing elder-led teachings of traditional tobacco, and promoting the use of traditional tobacco grown without chemicals. Carson et al. emphasized the importance of developing programming with community members and where possible, involving Indigenous health care workers in the delivery of the programFootnote 95. Multiple regions highlighted the significance of engaging Elders to teach youth of the sacred medicine of traditional tobacco. A key informant interview respondent noted that by teaching traditional versus commercial tobacco use, the program is able to take a culturally informed harm reduction approach to tobacco use. Informants emphasized the need for the program to be flexible to adapt to community needs and traditions.
Intra-Regional ADI Working Groups:
- An achievement of the ADI is the strong engagement of regional partners at their respective regional community of practice groups, which some key informants have referred to as "working groups". Partners across most regions expressed a high degree of satisfaction with this participatory working method and stated that the opportunities to build strategic partnerships with other colleagues at both the regional and community levels have been beneficial.
Land Based Activities:
- Communities across the country have shifted more towards land-based activities and integrating an environmentally focused approach to education. Communities have focused on reaching various participants (children, youth, elders), specifically exposing community members to traditional harvesting practices and traditional foods.
NIDA Resource Booklet:
- The National Indigenous Diabetes Association (NIDA) developed a resource booklet titled "Gifts from our Relations"Footnote 96, a food guide that highlights commonly consumed traditional foods (both plants and animals) that can be found on Indigenous lands. It provides practical guidance and insight into original food consumption as a means to reduce type 2 diabetes in First Nations communities. The focus of the resource booklet highlights how various consumed traditional foods (i.e., fish, seafood, seaweed, rice, plants, berries) provides specific vitamins for those living with diabetes and looking to self-manage the disease through diet. This is found to be highly beneficial by many of the community partners interviewed as the guide was developed by two nutritionists and these are viewed by ADI staff as resources materials that are familiar to Indigenous clients.
8.3 Regional Specific Best Practices
Manitoba: Partnership Models
- Diabetes Integration Project (DIP): The Diabetes Integration Project in Manitoba is a mobile diabetes care and treatment model that was developed to provide services on-reserve to support First Nation adults living with type 2 diabetes to prevent, screen, and/or delay the complications of diabetes. The DIP has maintained strong relationship with other community initiatives to ensure there is limited duplication of services. A barrier within DIP is that it is only available in a third of the Manitoba communities and without additional financial investment, many of the other communities across the province will not have access to the mobile clinics.
- Food Security Coordinator: The Four Arrows Regional Health Authority has been employing a full time Manitoba First Nations food security coordinator since 2011, who acts as liaison for all 63 First Nations communities in Manitoba. This position promotes and increases awareness about food security, supports food sovereignty and empowers communities to produce food locally (through gardens, greenhouses and raising livestock) and through sustainable ways, encourages the continuation of traditional food sharing networks. The training and support provided by this position is offered through various means such as telehealth sessions, by email, telephone, on-line, and when possible, through community visits. ISC provides funding for the position through the ADI.
- Tribal Diabetes Coordinators (TDC): The TDC role supports community ADI workers in capacity development at the tribal council level so that they can provide increased support to their communities. The TDC is commonly supported by a nurse, dietician, or diabetes related specialist. This is a role that communities find beneficial as TDCs act as a "go to resource" for ADI staff and can provide staff with technical support. There is also an opportunity for knowledge mobilization and has helped to reduce staff turnover rates among ADI workers.
Atlantic Region: Screening and Management
- Diabetes Self-Management Journey: The Atlantic region delivers the "Diabetes Self-Management Journey," an annual program that is offered in each province by a diabetes community consultant in partnership with diabetes educators from the local regional health authority, pharmacy and community elders. Communities are invited to send participants living with diabetes and their respective support individual (family member, friend etc.) to attend a 3-5 day culturally-relevant diabetes self-management workshop that focuses on topics that support the individual living with diabetes including nutrition, medications, physical activity, menu planning, traditional foods, mental wellness, etc. The journeys provide evidenced-based recommendations and enhance self-management skills for individuals living with diabetes and their support person. The region has received positive feedback from community members living with diabetes on this educational program. It is also viewed by community partners as a beneficial opportunity for people to share and learn together with people who are living with diabetes. The Atlantic region has been providing this annual education for over 15 years.
Alberta Region: Food Security Activities
- Food Security: The Prevention Program Committee of Alberta Co-Management developed the Alberta First Nation Food Security Strategy through their Food Security Working Group. The development of this strategy followed a number of steps including an environmental scan of learnings and practices from food security initiatives in a First Nations or Indigenous context. The development of this strategy also involved a series of community engagement sessions, where all First Nations in Alberta were invited to participate, as well as a series of stakeholder consultations. Creating this Food Security Strategy by Alberta First Nations is one of the first steps towards achieving food sovereignty and control.
- The Alberta First Nations Food Security Working Group in partnership with the Alberta First Nations Elders' Advisory Group developed an Alberta First Nations Food Sovereignty Declaration in order to increase access to traditional foods in community programs and facilities.
8.4 Lessons Learned (General Guiding Principles)
The following are general guiding principles regarding lessons learned in community programming design, as shared in key informant interviews:
- It is important to focus on meeting the individual where they are along the health spectrum;
- Relationship building is key in community development work and it is important to focus on building relationships with community members first, rather than solely focusing on the behavioural/ biomedical aspects of ADI;
- When programs focus on creating an environment that is culturally safe and trauma-informed for community participants, it helps to build trust and relationships;
- Integrating cultural practices into Healthy Living activities, such as Indigenous storytelling, can be a powerful and empowering tool for learning and sharing intergenerational experiences and knowledge;
- An ability to adapt programming to meet the needs and circumstances of a community is desirable for Healthy Living. What may be effective for one Nation/ community may not be effective for another; and
- The ADI programs that have community champions are seen to be highly effective at helping to build community level ownership.
9.0 Cross Cutting Themes
9.1 Climate Change
Finding 16: Impacts on the food supply chain and changes in the availability of country food as animal migration patterns change can potentially impact the Healthy Living Program, specifically remote and isolated communities.
The effects of climate change on the Healthy Living Program are potentially significant, especially in the context of remote and isolated communities. Key informant interview respondents noted that there are two elements to consider in terms of climate change effects as they relate to HL Programs: impacts on the food supply chain and changes in the availability of traditional or country foods as a result of changes to the environment and ecosystems. Both of these have the potential to impact the availability of nutritious foods that are important elements of the ADI and NNC Nutrition Education Initiatives, as well as food security itself in northern, remote and isolated communities.
Firstly, climate change has an impact on food security, and as a result can impact the HL Program. Many community-based activities supported through HL sub-programs seek to improve access to and availability of nutritious food, for example by incorporating healthy store bought and traditional foods, and supporting gardening. Survey respondents and key informant interview respondents noted that climate change is causing a less reliable food supply chain, as once reliable ice roads used for transport of food are increasingly impassable or are in operation for a shorter period of time due to late freeze-up/early melting. This has the potential to delay delivery of nutritious and healthy foods (i.e., fruits and vegetables) required to mitigate the effects of diabetes and other chronic health conditions whose treatment is positively influenced by diet.
Secondly, impacts such as changes in animal migration patterns, extreme weather conditions, and temperature changes have had an impact on the local availability of plants and animals leading to deleterious effects on food security. Survey respondents also noted that due to climate change, the migration patterns of game animals have been altered in some cases, which is increasingly deleterious for those communities whose food security relies more on the availability of traditional country foods as a larger portion of a healthy diet. Survey respondents also highlighted in the survey the need to increase collaboration with schools to promote healthy eating: "there are still some gaps with grocery stores in Northern communities keeping [their] stock up. Cannot find fresh fruit and vegetables in the stores. Not much opportunity for the school curriculum to allow time for Diabetic educator to do teaching on healthy eating. Schools are a vital part of learning about healthy eating and need to collaborate more with the Dietitian and Diabetes Educator".
9.2 Service Transfer
Finding 17: As part of the ISC strategic plan, the program is working towards eventual service transfer. However, there remain hurdles to transferring financial responsibilities to communities directly.
Readiness for transfer of Healthy Living programming directly to communities was found to be varied, but overall, key informant interview respondents highlighted that work needs to be done before the program would be ready for service transfer. Indeed, the fact that many communities over all regions are incrementally moving towards flexible funding arrangements may be viewed as a positive step in the service transfer continuum. Still, there remain hurdles. Most significantly, key informant interview respondents cited that the role that ISC provides in terms of financial oversight (i.e., management tools, databases, etc.) is not yet being transferred to community health directors and staff, which is an important administrative aspect of service transfer. This factor impedes the ability of ISC regional offices to adapt to changing community need-based priorities. Additionally, concerns were raised by key informant interview respondents around the likelihood of additional funding requests being approved once service transfer is complete. The current bidirectional relationship between the federal government and communities fosters accountability to ensure that Healthy Living programs are adequately funded. Without this relationship, some respondents expressed concerns that additional funding requests may not have as much priority.
9.3 Early Impacts of COVID-19
The COVID-19 pandemic has marked effects on Healthy Living programming, just as it has on society and programming initiatives as a whole. The greatest impact noted by key informant interview respondents and survey respondents has been that many planned activities (e.g., gathering in groups for activities such as cooking classes, school engagements) have effectively been delayed or put on hold. The reasons for the delays include community access restrictions/physical distance measures for non-community members; redeployment of community health workers to the COVID-19 response; and capacity limits within structures where programming would normally occur. Indeed, community priorities have generally been re-directed to focus on mitigating the spread of the virus, which has removed resources away from not only health-related programming, but also in other areas served by ISC (i.e., infrastructure). Additionally, COVID-19 has further amplified the food security challenges faced by many vulnerable communities, for reasons noted above.
In many cases, the Program has successfully pivoted to providing programming online by leveraging communications technology and social media (for example, cooking classes delivered via Facebook rather than in-person). While this has worked effectively in some areas, it has been more difficult in remote areas with limited internet access. It is not clear from key informant interviews whether emergency COVID-19 funding was provided to the Healthy Living programs, or how it may have been utilized. However, due to the flexible nature of Healthy Living funding, respondents noted that in some cases it has been utilized to augment and support COVID-19 relief efforts.
Aside from the above, an additional and significant reality to consider that could potentially impact the Program in the future are the potential effects of COVID-19 on the Indigenous population in general. According to the National Advisory Committee on Immunization, Indigenous individuals are also more likely to have underlying health conditions (for example, diabetes) that could make a bout of COVID-19 more deadly. The proportion of Canadians who identify as Indigenous and have at least one underlying medical condition associated with an increased risk of severe COVID-19 is higher compared to other Canadians for every age category above 20 years of age. Exacerbating this is the reality that Indigenous and remote communities face increased COVID-19 risks due to possible aggravating conditions, such as limited access to clean water, lack of health professionals/services, a high prevalence of chronic diseases, and crowded living conditions.
10.0 Conclusions
There is a clear demonstrated need for the Healthy Living Program to continue its efforts to address the gaps in health outcomes between First Nations peoples and the general Canadian population. So long as diabetes, use of commercial tobacco, and food insecurity remain disproportionately high among First Nations peoples, the Healthy Living Program will remain relevant to health and well-being of First Nations communities.
A key strength of the Healthy Living Program is the community-led aspect. Community health leaders are able to determine what the needs of their communities are and conduct activities to best serve them. This tailored and flexible approach was reported to be well received. However, with this flexibility also comes a reduced reporting burden, resulting in less data tracking and measurement of the impact of programming.
The flexible funding and wide scope of the program activities allows for collaboration between the sub-programs, particularly between the ADI and the NNC Nutrition Education Initiatives. These programs are able to collaborate and share activities and funding to optimize their reach.
The ADI is a well-established and well-known program providing diabetes education, prevention, and treatment in First Nations communities. ADI was reported to have high satisfaction and to be effective in the prevention and management of type 2 diabetes. The most notable success was found in its activities related to community-based health promotion and primary prevention.
CTS provides funding to support Indigenous communities across Canada in the development and implementation of distinct First Nations, Inuit and Métis approaches to reduce commercial tobacco use. The successes lie in the focus on delineating between commercial and traditional tobacco. Key informant interview respondents championed the integration of traditional tobacco uses, education, and cultivation.
NNC Nutrition Education Initiatives provide a venue for healthy eating knowledge and skills. With the incorporation of traditional foods, hunting practices, and community gardens, the program allows participants to build skills needed for healthier lives. Key informant interview respondents have highlighted that this program may be beneficial to a wider range of communities, not only those who meet the eligibility requirements for NNC currently set out under CIRNAC.
The evaluation found that HL sub-programs do not in any way exclude diverse members of communities (2SLGBTQIA+, youth, elders, etc.). However, in some cases certain activities garner less attendance because many sessions are held during working hours.
The realities of climate change was found to have a potential impact on food security, especially in remote and isolated communities. As the climate changes, this will likely impact the availability of country food as animal migration patterns alter, resulting in the possibility that food may become more scarce. This fact, coupled with climate change impacts on the general food supply chain, has already begun to occur.
Although transfer of HL services to communities was not a main point of inquiry in this evaluation, ISC-FNIHB has indeed taken positive steps on this continuum by moving away from set towards more flexible funding arrangements, which places the community as the arbiter of how health-related funds should be allocated, thereby having the opportunity to tailor programming to local needs. However, the administrative aspect of service transfer (i.e., management tools, financial oversight, databases, etc.) is an area where readiness is crucially lacking, along with concerns regarding funding requests to ISC from communities once service transfer is completed.
Finally, the COVID-19 pandemic has had marked effects on the HL Program, as it has also had on many ISC programs. The greatest impact has been on planned activities (e.g., gathering in groups for activities such as cooking classes, school engagements) that were effectively delayed or put on hold. Indeed, community priorities have generally been re-directed to focus on mitigating the spread of the virus, which has removed resources away from health-related programming.
Overall, the program's community-specific approach and flexible use of funding is the key to its success. While there are opportunities for improvement, the program received overall positive feedback across respondents. The program has allowed for communities to address chronic disease and food insecurity broadly with the ability to address their own priorities.
11.0 Recommendations
1. Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus); and gradual service transfer.
Data currently collected for the HL Program is based largely on the community-based reporting template (CBRT) and from the Regional Health Survey (RHS). While some community partners are required to submit annual CBRT reports to regional offices as a requirement of their funding agreement, others are not. There is an expressed need from community partners to develop standardized data tool(s) that can support community health staff to systematically collect and utilize quantitative data across sub-programs level, so that communities are able to effectively track performance and the achievement of program results equally across communities. There is also a need from partners for the development of additional data collection tools to support communities in both reporting on program activities and collect additional health data to help make decisions.
2. ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer.
Across the HL programming, there is concern that funding allocations are inadequate. As a result, community partners are facing considerable challenges in recruiting and retaining professional staff. When communities are unable to retain staff, they also face the potential loss of corporate and institutional knowledge across sub-programs, impacting the overall delivery of services. Exploring cost-effective methods to support community capacity, recruit and retain the right mix of talent, technologies, and professional development opportunities will better support communities reach their goals.
3. Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program.
Key informant interview respondents highlighted the success of incorporating traditional practices into the Healthy Living Program. Whether this was through growing traditional tobacco for ceremony, teaching of hunting practices for traditional foods, or community gardens, these activities were reported to garner support and enthusiasm from community members. Further integration of cultural/traditional practices would provide information sharing and consolidate best practices for communities just beginning to incorporate these practices. As well, the impacts of climate change on the HL program are potentially significant, and there are many community-based activities supported through HL sub-programs that seek to improve access to and availability of nutritious food, for example by incorporating traditional food and supporting gardening activities.
4. Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level.
Partners across all regions expressed a high degree of satisfaction with their respective working groups and expressed strong interest in further building linkages and strategic partnerships with other colleagues at both the regional and community level. To strengthen this approach, it is recommended that the national and regional ISC teams explore methods for information sharing between communities on the ways to include community members in program planning as well as around the activities which have garnered success. As well, supporting further partnership-building helps to breed innovation and creates opportunities for further collaboration and complementarity across the sub-programs. Thus, it may beneficial for partners to receive guidance and support on where cross-community and regional level partnerships can exist for sub-programs.
Appendix A: Evaluation Issues and Questions
The evaluation questions focus on issues of relevance and performance as required by the Treasury Board Policy on Results. The evaluation questions concerning the effectiveness of the program are organized to align with the logic model and to reflect the need for distinct learning from each sub-program. The evaluation questions also aim to learn about the relationships that exist between Indigenous communities and the department, and the journey towards service transfer.
- Relevance
- Is there a continued need for the Healthy Living Program, including its sub-programs, policy initiatives, and range of available services?
- What are the current and ongoing health issues contributing to the need for this program and how have these needs changed since the last evaluation?
- Effectiveness: Program
- To what extent has the Healthy Living Program achieved the expected program outcomes at the immediate and intermediate outcome levels of its logic model?
- To what extent are there service gaps within the HL program?
- To what extent are program funding recipients and clients aware of the resources available to them through the Healthy Living program?
- To what extent is the Healthy Living Program effective at reaching all community members (e.g. including from a Gender Based Analysis Plus perspective, etc.)?
- What is the degree of complementarity within the components of the HL program?
- How does the HL Program complement and ensure collaboration with other FNIHB-ISC programs and other government departments?
- What does success look like within the HL program?
- Effectiveness: Policy Development (Chronic Disease Prevention Policy, Nutrition Policy, Injury Prevention Policy)
- Are the HL policy areas effective tools to support the implementation of the HL program?
- Effectiveness: Aboriginal Diabetes Initiative
- Is the ADI operating effectively?
- Effectiveness: Canada's Tobacco Strategy
- Is Canada's tobacco strategy operating effectively?
- Effectiveness: Nutrition North Canada Nutrition Education Initiatives
- Are the Nutrition North Canada Nutrition Education Initiatives operating effectively?
- Efficiency and Economy
- What is the status of the recommendations put forward in the previous evaluation?
- Has the Healthy Living Program been managed and carried out efficiently and economically?
- Is there sufficient capacity (Human Resources, training, and financial resources) within the Healthy Living Program to achieve its intended objectives and outcomes?
- Are there appropriate performance measurement systems in place to track the progress of the Healthy Living Program?
- Are HL funding arrangements appropriate in supporting effective service delivery?
- Best Practices/Lessons Learned
- Within the Healthy Living Program, have best practices been identified?
- What are the challenges in delivering the Healthy Living Program?
- Relationships
- Are relationships between and amongst HL Program stakeholders and partners effectively contributing to its implementation?
- How does the HL Program contribute to service transfer?
- How is climate change impacting HL outcomes?
Appendix B: Logic Model
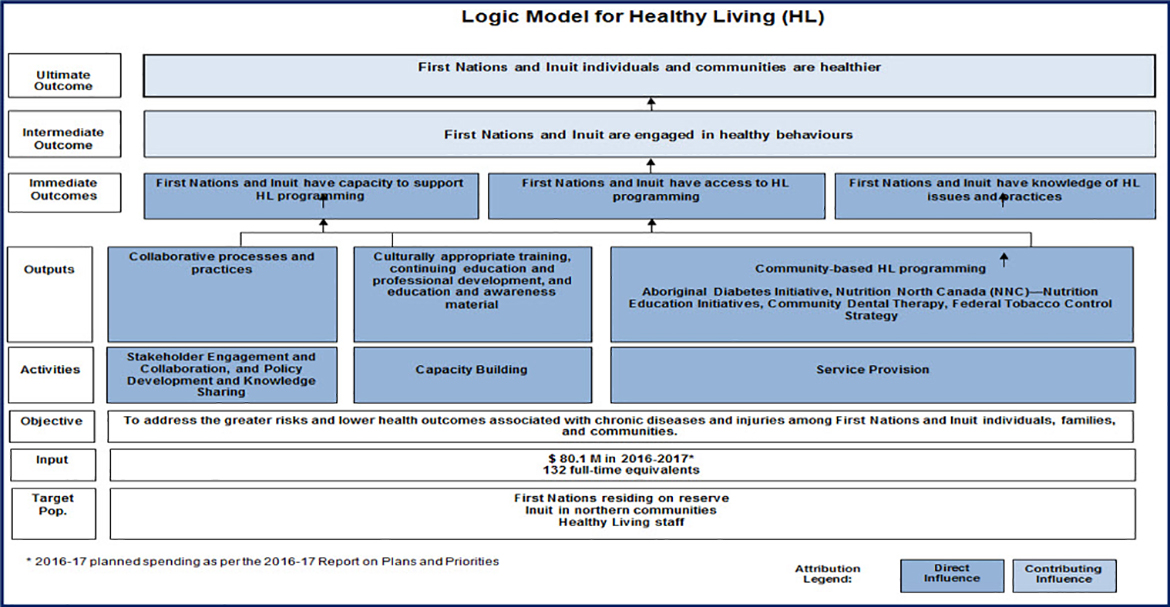
Text alternative for Appendix B: Logic Model
Appendix B is the logic model for the Healthy Living Program.
The 'Target Population' of the Healthy Living Program is "First Nations residing on reserve, Inuit in Northern communities, and Healthy Living Staff."
The 'Inputs' for the Healthy Living Program are $80.1 M in planned spending in 2016-2017 (as per the 2016-17 Report on Plans and Priorities) and 132 full-time equivalent staff.
The 'Objective' of the Healthy Living Program is "To address the greater risks and lower health outcomes associated with chronic diseases and injuries among First Nations and Inuit individuals, families and communities."
The 'Activities' of the Healthy Living Program are 1) stakeholder engagement and collaboration, policy development and knowledge-sharing, 2) capacity building, and, 3) service provision. These three areas of activity are considered to have a "direct influence" on the program.
The 'Outputs' of the Healthy Living Program are 1) collaborative processes and practices, 2) culturally appropriate training, continuing education and professional development, and education and awareness material, and 3) community-based programming such as the Aboriginal Diabetes Initiative, Nutrition North Canada (NNC), Nutrition Education Initiatives, Community Dental Therapy, and the Federal Tobacco Control Strategy. These outputs are considered to have a direct influence on the program. The outputs also support and contribute to the Immediate Outcomes of the Healthy Living Program.
The 'Immediate Outcomes' of the Healthy Living Program are 1) First Nations and Inuit have capacity to support HL programming, 2) First Nations and Inuit have access to HL programming, and 3) First Nations and Inuit have knowledge of HL issues and practices. These outputs are considered to have a direct influence on the program. The outputs also support and contribute to the Intermediate Outcomes of the Healthy Living Program.
The 'Intermediate Outcome' of the Healthy Living Program is "First Nations and Inuit are engaged in healthy behaviours". This outcome is considered to have a contributing influence on the Healthy Living Program. This intermediate outcome supports and contributes to the Ultimate Outcome of the program.
The 'Ultimate Outcome' of the Healthy Living Program is "First Nations and Inuit individuals and communities are healthier". The outcome is considered to have a contributing influence on the Healthy Living Program.
Appendix C: Logic Model Mapping
Below is a logic model mapping exercise to demonstrate the connection between the programs expected immediate outcomes and the related findings discussed in this report.
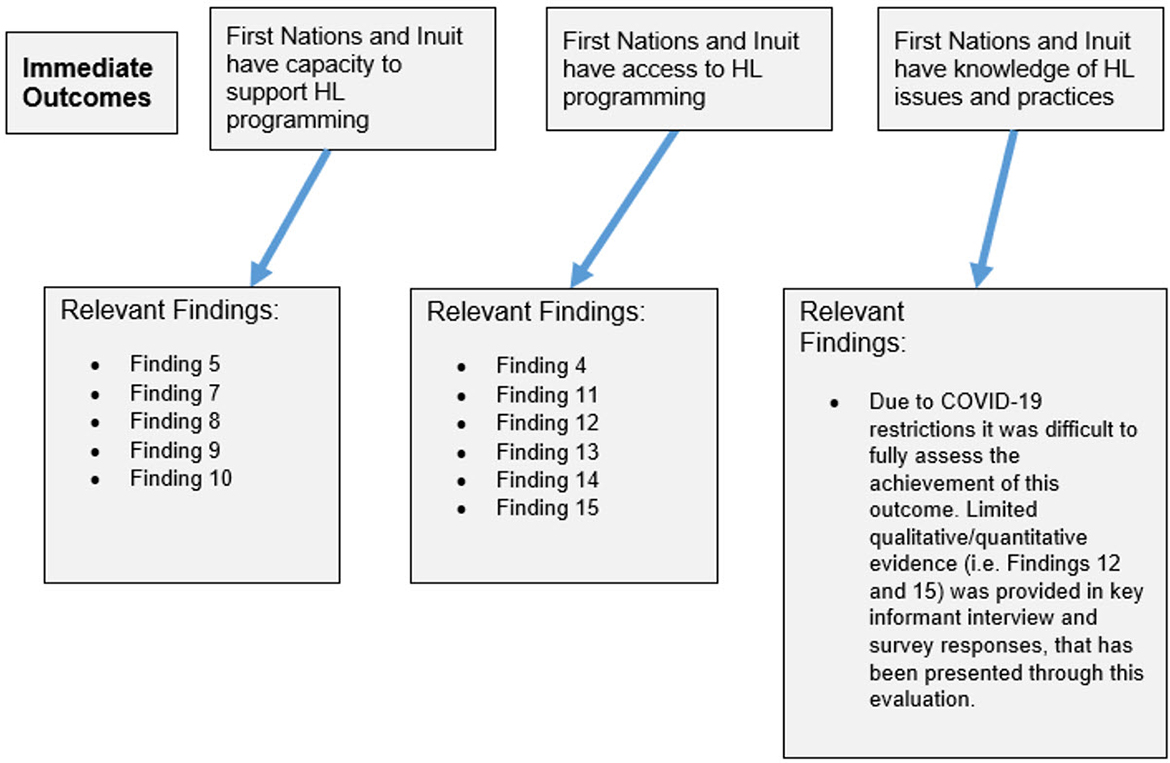
Text alternative for Appendix C: Logic Model Mapping
Appendix C is a logic model mapping exercise to illustrate the connection between the program's expected immediate outcomes and the related findings discussed in the evaluation report.
Relevant to the Immediate Outcome of "First Nations and Inuit have capacity to support HL programming" were the report Findings 5, 7, 8, 9, and 10.
Relevant to the Immediate Outcome of "First Nations and Inuit have access to HL programming" were the report Findings 4, 11, 12, 13, 14, and 15.
Regarding relevance to the Immediate Outcome of "First Nations and Inuit have knowledge of HL issues and practices" was the following note "Due to COVID-19 restrictions it was difficult to fully assess the achievement of this outcome. Limited qualitative/quantitative evidence (i.e. Findings 12 and 15) was provided in key informant interview and survey responses, that has been presented through this evaluation."
Appendix D: Summaries of Sub-Programs
The following appendix provides short summaries of all 3 sub-programs and includes succinct information on the evaluation scope, design, overview of each sub-program and subsequent key findings, as well as the evaluations recommendations. The aim of these summaries is to provide communities with a quick snapshot of the overall results of the evaluation.
Aboriginal Diabetes Initiative (ADI)
Evaluation Scope and Issues:
This evaluation covers the period from Fiscal Year 2013-14 to 2018-19 further to the Treasury Board requirements and includes each of the three Healthy Living sub-programs managed by FNIHB-ISC. The evaluation was undertaken to provide a neutral and evidence-based assessment of relevance, effectiveness and efficiency of the Healthy Living Program, including, Aboriginal Diabetes Initiative, Canada's Tobacco Strategy (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component), and Nutrition North Canada Nutrition Education Initiatives.
Evaluation Design and Methods
The evaluation was conducted in-house by the ISC Evaluation Directorate. It relied on a mixed-methods approach that included the following lines of evidence:
- A document and literature review
- 32 key informant interviews
- 168 online survey respondents
As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were not possible and were instead replaced by remote video/telephone interviews through various communication platforms.
Sub-Program Overview: Aboriginal Diabetes Initiative (ADI)
The ADI aims to reduce the prevalence of type 2 diabetes in First Nations and Inuit communities. ADI funding supports community-led health promotion and disease prevention programming, services and activities delivered by community workers and health service providers. During the time frame of this evaluation, ADI was the only sub-program within the Healthy Living Program funded universally, with all communities having access to ADI funding. The program consists of four components:
- Community-based health promotion and primary prevention;
- Screening and management;
- Capacity building and training; and,
- Knowledge mobilization.
The ADI program activities offered in each community vary based on local needs, priorities and capacity.
Key Findings: Aboriginal Diabetes Initiative (ADI)
Finding 12:The ADI has made progress to foster a high level of satisfaction among community partners
- Key informant interview respondents confirmed that there is a strong focus on delivering community-based promotion and prevention, because of the foundational role it plays in the overall design and delivery of the ADI, and that many communities are strong in delivering this component.
- Flexibility in program design also allows communities to implement activities that match the local needs, priorities, and realities.
- There is varying capacity in the level of screening and management effectiveness across regions. Of the 302 communities that responded to the diagnostic screening questionFootnote 97 asked in the community-based reporting template(CBRT), 54% reported that they delivered diagnostic screening during the 2018-19 reporting period. During that same reporting period, of the 299 communities that responded to the non-diagnostic screening question Footnote 98, 83% reported to have delivered non-diagnostic screening.
- Current capacity building and training efforts are on-going for staff supporting the ADI. Most key informant interview respondents noted that staff are keen in building upon their training repertoire. Specifically, staff noted interest in building their capacity to support clients and families with managing and improving their mental health and in having access to training that goes beyond the biomedical component of type 2 diabetes.
- In interviews across all regions, key informants have expressed a high degree of satisfaction with their many respective working groups, recognized the importance of tailoring activities to community needs and priorities, and expressed that the opportunities to build strategic partnerships with other colleagues at the regional and community levels have been beneficial for their work.
Finding 13: There are a few key challenges that may hinder the ADI from potentially meeting needs and priorities, including the impact of funding constraints, staffing challenges, technological disadvantages faced by some clients, and the impact of food insecurity.
A number of key challenges were identified in the document review, in interviews with key informants, and in survey responses. Below is a list of the key challenges that communities face as they work to deliver the ADI.
- Funding concerns: A lack of adequate funding (this is further discussed in section 6.4) is a concern for many key informant interview respondents. Specifically, respondents expressed that stagnant program funding impacts human resource capacity concerns, capacity building opportunities available to staff supporting ADI efforts, and hinders the program's ability to develop further.
- The remoteness of some First Nations communities has impacted program delivery in some communities, and this is further corroborated by key informant interview respondents Footnote 99.
- Regional and Provincial Health Authorities: The ability for communities to access their health data and/or electronic charting from both provincial and/or regional health authorities is an ongoing challenge faced by clients and many ADI staff workers.
- Digital Disadvantage: As a consequence of the COVID-19 pandemic, many communities pivoted to providing activities and services online. However, some key informant interview respondents highlighted that digital disadvantagesFootnote 100 can negatively impact some client's abilities to participate in program activities and/or communicate with service providers.
Recommendations
Based on the findings of this evaluation report, it is recommendedFootnote 101 that ISC:
- Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus; and gradual service transfer.
- ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer.
- Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program.
- Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level.
Canada's Tobacco Strategy (CTS)
Evaluation Scope and Issues:
This evaluation covers the period from Fiscal Year 2013-14 to 2018-19 further to the Treasury Board requirements and includes each of the three Healthy Living sub-programs managed by FNIHB-ISC. The evaluation was undertaken to provide a neutral and evidence-based assessment of relevance, effectiveness and efficiency of the Healthy Living Program, including, Aboriginal Diabetes Initiative, Canada's Tobacco Strategy (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component), and Nutrition North Canada Nutrition Education Initiatives.
Evaluation Design and Methods
The evaluation was conducted in-house by the ISC Evaluation Directorate. It relied on a mixed-methods approach that included the following lines of evidence:
- A document and literature review
- 32 key informant interviews
- 168 online survey respondents
As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were not possible and were instead replaced by remote video/telephone interviews through various communication platforms.
Sub-Program Overview: Canada's Tobacco Strategy (CTS)
The First Nations and Inuit component of the Federal Tobacco Control Strategy (FTCS) was a project-based knowledge development initiative that began in 2014-15 and continued through the timeframe of this evaluation. The FTCS provided proposal-based funding that supported the implementation of 16 projects and 3 strategies, reaching approximately 56% of First Nations and Inuit communities. The FTCS supported the development and implementation of comprehensive, holistic, culturally appropriate tobacco control projects that focused on reducing commercial tobacco use, while maintaining respect and recognition for traditional forms and ceremonial uses of tobacco within First Nation communities.
Key Finding: Canada's Tobacco Strategy (CTS)
Finding 14:While the evaluation did not yield adequate information to provide conclusive findings on the effectiveness of the ISC component of the Canada's Tobacco Strategy during the timeframe of this evaluation, Indigenous-led reporting showed success around key indicators towards outcomes. The integration of traditional tobacco practices is reported to be successful in this evaluation and in past reports.
- As of 2017-18, under the FTCS, 56% of First Nations and Inuit communities had access to tobacco control activitiesFootnote 102.
- Under the former FTCS, which was project-based, ISC supported the implementation of 16 projects and 3 strategies, reaching 386 of 689 First Nation and Inuit communities (approximately 56%).
- In 2017-18, the results were: an increase in the number of indoor and outdoor smoke-free spaces from 640 to 1225; the passing of 173 new smoking-related resolutions at the local level; and an increase in participation of community members in smoking cessation programs/ interventions, with 74% of individuals who completed a cessation program/ intervention either reporting reduced tobacco use (24%) or quitting commercial tobacco use (3.0%)Footnote 103.
- This cessation rate is considered a significant success and surpasses estimated cessation rates among other segments of the general Canadian population.
- Through key informant interviews, cessation efforts were identified as being a major challenge. In fact survey respondents also highlighted challenges pertaining to cessation efforts.
- Survey respondents also noted major challenges in retaining staff, promoting community engagement, and engaging individuals before they begin smoking. A survey respondent suggested that it may be important to engage individuals before they are even ready to quit smoking.
- Given the important cultural and spiritual roots of tobacco in many First Nations, tobacco cessation research has shown that culturally appropriate interventions bolster the effectiveness of Indigenous tobacco programming.
Recommendations
Based on the findings of this evaluation report, it is recommendedFootnote 104 that ISC:
- Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus; and gradual service transfer.
- ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer.
- Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program.
- Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level.
Nutrition North Canada Nutrition Education Initiatives (NNCNEI)
Evaluation Scope and Issues:
This evaluation covers the period from Fiscal Year 2013-14 to 2018-19 further to the Treasury Board requirements and includes each of the three Healthy Living sub-programs managed by FNIHB-ISC. The evaluation was undertaken to provide a neutral and evidence-based assessment of relevance, effectiveness and efficiency of the Healthy Living Program, including, Aboriginal Diabetes Initiative, Canada's Tobacco Strategy (formerly the Federal Tobacco Control Strategy – First Nations and Inuit Component), and Nutrition North Canada Nutrition Education Initiatives.
Evaluation Design and Methods
The evaluation was conducted in-house by the ISC Evaluation Directorate. It relied on a mixed-methods approach that included the following lines of evidence:
- A document and literature review
- 32 key informant interviews
- 168 online survey respondents
As data collection occurred in the context of the COVID-19 pandemic with the resultant travel restrictions, direct site visits were not possible and were instead replaced by remote video/telephone interviews through various communication platforms.
Sub-Program Overview: Nutrition North Canada Nutrition Education Initiatives (NNCNEI)
Nutrition North Canada is a Government of Canada program that helps make nutritious food and some essential items in isolated eligible northern communities available through a retail subsidy and a Harvester's Support Grant delivered through, Crown-Indigenous Relations and Northern Affairs Canada (CIRNAC), and through NNC Nutrition Education Initiatives supported by Indigenous Services Canada (ISC) and the Public Health Agency of Canada (PHAC).
NNC Nutrition Education Initiatives are funded through ISC to support culturally appropriate retail and community-based nutrition education activities in eligible isolated northern First Nations and Inuit communities. Activities focus on increasing knowledge of healthy eating and developing skills in the selection and preparation of healthy store-bought and traditional or country foods. Communities decide which activities to undertake based on their local needs and priorities.
Key Finding: Nutrition North Canada Nutrition Education Initiatives (NNCNEI)
Finding 15: The flexibility of the Nutrition North Canada Nutrition Education Initiatives is a contributing factor in the program's success, despite challenges reported with the program's eligibility requirements.
- NNC – Nutrition Education Initiative is community driven, with programming varying from community to community.
- The program is flexible, allowing for communities to choose the types of activities that serve their needs. From annual program reporting, between 2013-14 and 2018-19, funding recipients delivered almost 18,000 nutrition education activities such as promotion of healthy food knowledge, food skills development, in-store taste tests and grocery store tours, and traditional food harvesting and preparation.
- In 2018-19 aloneFootnote 105, at the community level, over 4,000 nutrition education activities were delivered to more than 44,000 participants, and an estimated 70% of funding recipients indicated that community members had increased their knowledge of healthy eating and skills and were choosing and preparing healthy food.
- The recent Horizontal Evaluation of Nutrition North CanadaFootnote 106 found that given the nature of initiatives funding, inadequate data collection and reporting makes it difficult to attribute particular results of Nutrition Education Initiatives to the NNC program. However, it did report that the growing incidences of participation suggest that there is widespread interest in healthy eating. Thus, it can reasonably be concluded that participants are likely acquiring knowledge and skills to eat healthier.
- The evaluation also found that there is a higher demand for certain types of activities such as traditional food knowledge and skills and retail-based nutrition knowledge and awareness.
- Many key informant interview respondents expressed concerns around the eligibility for Nutrition Education Initiatives. Funding is currently dependent on the First Nations community meeting eligibility criteria for the NNC subsidy administered by CIRNAC. Key informant interview respondents expressed that the NNC - Nutrition Education Initiatives remains relevant for all communities.
- Key informant interview respondents also expressed the needs to expand the eligibility criteria to allow for a wider range of communities to receive this program.
Recommendations
Based on the findings of this evaluation report, it is recommendedFootnote 107 that ISC:
- Work with the ISC Chief Data Officer (CDO), ISC Chief Information Officer (CIO) and the ISC Director General responsible for Performance Measurement to liaise with First Nations partners to support the development of a data strategy to improve the availability of Healthy Living performance data at the community, regional and national levels. Options should take in to consideration (but not be limited to): Indigenous data sovereignty; data sharing mechanisms; data standardization; reducing reporting burdens; Gender Based Analysis Plus (GBA Plus; and gradual service transfer.
- ISC to work with First Nations and health systems partners to explore potential mechanisms for increased, sustainable funding to better support community capacity in the design and delivery of Healthy Living programming based on the unique needs and priorities of communities, taking into consideration remoteness and gradual service transfer.
- Support First Nations and health systems partners to continue incorporating Indigenous-led principles or a potential framework that highlights and integrates traditional practices and teachings into the Healthy Living program.
- Building on best practices, explore opportunities to support the sharing of information among Healthy Living workers and across sub-programs, as a way to continually improve efficiencies and identify common needs and best practices at the regional and community level.