Evaluation of Clinical and Client Care Program 2012-2013 to 2016-2017
Final Report
August 2018
Format PDF (415 Ko, 51 pages)
Table of contents
List of Acronyms
| ACLS |
Advanced Cardiac Life Support |
|---|---|
| AHHRI |
Aboriginal Health Human Resource Initiative |
| BC |
British Columbia |
| CCC |
Clinical and Client Care Program |
| CPR |
Cardiopulmonary Resuscitation |
| EKG |
Electrocardiogram |
| FTE |
Full-Time Equivalent |
| FNIHB |
First Nations and Inuit Health Branch |
| FNHA |
First Nations Health Authority |
| ITLS |
International Trauma Life Support |
| INAC |
Indigenous and Northern Affairs Canada |
| NRRS |
Nursing Recruitment and Retention Strategy |
| OT/SB/CB |
Overtime, standby, callback |
| PALS |
Pediatric Advanced Life Support |
| PEMH |
Percy E. Moore Hospital |
| R/I |
Remote and isolated communities |
| RNs |
Registered Nurses |
Executive Summary
This report presents the findings of the Clinical and Client Care (CCC) Program evaluation.
During the period under review, the CCC program was delivered and operated by the First Nations Inuit Health Branch (FNIHB) of Health Canada. FNIHB programming was transferred to the newly created Department of Indigenous Services Canada in 2017 where the CCC program continues to be delivered.
The evaluation was a contracted project conducted on behalf of Health Canada and the Public Health Agency of Canada's Office of Audit and Evaluation. At the time of publishing the report, the project was transferred to the Evaluation, Performance Measurement and Review Branch of Indigenous Services Canada.
Evaluation Purpose and Scope
The purpose of the Clinical and Client Care evaluation was to assess the relevance and performance of the program during the period of April 2012 to March 2017, while also accounting for progress made since the 2015 Office of the Auditor General's assessment of the program.
The scope of the evaluation includes all program activities funded under the CCC program at the national and regional levels, including two federal hospitals in Manitoba. Out of scope are nursing stations in the north where clinical and client care services are provided by territorial governments, and in British Columbia where all responsibilities for federal health programs have been transferred to the First Nations Health Authority (FNHA) through the British Columbia Tripartite Framework Agreement on First Nation Health Governance (2013).
The evaluation was undertaken by the Office of Audit and Evaluation at the Public Health Agency of Canada and has been conducted in accordance with requirements under the Financial Administration Act and the Treasury Board of Canada Policy on Results (2016).
Program Description
The CCC program is designed to provide essential primary care services to First Nations in remote and isolated communities (R/I) with limited or no provincial services readily available during regular operating hours and urgent/ emergent care after hours. Services are delivered by a collaborative health care team, predominantly nurse-led, and include:
- Emergency resuscitation and stabilization, emergency ambulatory care, and out-patient non-urgent services;
- Coordinated and integrated care and referral to appropriate provincial secondary and tertiary levels of care outside the community;
- Scheduled physician and other health professional visits; and,
- Hospital in-patient, ambulatory, and emergency service (Manitoba only).
The services are delivered in 74 nursing stations and five health centers with treatment located across five regions. Health Canada directly delivers services in 52 R/I First Nations communities located in four regions and provides funding through Contribution Agreements to 27 First Nations communities (including 12 in Saskatchewan, one in Alberta, one in Manitoba, four in Ontario, and nine in Quebec) to deliver services. The program is also responsible for two federal hospitals operating in Manitoba (Percy E. Moore Hospital and Norway House Hospital). In recent years (2015-16 - 2016-17), the two sites reported a combined average of approximately 8,400 visits annually, with Percy E. Moore accounting for the vast majority of those visits (7,900).
Evaluation Findings and Conclusions
Relevance
For First Nations living in remote and isolated communities serviced by the CCC program, there are no local alternative options for essential primary, urgent, and emergent health care services. As such, the provision of these services is consistent with the tenets of equal access outlined in the Canada Health Act (1984) and the need to improve Indigenous health outcomes, as articulated by the Indian Health Policy (1979).
The evaluation also found evidence of the program's alignment with overarching roles, responsibilities, and priorities of both the federal government and Health Canada's First Nations and Inuit Health Branch. However, the extent to which the CCC program is responsive to the priorities of the communities it serves is difficult to determine due to the nature of the program (e.g., largely reactive to emerging and urgent needs), limited community engagement in primary care, and little reliable data on utilization of services.
Irrespective of government mandate or priorities, the continued need for CCC programming is evident when considering the significantly poorer health outcomes experienced by First Nations compared to non-First Nations individuals. This is exacerbated by the complexity and high rates of chronic disease, as well as the significant presentation of First Nations individuals living with more than one health condition.
Performance
Overall communities are generally satisfied with the CCC services and hospital care they receive. The program has effectively improved clients' access to, and receipt of, quality care. By exploring interdisciplinary models of care, the program has facilitated greater access to a range of health care professionals, including nurse practitioners. However, challenges still vary across regions related to accessibility of physicians; and progress in hiring more nurse practitioners has not reached all communities. The program's expanded use of interdisciplinary models of care have allowed CCC sites to mitigate challenges raised by the 2015 Office of the Auditor General audit that found nurses were providing care that was beyond their legislated scope of practice.
The main challenges raised by key informants in regards to accessibility of CCC services were often outside the scope of the program (e.g., the condition and capacity of facilities, medical transportation, and road access), thus further highlighting a need to strengthen communication and collaboration across portfolio areas.
Key informants also identified limitations in equipment and diagnostic tools, staffing shortages, and limitations in the effective use of telehealth and other service based technologies as barriers to access.
While cost-effective alternatives/complementary approaches to delivering care have, to a certain extent, been resourced in communities, barriers still exist in fully maximizing their use. Currently, 93 percent of sites with CCC programming are equipped to offer telehealth services. Key informants were clear in saying the technology is available but challenges still exist concerning sufficient bandwidth, connectivity, staff's awareness and comfort level in operating the equipment, and a lack of clarity surrounding remuneration arrangements for physicians providing care through telehealth, which is under provincial/territorial responsibility. Ultimately, making full use of available technology could contribute to further efficiencies and potential cost savings in service delivery, while also providing greater opportunity to offer staff training at a distance.
In terms of ensuring staff are equipped to provide quality care, compliance with mandatory training has markedly improved. Staff completion rates increased from 27 percent in June 2015 to 60 percent in March 2017. However, they vary significantly across regions, affected by factors such as: timing and availability of course instructors; access to nurses to replace nursing staff requiring re-certification; as well as staff turnover. Furthermore, the evaluation found evidence that staff did not always feel properly prepared to work in remote and isolated First Nation communities due to limited awareness of the culture.
Although nurses do not intend to commit to a frontline CCC position for the length of their career, and there is a certain degree of understanding by the program that turnover is a natural state for the profession, there continues to be higher than expected turnover rates for the program. For example, in 2015-16 alone, the program hired 65 nurses, while facing 60 departures in that same year. While staffing turnover/shortages are a reality faced by health care settings in urban, rural, and remote locations, the evaluation recognizes the unique challenges present in R/I First Nation communities. The literature lists some of the following factors impacting recruitment of nurses for remote health care: limited number of nurses willing to relocate to an isolated community, as well as the need for specific personal suitability traits and a greater degree of adaptability to work with challenging cases, as well as limited resources and equipment. In the case of staff turnover, primary contributors identified through the evaluation included: work stress, availability of other job opportunities, the isolated location of the communities, and overall working conditions.
On the whole, since the implementation of the Nursing Recruitment and Retention Strategy in 2012-13, nurse vacancy rates have decreased from 40 percent to 16.2 percent, as of March 2017. While there is still reliance on agency nurses a cumulative cost savings of $18 million has been realized, far exceeding the intended cost savings of $2 million by 2016-17. This reduction in costs has been made possible due to fewer agency nurse hours, but as a result of increased agency rates, continues to be a cost driver irrespective of the fewer shifts filled by temporary staffing agencies. In addition, the program continues to have significant expenditures related to extended hours of operation (overtime, callback, and standby), but has since begun discussions to explore parameters around hours of work in an attempt to establish guidelines that are more consistent with client needs and the structure of nursing station/health centre work.
By providing access to clinical and client care services including urgent and emergent care after hours, the CCC program positively contributes to the health status of First Nation individuals in remote and isolated First Nations communities. However, achieving significant improvements in residents' health outcomes requires a multi-faceted approach where CCC is just one of many programs integrated into a service delivery landscape that captures the broad continuum of community-based programs for First Nations. At this point in time, there continues to be limited integration with provincial health services; as well as communication and collaboration between primary, home care, and other community-based programming such as mental wellness. In effect, the siloed program structure, as well as the multitude of programs and service providers, makes it challenging to ensure an integrated approach to both the planning and delivery of health care services.
Recommendations
The findings from this evaluation have led to the following four recommendations:
- Contribute to greater continuity of care by enhancing data collection, communication and sharing of information across health care providers in different jurisdictions.
To achieve greater integration of services and a stronger continuum of care, the degree of communication and collaboration among federal health programming for First Nations (e.g., Home and Community Care, Mental Wellness), and across health providers in different jurisdictions (including First Nations communities) should be strengthened. Areas for consideration include: enhanced data collection/reliability, and sharing of information to help better inform planning and decision making.
- Make more effective use of technology in the delivery of care and for training purposes.
Telehealth and other technologies available in most communities are currently not being used to their full potential. Action is required to address factors that can constrain the use of technology including connectivity issues (limited bandwidth), a lack of training and technical support, maintenance issues, and limited buy-in from service providers. In addition, there is opportunity to maximize the use of technology in delivering training for frontline CCC staff.
- Strengthen nurse recruitment and retention strategies, including efforts to address conditions that contribute to high rates of turnover amongst nurses.
There is a particular need to address conditions that contribute to nurse turnover. This involves addressing some of the root causes related to issues such as: scope of practice; security and safety; management and operation of nursing stations; and, overtime. Research, including data mining, a labour market analysis, and a survey of existing and former Health Canada nurses would enable the Department to better understand the drivers of turnover such that more effective retention strategies could be developed. - Ensure that formal cultural training is available and completed by all nurses employed in remote and isolated First Nations communities.
In order to provide responsive health services, it is important that CCC staff have a certain degree of cultural understanding. In recognition of the diversity of First Nations communities, it is also important that the training offered be tailored to reflect the diverse communities that each CCC site serves. As it stands, cultural training is provided as part of the orientation for new nurses, but the quality, structure, and consistency with which training is offered often varies. Ensuring that all nurses, both new and longer-term employees, have formal cultural training may positively contribute to the quality of care provided, and ease staff concerns related to their preparedness for providing health services in remote and isolated First Nations communities.
Management Response / Action Plan
Evaluation of the Clinical and Client Care Program—2012-2013 to 2016-2017
| Recommendations | Response | Action Plan | Deliverables | Expected Completion Date |
Accountability | Resources |
|---|---|---|---|---|---|---|
| Recommendation as stated in the evaluation report | Identify whether program management agrees, agrees with conditions, or disagrees with the recommendation, and why | Identify what action(s) program management will take to address the recommendation | Identify key deliverables | Identify timeline for implementation of each deliverable | Identify Senior Management and Executive (Director General and Assistant Deputy Minister level) accountable for the implementation of each deliverable | Describe the human and/or financial resources required to complete recommendation, including the source of resources (additional vs. existing budget) |
| Contribute to greater continuity of care by enhancing data collection, communication and sharing of information across health care providers in different jurisdictions. | Management agrees with the recommendation. With a view to support health services devolution, FNIHB is committed to working with regions and its partners to better coordinate the sharing of information across various health care providers and jurisdictions to facilitate better continuity of care, while respecting privacy legislations on client information. This aligns with the following departmental result: Responsive primary care services are available to First Nations and Inuit. The CCC program will build upon its previous work accomplished in this area taking into consideration the locus of control. |
The CCC program in collaboration with the regions will produce a scan of the various quality improvement processes that are in collaboration with First Nations (e.g., discharge planning, interdisciplinary team meetings that span across the circle of care and trends in digital technology that support the continuity of care) to improve the continuity of care for clients between health care providers and jurisdictions involved in the circle of care. Challenges and opportunities will be identified and recommended next steps will be presented at the First Nations and Inuit Health Branch's Senior Management Committee to inform the Indigenous Services Canada health transformation agenda. The CCC program will also collaborate in utilising business intelligence tools, such as Synergy in Action, to better collect, analyse and report on nursing station information and other data (e.g., progress on accreditation). |
Report on regional engagement and quality improvement activities/ initiatives to improve the continuity of care. | December 2019 | Assistant Deputy Minister, Regional Operations First Nations and Inuit Health Branch Regional Executive Officers Executive Director, Office of Primary Health Care, Population Health and Primary Care Directorate, FNIHB |
No additional resources required |
| Presentation to the Senior Management Committee on initiatives directed towards improving the continuity of care in First Nations communities. | March 2020 | |||||
| Updated Clinical and Client Care Dashboard/ Report Card | March 2019 | |||||
| Make more effective use of technology in the delivery of care and for training purposes. | Management agrees with this recommendation. FNIHB recognizes the importance of using technology in remote and isolated areas and is committed to leverage the use of technologies where possible considering current connectivity/ bandwidth issues and arrangements in place with health care providers. This aligns with the following departmental result: First Nations and Inuit health is supported by modern infrastructure and Indigenous governance. |
The CCC program in collaboration with the regions and academic institutions will assess the delivery mode for providing the onboarding and ongoing training/courses for nurses (e.g., face to face, online, group vs individual); potential expansion on the use of technology for providing training to nurses will be considered. | Scan of the current onboarding and ongoing courses (including delivery mode such as; in-class, face to face or online; group vs individual, videoconferencing, etc.) and its potential expansion to online delivery. | September 2019 | Executive Director, Office of Primary Health Care, Population Health and Primary Care Directorate, FNIHB Regional Executive Officers |
No additional resources required |
| The CCC program is also collaborating with the e-Health Program in order to implement new and effective remote presence health technologies (e.g., Doc in the Box, tele robotics, OTN Hub) that could enhance efficiencies and effectiveness of services in the communities. | The CCC program in collaboration with the eHealth will introduce remote presence technology initiatives in the regions where the infrastructure supports such technology. The duration of these projects will span from one to five years. | Interim Remote Presence Technology Pilot Project Report illustrating the challenges and opportunities of the effectiveness of remote presence technologies in the delivery of care | June 2020 | Executive Director, eHealth, CIAD FNIHB | Funding of $5M /5 years will be allocated to support this project through budget 2017 investments. | |
| Strengthen nurse recruitment and retention strategies, including efforts to address conditions that contribute to high rates of turnover amongst nurses. | Management agrees with this recommendation. The FNIHB Nurse Recruitment and Retention Strategy Steering committee will continue to oversee the development and the implementation of the Nursing Recruitment and Retention Strategy (NRRS) to address specific priorities and persistent issues. This recommendation contributes to the following departmental result: Responsive primary care services are available to First Nations and Inuit The development of comprehensive and ongoing education and clinical practice supports are essential to the overall integration and preparation of newly hired and current FNIHB nurses. |
Conduct a review of the NRRS marketing approach and products (e.g., photos used for advertisement, venues, etc.) will be conducted and changes will be made as appropriate. | Updated FNIHB NRRS marketing approach | March 2019 | Executive Director, Office of Primary Health Care, Population Health and Primary Care Directorate, FNIHB Regional Executive Officers |
Funding of $75K for photo shoot and other social media and print advertisements in 2018-19 Management Operational Plan pending approval. |
| In order to standardize the approach for onboarding at the regional level, a national policy on onboarding will be developed for nurses. | Nurse Onboarding Policy developed and approved | September 2018 | ||||
| To assess current changes in provincial legislation and regulations for nursing practice with a view to refine clinical practice support tools (e.g., registered nurse prescribers, updated list of essential services with point of care testing). This assessment would address the various distinct regional practices where primary care services are provided by FNIHB. | Report on regional nursing regulatory practice changes in order to refine clinical practice support tools | January 2020 | ||||
| To explore initiatives targeted at improving and influencing the pay process, where possible, in order to prevent pay irregularities for nurses. | Report on the development of a regional Pay Support Officer at the program level in Alberta. | January 2019 | ||||
| The FNIHB (CCC program) in collaboration with Professional Institute of the Public service of Canada has developed a memorandum of understanding to address significant safety and security issues in the work place. A work plan, including actions specific to safety and security in remote and isolated locations, such as an Indigenous Service Canada standard on security in remote and isolated work locations, will be developed to address the issues employees are facing regarding safety in the communities. | 2018-19 Workplan to address specific safety and security issues in remote and isolated locations | January 2019 | Funding of $100K to establish the new role. | |||
| The CCC program will also establish a role dedicated to nursing wellness for Northern Ontario and Manitoba to better support a healthy, safe and respectful workplace for nurses. | Wellness role in place to support a healthy, safe and respectful workplace for nurses. | March 2019 | ||||
| Ensure that formal cultural training is available and completed by all nurses employed in remote and isolated First Nations communities. | Management agrees with this recommendation. The Government of Canada is committed to advancing the Truth and Reconciliation Commission of Canada calls to action to provide cultural competency training for health care professionals. This recommendation contributes to the following departmental result: Responsive primary care services are available to First Nations and Inuit |
The CCC program in collaboration with the regions will include cultural competency courses and training as part of the standardized nurse onboarding for all FNIHB employed nurses. Regions to continue to move forward towards the identification of options for staff cultural competency training initiatives specific to the indigenous cultures in their regions. | To include specific cultural competency component to the standardized nurse onboarding policy. | September 2019 | Assistant Deputy Minister, Regional Operations, First Nations and Inuit Health Branch Regional Executive Officers |
|
| FNIHB is developing a cultural curriculum for all employees which will be a foundational element for cultural competency. | Regions to complement the nurse onboarding policy with additional regional training including customized cultural competency training. | National scan of regional adaptation and implementation of cultural competency training | October 2019 | Executive Director, Office of Primary Health Care, Population Health and Primary Care Directorate, FNIHB |
1. Evaluation Purpose
The purpose of the Clinical and Client Care (CCC) evaluation was to assess the relevance and performance of the program during the period of April 2012 to March 2017, while also accounting for progress made since the 2015 Office of the Auditor General's assessment of the program.
The evaluation was required in accordance with Section 42.1 of the Financial Administration Act, which stipulates that every five years departments conduct a review of the relevance and effectiveness of each ongoing program of grants and contributions. The Treasury Board of Canada's Policy on Results (2016) defines such a review as a form of evaluation. The evaluation has been conducted to provide a credible and neutral assessment of the ongoing relevance and performance of the CCC program.
2. Program Description
2.1 Program Context
During the period under review, the CCC program was delivered and operated by the First Nations Inuit Health Branch (FNIHB) of Health Canada. FNIHB programming was transferred to the newly created Department of Indigenous Services Canada in 2017 where the CCC program continues to be delivered.
The CCC program is one of two programs that supported Health Canada's First Nations and Inuit Health Branch's Primary Care sub-program. The program is designed to deliver primary care services to First Nations in remote and isolated communities (R/I) with limited or no provincial services readily available. Funding is administered through contribution agreements and direct departmental spending. The program was developed to meet the primary health care needs of R/I First Nations communities. Remote and isolated communities are defined as "those First Nation communities where transit time to provincial treatment facilities is over four hours by ground transportation. There are four types of R/I communities including Type I (Remote/Isolated Satellite) with no year-round access and intermittent air service; Type II (Isolated) with no year-round road access but regular air service; Type III (Semi-Isolated) communities located one to two hours (or more than 90 km) by road or water from emergency medical services; and Type IV (Non-Isolated Rural/Urban) communities located less than one hour (or less than 90 km) from emergency medical services."Footnote 1
2.2 Program Profile
CCC programming is designed to provide essential services during regular operating hours and urgent/emergent care after hours, seven days per weekFootnote 2. The services, which are delivered by a predominantly nurse-led, collaborative health care team, include:
- Emergency resuscitation, stabilization, and ambulatory care (referred to as emergent care); and out-patient non-urgent services;
- Coordinated and integrated care and referral to appropriate provincial secondary and tertiary levels of care outside the community;
- Scheduled physician and other health professional visits; and,
- Hospital in-patient, ambulatory, and emergency services (Manitoba only).
CCC services are delivered in 74 nursing stations and five health centers with treatment, located across five regions. The CCC health services are directly delivered by Health Canada in 52 R/I First Nations communities located in Alberta, Manitoba, Ontario and Quebec. Health Canada also provides funding to 27 First Nations communities (including 12 in Saskatchewan, one in Alberta, one in Manitoba, four in Ontario, and nine in Quebec) to deliver these services.
| Regions | Alberta | Saskatchewan | Manitoba | Ontario | Quebec | Total |
|---|---|---|---|---|---|---|
| Nursing Stations | 4 | 12 | 22 | 25 | 11 | 74 |
| Health Centers with treatment | 1 | 4 | 5 |
| Regions | Alberta | Saskatchewan | Manitoba | Ontario | Quebec | Total |
|---|---|---|---|---|---|---|
| Health Canada Managed | 4 | - | 21 | 25 | 2 | 52 |
| First Nations Managed | 1 | 12 | 1 | 4 | 9 | 27 |
| Total All | 5 | 12 | 22 | 29 | 11 | 79 |
Note: Does not include federal hospitals (two) in Manitoba |
||||||
In addition, Health Canada is responsible for two federal hospitals located in Manitoba:
- Norway House Hospital is situated at the northern tip of Lake Winnipeg and linked to Winnipeg year-round by daily flights and an all-weather road. The hospital has seven in-patient beds and underwent renovations in 2011, which included the upgrade of 12 examination rooms, treatment and triage rooms. The hospital has a laboratory, x-ray, on-site pharmacist, and social services.
- Percy E. Moore Hospital (PEMH) is located 192 kilometres north of Winnipeg and easily accessible by highway. The hospital is a 16-bed, four-bassinet facility and has resident physicians, a full-time pharmacist, and social workers providing health-care services.
Service Providers
The CCC services are provided by qualified health care professionals who must have the necessary competencies and meet the regulatory and legislative requirements of the provinces in which they practice. They are assisted by unregulated health workers such as health care aides and community health representatives, rehabilitation aides, laboratory and X-ray technicians, pharmacy technicians and support personnel such as health receptionists. Nurses play a central role in the delivery of health services in R/I First Nation communities. In most R/I communities, essential treatment services are provided by nursing staff, including registered nurses, registered psychiatric nurses, and nurse practitioners, licensed or registered practical nurses supported by off-site medical practitioners and/or nurse practitioners. For residents in most of these communities, the CCC program is often the first point of contact with the healthcare system. In nursing stations or health centers with treatment, registered nurses consult, often at a distance, with other health care providers and services, including physicians, to provide a broad range of essential services. Telehealth is another service used to enhance access to additional services as required.
Governance
The CCC program is governed by FNIHB 's national office and regional offices, which are responsible for oversight of all FNIHB programs, including the CCC. The Senior Management Committee includes representation from FNIHB national and regional senior management, the Assembly of First Nations and Inuit Tapiriit Kanatami. The Committee discusses and determines objectives, plans and priorities, and informs operational and financial plans.
The FNIHB national office is responsible for policy development and program planning, including national program framework design, national project reporting and branch-level special studies, provision of advice and/or guidance on program delivery, and working with First Nations and Inuit partnersFootnote 3 to ensure effective program delivery.
Regional offices collaborate with Indigenous communities and organizations as well as Health Canada senior management to determine and review regional priorities in the context of national priorities and establish strategies to address regional needs. Regional offices play a lead role in the management of contribution agreements, which involves regional program performance monitoring, reporting, information roll-up, supporting communities with program delivery and working with First Nations partners at regional and local levels.
2.3 Program Narrative
The primary objective of the CCC program is to provide access to clinical and client care services in R/I First Nations communities. In the logic model (2016) contained in Appendix 1, Program Activities are grouped under three categories: workforce recruitment, retention and capacity building activities; provision of clinical and client care services; and evidence-based research activities, and collection and assessment of service delivery information. Program outputs include: health human resources; training; emergent, urgent and non-urgent visits; and quality improvement processes and tools. The immediate outcomes, which are directly attributable to CCC outputs, include:
- First Nations individuals, families and communities have access to CCC Services, enabling needs to be addressed in the R/I communities. By making programming available locally, barriers to accessibility (e.g., transportation) are reduced and individuals can benefit from the services offered.
- A trained nursing workforce is in place to provide CCC services. Health Canada hires health care providers with the required education and experience and provides mandatory training to ensure nurses have the skills and abilities needed to work within the demanding clinical and client care environment of R/I communities.
- Quality CCC services are delivered. Clinical practice guidelines, processes, training and tools are developed to improve the quality of services provided to CCC clients and their families.
The CCC program's immediate outcomes contribute to achievement of intermediate and ultimate outcomes. For example, the provision of culturally relevant training, continuing education, and professional development contributes to a trained CCC workforce, which in turn contributes to the sustainability of the program and its ability to contribute to the health status of First Nations living in R/I communities in the long term. All outcomes are related to the Branch Strategic Outcome, which states that First Nations and Inuit communities and individuals receive health services that are responsive to their needs so as to improve their health status.
2.4 Program Alignment and Resources
The CCC fell under Health Canada's Sub-Program 3.1.3 First Nations and Inuit Primary Care, from which it receives transfer payment funding. Actual expenditures of the program in 2016-17 totalled $187 million, of which 37 percent was allocated through contribution agreements. The remaining 63 percent was expended directly by Health Canada for service delivery. The following table outlines the actual program expenditures over the period from 2012-13 to 2016-17.
| Expenditures | 2012-13 | 2013-14 | 2014-15 | 2015-16 | 2016-17 | Total | % |
|---|---|---|---|---|---|---|---|
| Salaries | $49.9 | $53.2 | $69.1 | $68.2 | $67.4 | $307.9 | 36% |
| Operations and Maintenance | $46.3 | $48.1 | $46.9 | $52.1 | $58.2 | $251.6 | 30% |
| Contributions | $55.1 | $58.9 | $68.0 | $64.9 | $65.2 | $312.0 | 37% |
| Revenue/Other | -$3.8 | -$3.3 | -$3.4 | -$3.7 | -3.6 | -17.8 | -2% |
| Total: Clinical and Client Care | $147.5 | $156.9 | $180.6 | $181.5 | $187.3 | $853.7 | 100% |
Source: Financial data provided by the Chief Financial Officer Branch, Health Canada |
|||||||
3. Evaluation Description
3.1 Evaluation Scope, Approach and Design
The evaluation was a contracted project conducted on behalf of Health Canada and the Public Health Agency of Canada's Office of Audit and Evaluation. At the time of publishing the report, the project was transferred to the Evaluation, Performance Measurement and Review Branch of Indigenous Services Canada.
The period covered by the evaluation includes activities from April 2012 to March 2017. The scope of the evaluation includes all program activities funded under the CCC program at the national and regional levels. Out of scope are nursing stations in the northern region provided by the territorial governments and the pacific region. In British Columbia, all responsibilities for federal health programs have been transferred to the First Nations Health Authority (FNHA) through the British Columbia Tripartite Framework Agreement on First Nation Health Governance, signed in 2011. The British Columbia (BC) FNHA services were reviewed as part of the case studies to identify best practices and alternative delivery models that could be adapted by Health Canada.
The Treasury Board's Policy on Results (2016) guided the evaluation design and data collection methods such that the evaluation would meet the objectives and requirements of the policy. A non-experimental design was used. As this program focuses on First Nations communities, the Assembly of First Nations was consulted during the development of the scoping deck and evaluation methodology, and provided with an opportunity to review and comment on the evaluation instruments, the preliminary findings, and the evaluation report. For more detailed methodology, see Appendix 2.
The evaluation employed multiple lines of evidence, including:
- A document, file and data review consisting of internal documents, programs evaluations, program reports, regional reports and inventories, and financial data;
- A literature review focused on peer-reviewed literature related to best practices in delivery of services in remote and isolated communities;
- Surveys with 118 health professionals across five regions;
- Interviews with 46 key informants, including FNIHB national and regional program staff, other Health Canada program representatives, provincial governments, regional health authorities, health associations, and other stakeholders (out of 13 health directors, seven were from transferred communities);
- Six community case studies involving visits to five communities and a federal hospital in Manitoba. Including the hospital, a total of 73 interviews were conducted, of which 33 representatives were from two communities where health services were managed by the First Nation, 25 representatives were from three communities with health services managed by Health Canada, and 15 representatives from the hospital. The evaluators toured the facilities and reviewed available health plans and other documents; and
- A comparative analysis case study focused on the BC FNHA to identify best practices. The case study involved a review of publicly available documents on the design and delivery of the CCC program in British Columbia, as well as interviews with six representatives of BC FNHA and one representative of British Columbia Ministry of Health.
In total, at least 57 representatives from First Nations managed sites participated in the evaluation via key informant interviews (seven), surveys (17) and case studies, which included interviews (33). The use of multiple lines of evidence and triangulation increases the reliability and validity of the evaluation findings and conclusions. The quantifiers used to report findings from key informant interviews are as follows:
- Most means over 80 percent of those responding to the question;
- Majority means between 50 percent and 80 percent of those responding to the question;
- Some means between 25 percent and 50 percent of those responding to the question; and,
- A few means less than 25 percent of those responding to the questions or two to four respondents.
3.2 Limitations and Mitigation Strategies
Most evaluations face constraints that may have implications for the validity and reliability of evaluation findings and conclusions. Table 3 outlines the limitations encountered during implementation of the methods selected for this evaluation. Also noted are the mitigation strategies put in place to ensure that the evaluation findings can be used with confidence to guide program planning and decision making.
| Limitation | Impact | Mitigation Strategy |
|---|---|---|
| Some data on program outputs and outcomes has only been collected since 2015. | Limited analysis for some outcomes with respect to the progress made. | Other proxy indicators were used to comment on the progress made such as perceptions of key informants, and health professionals. |
| Variations across the regions/communities in program delivery. | Limitations in applying evaluation findings to all regions/communities. | The evaluation emphasizes areas where differences across regions or communities were found. Case studies highlight such differences. |
| Limited availability of data from First Nations operated sites (transferred communities). | Challenges in conducting a comparative analysis of delivery of services in Health Canada and First Nation managed sites. | Analyses are based on primary data collected through interviews with nearly 40 health professionals and managers working in transferred communities, and interviews with 11 community members. |
| Key informants had varying levels of knowledge of the services. They responded selectively to the questions related to their area of expertise or knowledge. | The number of key informants responding varies across questions. | Qualitative analysis of interview data was conducted for each question/topic according to key informants' role and knowledge of a particular area. |
| Detailed financial data was not available for different program components by region. Discrepancies in costs reporting. | Unable to provide more detailed analysis of efficiency and economy of the program and effectiveness of cost reduction strategies. | Higher level analyses were done related to costs associated with Health Canada vs. agency nurses. |
4. Findings
4.1 Relevance: Issue #1 – Continued Need for the Program
There is a continued need for clinical and client care services in R/I First Nations communities, which is projected to increase given the population growth, an aging demographic, continuing disparities in health outcomes, the complexity and co-morbidity of disease, and the increasing need to provide care related to chronic disease management, mental health and specialized care.
The First Nations Regional Health Survey (2008-10) reported that First Nations in Canada experience higher rates of chronic health conditions and multiple conditions than non-First Nations, including diabetes, high blood pressure, stomach and intestinal problems, and high levels of psychological distress. About two-thirds (63 percent) of First Nations adults indicated having at least one chronic health condition, with just under 40 percent reporting having two or more conditions. In comparison, one in five Canadian adults lives with one of the following chronic diseases: cardiovascular disease, cancer, chronic respiratory diseases, or diabetes, according to a recent study by Health Canada on prevalence of chronic diseases among CanadiansFootnote 4. Furthermore, 51 percent of all First Nations adults (with a greater proportion of females than males) report either moderate or high levels of psychological distress, as compared to 34 percent of the general Canadian population.
The need is projected to increase. According to newly released data by Statistics Canada on 2016 Census Data, the First Nations population grew by 39.3 percent from 2006. This is about four times the growth rate of the non-Indigenous population over the same periodFootnote 5. Close to half (44.2 percent) of First Nations people with registered or treaty Indian status, lived on-reserve in 2016, registering a growth of 12.8 percent for on-reserve population. Although the First Nations population is young, many First Nations communities have a growing aging population, which will further increase demand for services. According to Statistics Canada (2017) projections, populations 65 years of age and older could more than double by 2036.Footnote 6
The CCC services complement other health programs delivered in remote and isolated First Nations communities, although limited collaboration and information sharing across programs in some communities has resulted in gaps and areas of overlap.
The CCC program is the only source of primary clinical care services in the R/I communities. It is also a front-line service, on the continuum of careFootnote 7, that is highly dependent on number of other federal, provincial and community health support programs. For example, the program works closely with provincial services such as those responsible for medical air evacuation and provincial hospital programs. With respect to Health Canada services, the program is closely linked with the Home and Community Care Program, e-Health Infrastructure Program and the Non-Insured Health Benefits Program, which provide support for related services such as medical transportation, emergency services and other specialized services.
The program is largely perceived as complementing other programs available in the communities in providing continuity of care. However, some key informants, involved in the management and delivery of the CCC program (health directors and FNIHB regions), noted difficulties with respect to coordinating services across various programs given the number of health programs, delivery organizations and employers involved, and limited communication and collaboration (e.g., siloed program structures). Case studies identified that a lack of coordination and information sharing between the CCC and Home and Community Care Program in some communities has created gaps and duplication of services in areas such as chronic disease management, prenatal services, and healthy living. For example, nurses in one community visited reported that they have no way of knowing what information has been given to their patients or whether, in fact, the patients have been visited by a home care worker.
4.2 Relevance: Issue #2 – Alignment with Government and First Nation Priorities
The Government of Canada has demonstrated the priority it places on the delivery of clinical and client care in the communities by making significant additional investments to stabilize operations, enhance models of care, and support the construction, renovation and repair of nursing stations and residences.
Since the last evaluation, the federal government has increased the financial allocation to the program, confirming its on-going commitment to improving health care and health outcomes of First Nations in Canada. Budget 2013 included $211 million in supplemental funding over five years to stabilize the CCC program and ensure that essential primary services are available in First Nation communities to address immediate health needs. The budget in 2014-15 outlined initiatives to further enhance models of primary health care with the goal of re-orienting current practices to support modern, sustainable, high-quality health care in R/I First Nations communities. Budget 2016 included a significant investment in health infrastructure through the Health Care Facilities Program; $270 million over five years will be used, in part, to support the construction, renovation and repair of nursing stations, residences for health care workers, and health offices that provide health services on-reserve. The Health Canada departmental plan (2017-18) reports that improving health services and developing innovative partnerships to close the Indigenous health gap remains a top priority for Canada. Budget 2017 proposes to invest $828.2 million over five years to improve the health outcomes of First Nations and Inuit, of which $72.1 million has been allocated to Primary Care.
The program aligns directly with broad strategic priorities identified in collaboration with First Nations. The extent to which the program is well aligned with local First Nations' priorities varies across communities, and is related to factors such as level of community engagement, ability to proactively identify issues, and flexibility of resources.
The First Nations and Inuit Health Branch Strategic Plan: A Shared Path to Improved Health (2012) outlined health priorities identified in collaboration with First Nations representatives, other governments and Health Canada. The intended outcomes of the CCC program align directly with the goal of providing high quality health services across the continuum of care for individuals, families and communities.
Over one-half of the key informants working with the communities with Health Canada- managed CCC services, agreed that the program is aligned with the priorities of First Nations communities. Key informants highlighted Health Canada's efforts to identify priorities and structure services accordingly, in collaboration with First Nations communities (e.g., the development of health care planning guides and toolkits to facilitate planning). Nearly one third of key informants indicated a lack of alignment with local priorities, and listed the following barriers: difficulties in engaging the community in a meaningful way and limited flexibility with respect to allocating resources in response to emerging issues and priorities. They also noted that the immediate pressures of having to address emergency and clinical care needs often result in other priorities being overlooked, such as chronic care management or mental health care. FNIHB representatives noted that planning is challenging given the nature of urgent and emergent health services (i.e., the program is designed to respond to immediate needs), but added that delivery of services could still be better aligned with the local community needs (e.g., by adjusting hours of operation, allowing for greater flexibility in the allocation of resources and models of care, etc.)
Key informant data indicates that staff perceive better alignment with local First Nations priorities in First Nations- managed CCC sites. Nearly all representatives working in First Nations managed CCC sites, compared to approximately half of staff surveyed in Health Canada managed sites agreed that the program is aligned with the local priorities of First Nations communities. Some transferred communities tend to be more effective in engaging the community. Health directors from transferred communities reported using meetings, surveys and other ongoing engagement to
identify priorities or concerns, which were then communicated to health boards or health managers who then work together towards addressing the issues raised. For example, under their funding agreements, transferred communities can have greater flexibility to quickly and effectively respond to the emerging priorities (e.g., by hiring a mental health nurse).
4.3 Relevance: Issue #3 – Alignment with Federal Roles and Responsibilities
The program is aligned with federal government and departmental roles and responsibilities.
The federal government shares responsibility for improving the health of Indigenous people with provincial and territorial partners and Indigenous organizations. Federal government funding for CCC services is aligned with provisions found in the Canada Health Act (1984), the Indian Health Policy (1979), and other Health Canada policies. The 1979 Indian Health Policy recognizes the special relationship between the federal government and Indigenous people, the interrelated nature of health system, and the role of the federal government in "providing public health activities on reserves, health promotion and detection and mitigation of hazards to health in the environment"Footnote 8.
The CCC policies and practices are generally aligned with provincial health legislation and regulations. FNIHB has taken steps to ensure that nurses are working within their scope of practice in each jurisdiction; however, concerns remain in some communities.
Provincial legislation governs nursing practice in each region. Over half of key informants involved in the delivery of the CCC (e.g., regional FNIHB representatives, health directors and nurse managers) reported that CCC policies and practices are consistent with provincial legislation (e.g., legislation regarding maintenance and inspection of diagnostic tools, laboratory licenses, transportation of dangerous goods, etc.).
Nursing scope of practice is regulated by the provincial regulatory bodies. Significant concerns about nurses working outside of their regulated scope were raised in the previous CCC Evaluation (2013) and Auditor General Report (2015). Two-thirds of key informants noted that necessary steps were taken to address these concerns, through actions such as introducing interdisciplinary teams, increasing access to nurse practitionersFootnote 9, and adding full-time paramedics or full-time physicians (in transferred communities) to broaden the skill sets within the health teams working at the nursing stations. In Saskatchewan, the Additional Authorized Practice certification allows Registered Nurses (RNs) to practice with an expanded scope (e.g., RNs can prescribe and dispense certain controlled drugs and substances, order tests, prescribe vaccines, and perform minor procedures).
Although progress has been made, there are still some concerns related to ensuring that nurses practice within their regulated scope. About one-third of key informants, provincial and regional FNIHB representatives noted that nurses may still work outside their scope of practice in areas where access to other health professionals is limited. When asked about the major factors that contribute to a high rate of nurse turnover in their communities, 28 percent of the nurses surveyed identified concerns about the scope of practice.
4.4 Performance: Issue #4 – Achievement of Expected Outcomes (Effectiveness)
4.4.1 To what extent have the immediate outcomes been achieved?
Immediate Outcome #1: First Nations individuals, families and communities have access to Clinical and Client Care Services (including federal hospitals).
Through nursing stations and hospitals, the CCC provides all R/I communities with access to essential clinical and client care services during regular weekday hours as well as access to urgent services after hours. Nearly 70,500 residents in communities with Health Canada- managed services made approximately 370,000 CCC visits in 2015-16 (over a third of which were made after hours) while approximately 8,400 visits were made to the two federal hospitals in Manitoba. In 19 First Nations-managed communities that reported data in 2014-15Footnote 10, close to 130,000 urgent and non-urgent visits were made.
Most health professionals surveyed agreed that First Nations individuals, families and communities have access to the clinical and client care they need in the communities. According to nursing inventories conducted in 2016, all R/I communities have access to essential clinical and client care during regular weekday hours (8:30 to 17:00 Monday to Friday), and urgent services after hours delivered by health care professionals on-call. The regular hours of operation may vary slightly across the nursing stations. Some stations close occasionally, providing emergency only services during staff rotation or on days when they are short staffed.
Of the 368,374 visits reported to Health Canada-managed CCC services in nursing stations and health centres with treatment across the four regions in 2015-16Footnote 11, 63 percent were made during regular hours and 37 percent occurred after-hours. While after-hour services are provided to ensure that R/I communities have access to urgent care, program utilization data indicates that only 15 percent of after hour visits were urgent (urgency of after-hour services varied across the regions, from 95 percent in Alberta to 33 percent in Ontario and 10 percent in both Quebec and ManitobaFootnote 12).
According to data from approximately 19 communities with First Nations-managed CCC services, the severity of cases seen in 2013-14 compared to 2014-15 has decreased. In 2013-14, one-third of the 156,000 visits accessed urgent care services, compared to less than one-fifth of the 130,000 visits in 2014-15 qualifying as urgent care.Footnote 13
Visitation data for the two federal hospitals indicate that there were about 7,900 visits annually to the PEMH over the past two years (2015-16 and 2016-17), while the Norway House Hospital has admitted an average of approximately 500 patients annually providing for an occupancy rate of about 50 percentFootnote 14. Non-urgent care accounts for over 60 percent of the visits to PEMH, with the demand attributed, by hospital representatives, largely to a lack of physicians in surrounding health clinics and rural hospitals (e.g., diversion from surrounding communities, clients prefer to access a physician at the hospital due to waiting times at the clinic). According to the hospital representatives, wait times at the hospitals vary depending on the level of acuity of conditions patients are presenting with, which are currently considered to be reasonable. In a survey, conducted by PEMH in February 2017, 42 percent of 49 emergency room patients indicated that their condition was always or usually addressed by a physician within one hour of their presentation to the Emergency Room, 34 percent said sometimes, and 16 percent said never. The average wait time for the Norway House Hospital from arrival at the Emergency Department to admission was 3.3 hours in 2015-16, which is skewed by the large numbers of non-urgent cases. A study of Emergency Room wait times in Winnipeg hospitals shows that emergency department wait times for a small number of patients (10 percent of non-urgent visits) are long (at least 4.7 hours), while the more urgent cases, experience wait times of approximately 42 minutes.Footnote 15
Key informants argued that R/I First Nations communities require greater access to clinical and client services than other similarly located communities because of the unique challenges they face.At the present time, access to RNs in some First Nations communities is higher than similar provincially-served communities, while access to timely physician and specialized care, particularly mental health professionals, varies across, and is limited in most communities.
In response to questions about whether R/I First Nations communities have access to services comparable to those in other similar communities, most key informants argued that there are no other similar communities. Communities served by the CCC program are unique in their challenges, particularly with respect to the degree of geographic isolation and accompanying transportation issues (65 percent of health professionals surveyed identified transportation issues as constraining access to services)Footnote 16, the model of care (nurse vs. physician-driven), access to diagnostic tools (e.g., point of care), the involvement of multiple levels of government in the delivery of services (e.g., the federal government, provincial government, and the band), the social determinants of health, infrastructure, and historical circumstances. Some key informants argued that any efforts to assess comparability should focus on equality of outcomes rather than achieving comparability of resources with the provincial systems. Given differences in the challenges faced by R/I First Nations communities, it was argued that equality of resources will not result in equality of outcomes.
A comparability of access study conducted by Health Canada using a sample of three communities meeting similar criteria, across three regions, concluded that access to services in First Nations remote communities was comparable, on most measures, to those provided in provincial rural communities. The study found that the nurse-to-population rate was generally higher in Health Canada facilities. However, the physician-to-population rate and visiting physician hours were lower in First Nations communities.Footnote 17 Access to physicians varies depending on the needs and remoteness of the communities, and is negotiated with provincial partners. Most health professionals surveyed as part of the evaluation identified long waiting times to access other health professionals or specialists (82 percent) or physicians (65 percent) as factors constraining access to care in the communities. In one of the communities assessed as part of the Quality Improvement Onsite Assessment, there was a two-month wait time to see a physician in the community. Nearly all community members and health professionals, interviewed as part of case studies, expressed concerns regarding access to physicians and other health specialists, particularly mental health professionals. Most key informants, including nearly all health directors interviewed, emphasized the challenges with respect to accessing mental health professionals and provincial mental health services, including difficulties scheduling appointments. Similar concerns were noted in regional 'Key Issues and Deficiency' documents (2016), which highlight challenges in accessing the resources needed to address acute mental health care issues (e.g., grief, acute anxiety, domestic violence, suicidal ideation with no plan, substance abuse).
While the Health Canada comparability of access study found that the nurse-to-population rate was higher in the communities where CCC programming is offered, the majority of key informants indicated that there is still a nursing shortage given the strong demand for services. Close to two-thirds of the health professionals surveyed identified nursing shortages as a major factor constraining access to services. This was particularly highlighted by health professionals from Ontario, where about 80 percent of respondents reported nursing shortages. A few health directors noted that access to the CCC services is not equal in all communities, indicating significant differences with respect to workloads and access to provincial care.
Immediate Outcome #2: A trained nursing workforce is in place to provide CCC services.
Measures taken by Health Canada have improved compliance with mandatory training for nurses. Barriers to achieving higher and more consistent compliance with mandatory training include: the rate of nurse turnover, availability of nurses to backfill for those requiring re-certification, costs of travel, training and replacements, and accessibility of the training courses.
Health Canada has taken multiple steps over the past few years to set out the guidelines and improve training compliance among Health Canada employed nurses. The updated national policy on Mandatory Training (revised 2015) outlines the roles and responsibilities for Health Canada employed nurses in obtaining and maintaining certifications in the following five mandatory courses: Advanced Cardiac Life Support (ACLS), International Trauma Life Support (ITLS), Pediatric Advanced Life Support (PALS), Controlled Substances, and Immunization. Recertification is required every two (PALS, ACLS) to three years for mandatory training courses.
Most key informants noted that the national training policy (which includes responsibilities for monitoring compliance, and increased resources) has helped to improve compliance rates. As of March 2017, 60 percent of the 337 Health Canada nurses, across four regions, were fully compliant across all of the mandatory training. This is up from 46 percent in March 2016 and 27 percent in June 2015. Differences in the level of compliance across regions and type of training are indicated in Table 4. To achieve full compliance, regions must ensure that nurses have up-to-date certification in all five mandatory training courses. As illustrated in the following table, failing to meet requirements in one course (as was recently the case for PALS recertification in Quebec), would result in none of the nurses being in full compliance with the mandatory training. Consequently, this criteria negatively impacts overall compliance rates.
| Region | ACLS | ITLS | PALS | Controlled Substances |
Immunization | Full Compliance |
|---|---|---|---|---|---|---|
| Alberta (30 Nurses) |
80% (24/30) |
80% (24/30) |
73% (22/30) |
80% (24/30) |
83% (25/30) |
53% (16/30) |
| Manitoba (174 Nurses) |
80% (139/174) |
75% (130/174) |
79% (138/174) |
74% (129/174) |
80% (139/174) |
43% (75/174) |
| Ontario (125 Nurses) |
94% (118/125) |
92% (115/125) |
90% (112/125) |
97% (121/125) |
95% (119/125) |
90% (112/125) |
| Quebec (8 Nurses) |
50% (4/8) |
38% (3/8) |
0% (0/8) |
63% (5/8) |
50% (4/8) |
0% (0/8) |
| Total (n=337) | 85% | 81% | 81% | 83% | 85% | 60% |
According to the document review and key informants, fluctuations in mandatory training compliance over time and across regions is a function of turnover (e.g., new nurses must obtain the mandatory certifications) and the availability of relief nurses to cover for existing nurses requiring recertification. At least three mandatory training courses (ACLS, ITLS, PALS) are delivered in the classroom, which requires nurses to travel out of the community and relief staff to be scheduled to provide replacement. The program estimates that a maximum of 40 hours per year is required for training for both full-time and part-time nurses. To put that in perspective, at this level and based on the number of Health Canada nurses employed as of March 31, 2017 (n=337), approximately 1,800 days each year would have to be filled by relief nurses to achieve 100 percent compliance.
Most regional FNIHB representatives, as well as some health directors, noted that insufficient resources are available to cover the costs of replacement, training and travel expenses. Accessibility of the mandatory training courses can also be challenging. About half of surveyed health professionals noted that the training is difficult to access. Depending on the region, the courses may be offered only once a month, on weekends, or when enough nurses have signed up for the course to be scheduled. Nurses strongly prefer not to be taking training during their scheduled time off. Some frustrations were expressed by Health Canada nurses during community visits regarding having to search for, schedule and pay for the training themselves, with some reporting that they received reimbursement only months after it had been completed.
To address some of these issues and reduce reliance on traveling for training, about half of key informants suggested that Health Canada should work more closely with the academic and other institutions to implement a combination of the following: make some parts of the mandatory training available online, increase the use of telehealth for trainingFootnote 18, and provide on-site instruction for aspects of training that require hands on experience. In British Columbia, FNHA representatives highlighted e-Health initiatives as a promising practice to deliver training. These initiatives have provided two-way live video conferencing support for clinical and health-related education to about 150 First Nations communities across British Columbia.
An onboarding and orientation process for new nurses is in place. However, it is unevenly implemented.
In addition to national mandatory training, each region provides a number of essential training activities for nurses, which are in line with the provincial requirements, such as Cardiopulmonary Resuscitation (CPR), Transportation of Dangerous Goods, Nurse Safety Awareness Training, Workplace Hazardous Materials Information System, and other relevant skills development training. The regions are also responsible for providing orientation to new nurses. To deliver training, regions use various strategies such as telehealth, train-the-trainer for immunization courses or CPR, and having paramedics provide training on-site.
A few key informants noted that the National Onboarding Checklist (2017) was developed to standardize the onboarding process, provide information about various roles, responsibilities, and the clients, and offer links to additional resources. As part of the onboarding process, during their first few weeks, new nurses receive orientation and mentoring at the regional office and in the community. Over half of nurses surveyed agreed that new nurses are provided with the orientation and mentoring support they need. However, close to a third disagreed that the orientation was adequate. The case studies indicate that there can be significant differences across communities in terms of the quality and duration of the orientation as well as the emphasis placed on mentoring. For example, one of the visited communities offered a well-structured on-site orientation for the first two weeks, delivered by a nurse practitioner. The orientation included an overview of the nursing station policies, organizational structure and management structure as well as an introduction to the community in terms of culture, language and political structure. In other communities, there was less emphasis placed on formal orientation ("nurses learn by doing"), particularly where there has been turnover at the management level (e.g., nurse manager or nurse-in-charge). Most health directors noted that there is a need for more comprehensive onboarding, orientation and mentoring process for new employees to adequately prepare them for remote practice environment (e.g., longer orientation with more hands-on training with remote practice skills and environment, standardization of process, understanding of 'how things work').
Gaps were identified related to various elements of the mandatory training courses and formal cultural sensitivity training.
In R/I First Nations communities, nurses face emergency situations that require training beyond what basic nursing education programs provide. The Department specifies mandatory training for these nurses to complete, including courses in areas such as immunization, cardiac life support, and the handling of controlled substances in First Nations health facilities. Specified mandatory and essential training requirements, along with the clinical practice guidelines, aim to prepare the nurse to work in this challenging environment, and enable them to practice to the full extent of their education, training, and competencies, and foster inter-professional collaboration.
The most common challenge related to training, reported by 54 percent of health professionals, is that training does not reflect the full range of competencies needed to work in R/I First Nations communities. Various gaps and issues were identified in the health professionals survey, case studies, and document review, which can be divided into three categories:
- The limited relevance of some parts of training courses to providing essential health services in R/I communities. For example, ACLS/PALS training includes topics that are based on having access to a physician when the situation requires interventions outside the nurses' legislated scope of practice, and the ITLS training is viewed to be targeted towards paramedics rather than nurses. Over 10 percent of nurses surveyed reported that the training they received is not fully aligned with community needs, such as mental health and addiction-related training, prenatal counselling, nutrition, chronic disease management, case management, and the over-prescribing of antibiotics. CCC internal program documents (2016) highlighted that nurses are not well trained in Canadian Triage and Acuity Scale as the standard classification for triaging patients.
- Limited access to management training on operational, management and human resources issues for nurses-in-charge or nurse managers (highlighted in the case studies as a gap by the nurses-in-charge). Given the workload and other training requirements, such training to the extent that it is available, is not a priority for nurses in management positions. Over half of health professionals surveyed identified a lack of time as a barrier to accessing needed training.
- Lack of training related to information collection, data management and use of technology. For example, all nurse managers spoke about the importance of systematic and consistent information records in patient charts for effective case management. The level of technology utilization (e.g., telehealth equipment) is dependent upon the skills of the staff and can be impacted by turnover, highlighting the need for ongoing technical training.Footnote 19
The need for more formal cultural sensitivity training was identified by most key informants including about half of health directors, and nearly all health staff participating in interviews as part of the case studies. A few regional FNIHB representatives called it the most significant gap in training. About half of nurses interviewed, most of whom had been employed by Health Canada for less than two years, noted that, when hired, they received some cultural sensitivity training; however, the overall volume of material covered as part of their orientation makes it hard for them to retain that part of the training.
The review of practices in British Columbia shows that FNHA implements a formal mentorship program for new nurses, including a cultural safety component. The regional FNHA representatives interviewed emphasized their commitment to cultural training for all health providers, and other initiatives that integrate culturally safe practices in health service to meet the needs of First Nations. To improve delivery of cultural training, the FNHA has established mandatory cultural competency training for all FNHA employees (online module); integrated First Nations cultural safety and humility within health services by signing the first-ever Cultural Safety and Humility Declaration between British Columbia's health authorities and the Deputy Minister of Health for each regional health authority in British Columbia; developed and delivers a webinar series on cultural sensitivity and humility (delivered by the Chief Executive Officer); and created an evaluation framework to measuring the impact of cultural safety and humility interventionsFootnote 20.
Immediate Outcome #3: Quality Clinical and Client Care services are delivered (includes hospitals)Footnote 21
Quality of care is a function of a variety of factors, including the presence and use of relevant policies and standards, the stability of the workforce and diagnostic capabilities. Relevant policies and standards are in place and used regularly, contributing to the quality of care. However, some gaps in policies and issues were identified with respect to staff turnover and diagnostic services.
Most program representatives (FNIHB and health directors) noted that relevant standards and policies are in place to ensure that the health services are of high quality. The policies are most commonly developed by the national office and then adjusted by regions to ensure alignment with provincial standards. Policies and tools that have been created and updated to ensure high-quality services include a National Education Policy, FNIHB Health Facilities Safety and Security Policy updates (March 2016), Infrastructure-Related Health and Safety Risks, and Patient Safety Incident Management. Key informants also reported that new quality improvement processes and tools have been developed to ensure quality services, such as the 'Essential Service templates' which are used as a tool for ensuring the minimum resources required by nursing stations are in place. In September 2016, FNIHB piloted a quality improvement on-site assessment process in two R/I nursing stations to inform the nurse-in-charge and nurse managers of gaps so that they can develop a plan to address the issues.
Most nurses strongly or somewhat agreed that nurses make good use of relevant policies and standards in their practice. The Clinical Practice Guidelines were identified as the most commonly used policy document (91 percent of health professionals surveyed reported using it daily). Other policies commonly used by health professionals surveyed include: Nursing Station Formulary and Drug Classification System (75 percent use it on regular basis); FNIHB Policy and Procedures on Controlled Substances (58 percent); and to, a lesser extent, the Diabetes Canada Practice Guidelines (39 percent). In addition, nurses reported frequently using anti-infective guidelines, hypertension guidelines, public health and immunization documents, and various specialized guidelines (e.g., cervical screening, pediatric guidelines, etc.).
Some gaps in policies were identified, of which the most common were gaps and outdated standards in the Clinical Practice Guidelines (identified by 71 percent of nurses) in areas such as mental health, Sexually Transmitted Blood Borne Infections, Human Immunodeficiency Virus, antibiotics use, diabetes care, etc. About one-third of the health professionals interviewed during case studies, noted that they look to provincial standards for best practices with respect to some of the gaps observed. Most participants in case studies also identified gaps or issues related to procedures or protocols (e.g., governing issues such as communication and information sharing between programs, operating policies, procedures or handling complaints).
Staff turnover negatively impacts quality of careFootnote 22. The community members who were interviewed as part of the case studies most commonly defined quality of care in terms of the relationship and trust they have developed with their health care providers. In fact, the literature shows that patient perception of health care quality and treatment outcomes are highly correlated with the level of trust that has been established, and effective communication, as well as perception of professional competency.Footnote 23 In one community, health staff spoke of a physician who has been able to build a strong relationship with community members over time, which resulted in increased visits, decreased cancellation of scheduled visits, and more individuals (particularly older men) opening up about their mental health Similarly, health directors identified a stable nursing staff as a key determinant of quality of care, which enables nurses to become more aware of local health concerns, familiarize themselves with the community, and connect with clients over time. A literature review conducted in Ontario (2017) found that four principles (respect, trust, self-determination, and commitment) underline successful approaches and meaningful ways of engagement with First Nations communities. Commitment is seen as part of the engagement process, which takes time and community presence among other thingsFootnote 24.
While the proper assessment and diagnosis of the client conditions or symptoms is a key determinant of quality of service, over half of health care professionals surveyed reported major gaps in services related to diagnostics (e.g., X-rays, EKGs, blood sampling). Regional reporting templates, specifically the essential care templates, also identified issues related to diagnostic tools in some communities (lack of point of care testingFootnote 25, broken X-ray machines, etc.). In all but one of the communitiesFootnote 26 visited, community members raised concerns as to whether assessment of their conditions made at the nursing stations were appropriate (e.g., some community members believe that their health concerns were not properly assessed or diagnosed by on-site health care professionals). In the absence of needed diagnostic tools and with limited access to other health professionals, nurses interviewed feel they are often caught between the demands from the community members to be transferred out for further diagnosis and treatment, and the pressures to minimize medical transfers. Some nurses noted that, without convincing diagnostics, their decision to medivac a patient can be challenged by a receiving physician. Paramedics interviewed as part of the case study talked about a need for I-STATFootnote 27 point of care testing that would help them to make more accurate diagnoses and improve the decision-making processes such as when to medivac a client.
The case study of the PEMH hospital further illustrates some of the factors contributing to high-quality health services. The document review and interviews indicate that the hospital is well managed with a stable and highly experienced nursing staff. There has been a strong emphasis on team building activities, safety improvements, and standardization of policies, procedures and forms. A number of committees have been established to plan, develop policies and procedures such as discharge planning improvements, and provide quality assurance. Families, patients and selected members of the communities are invited to provide input via one-on-one meetings or focus groups. These activities and approaches led to high client satisfaction with the services. The community members interviewed as part of the case study were generally satisfied with the services. A survey of Emergency Room clients, conducted by the hospital, showed that 63 percent of respondents rated their experience at PEMH as seven or higher (on a scale of 0 to 10, where 10 is the best experience possible). In comparison, a market research study reported that only 19 percent of Manitobans were satisfied with the hospitals in their provinceFootnote 28. When asked about factors that constrain quality of care, the hospital representatives interviewed noted that infrastructure remains the major challenge, particularly in the Norway House hospital (e.g., they cannot apply for accreditation because of the aging infrastructure).
Accreditation of health services is widely recognized as an important tool for ensuring quality of care. Two nursing stations have been accredited to date and there are plans for more nursing stations to begin the accreditation process.
According to the FNIHB Approach to Accreditation (Fall 2016) document, the Branch is committed to increasing the number of accredited health services, with a particular focus on nursing stations, by encouraging new organizations and communities to begin and remain in the accreditation process, providing ongoing support to those already engaged in the process, and establishing accreditation as an ongoing priority at all levels within FNIHB. Interest in the accreditation process has grown as the benefits of health services accreditation have been recognized. A surveyFootnote 29 reported in the Accreditation Dashboard (2016) found that accreditation leads to more appropriate care being provided to patients/clients (agreed to by 100 percent of health center representatives), better staff safety (100 percent), improved patient/client safety (97 percent), and greater pride in their organization's health services (97 percent).
Visits to an accredited health center in Quebec and the PEMH, an accredited hospital, confirmed some of these findings. PEMH has been part of the accreditation process since the 1970s, and currently holds an accreditation status with commendation. The hospital representatives interviewed highlighted the usefulness of the accreditation process in ensuring that proper policies and procedures are in place (e.g., work-life policy, patient safety policy and cultural tools, organizational standards and policies, family center, family in-patient plans, and social workers). Representatives from the accredited nursing station in Quebec noted that accreditation helped them to standardize and strengthen processes, and has been used as a marketing tool to recruit nurses (e.g., nurses are reassured that the operations and management of the centre are effective and up to standards).
Some key informants (FNIHB and a few other representatives) highlighted the importance of accreditation in ensuring standardization of practices and quality of care across all regions and communities. Accreditation is an ongoing process. It can be a lengthy and costly process that requires the participation of players at various levels, which can be very challenging given the number of stakeholders involved in the delivery of health services in First Nations communities. According to program documents and interviews conducted with representatives from accredited facilities, to be successful, accreditation must be established as a priority for the organization, and funding and human resources must be invested in quality improvement. For example, PEMH has a dedicated accreditation coordinator who is responsible for ensuring that accreditation standards are met.
According to documents provided by the program, two transferred nursing stations in Quebec have been accredited to date and two transferred nursing stations in Saskatchewan have been accredited as part of the Athabasca Health Authority. In addition, up to three non-transferred nursing stations in Alberta (John D'Or, Garden River and Fox Lake) have begun the accreditation process.
4.4.2 To what extent have the intermediate outcomes been achieved?
Intermediate Outcome #1: Clinical and Client Care services are sustainable
Program sustainability has benefited from the Nursing Recruitment and Retention Strategy (NRRS), which contributed to the hiring of 116 full-time equivalent (FTE) nurses over the past three years, resulting in a net increase of 23.1 FTEs, and a decline in vacancy rates amongst clinical and client care nurses.
One component of a sustainable program is the sustainability of its workforce, meaning the balance between the registered nurses needed to deliver the program and the supply of those nurses (i.e., the ability of the program to put those resources in place on a sustained basis)Footnote 30.
As of March 2017, there were 221.5 FTE nursing positions in communities with services managed by Health Canada, most of which were in Manitoba (107 FTEs) and Ontario (88), while the remainder are in Alberta (18.5) and Quebec (eight).
CCC's nursing positions are filled by a complement of nurses who are:
- Attached to a nursing station or health center and working full-time or part-time with Health Canada (regular nurses);
- A member of a Health Canada resource team, not permanently attached to a nursing station or health centre with treatment (resource team nurses); or,
- Employed by an agency which has a contract with FNIHB (agency nurses). The resource team nurses and agency nurses may fill ongoing vacancies as well as positions temporarily vacated by a nurse who must leave for training or is on vacation.
Staffing challenges are a reality faced by the nursing profession as a whole. Most recently, the Canadian Institute for Health Information released data indicating that "since 2013, there has been a decline in the number of new registered nurse graduates obtaining a license to practice in Canada, with the average annual growth of -3.2 percent, compared with 2.8 percent since 2007."Footnote 31 However, in addition to this overarching impact to the field at large, it is important to consider that rural and remote health care settings have an even smaller pool of nurses to draw fromFootnote 32, as fewer nurses are willing to relocate to these regionsFootnote 33. The literature review identified that in 2010, approximately 11 percent of RNs (including nurse practitioners) and 18 percent of licensed practical nurses worked in rural and small town settings, indicating an overall decrease in the percentage of nurses working in rural settings during the years of 2003-2010.Footnote 34, Footnote 35 As it pertains to remote nursing stations, the unique demands of the context within which nurses provide care, invites an even narrower criteria to determine suitability for the position. The literature suggests that personal suitability is a key consideration for nurses to withstand the complexity and challenges created by the isolated, geography and cultural dynamics present in the remote northern settings.Footnote 36 The literature review highlighted that in order for nurses to be effective in northern communities, they had to "possess a calm, skillful approach to challenging patient care situations and be extremely adaptable to change of all sorts, including the stability of client health conditions, availability of resources and equipment, and weather".Footnote 37 In addition, nurses in remote settings interviewed through the Misener study described the impact of working in remote settings, as often more intrusive on a nurse's personal life since the need is not necessarily contained to their scheduled working hours."Footnote 38
As a result of a shortage of nurses in Canada, and more specifically a shortage of nurses willing to work in R/I locations, it has long been a challenge for FNIHB to fill its nursing positions. The document review shows that vacancy rates averaged 30 percent to 40 percent in the period prior to the term covered by this evaluation. The high vacancy rates contributed to a heavy reliance on agency nurses to meet the shortfall in the supply of nurses. This increases the cost of the program to Health Canada, in that the cost of an agency nurse is over twice the cost of a fully-costed regular nurse. As such, program efforts to improve sustainability have focused primarily on the supply of regular nurses and, to a lesser extent, the supply of resource team nurses.
To help reduce the vacancy rate and improve program sustainability, Health Canada implemented the NRRS. Key elements of the NRRS included a streamlined job application process, a marketing campaign, a center for nurse recruitment and website, development of nursing pools and optimization of the staffing mix (e.g., recruiting more nurse practitioners). As shown in Table 5, over the three-year period from April 1, 2014, to March 31, 2017, Health Canada hired part-time and full-time registered nurses to fill positions representing 116.4 FTE positions. The hiring rate is defined by the total number of funded FTE nursing positions, and averaged about 18 percent.
| Nurses Hired (FTEs) | 2014-15 | 2015-16 | 2016-17 | TOTAL |
|---|---|---|---|---|
| FTEs | ||||
| Number Hired (FTEs) | 42.0 | 36.3 | 38.1 | 116.4 |
| Number of Funded FTEs as of year-end date | 216.5 | 219 | 221.5 | |
| Hiring as a Percent of FTE Nurses | 19.4% | 16.6% | 17.2% | |
As indicated in Table 6, the recruitment program was successful in reducing vacancy FTE rates, which declined from 26 percent in December 2014 to approximately 16 percent in March 2017.
| Year | 2014 | 2015 | 2016 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Month | Dec | Mar | June | Sept | Jan | April | Jun | Sept | Dec | Mar |
| Number Funded FTEs | 216.5 | 216.5 | 217 | 219.5 | 219 | 219 | 220 | 220 | 221.5 | 221.5 |
| Encumbered Nurse FTEs | 160.7 | 173.6 | 165.8 | 189.3 | 180.2 | 185.3 | 189.9 | 185.7 | 180.5 | 185.7 |
| Vacancies (FTEs) | 55.9 | 42.9 | 51.2 | 30.2 | 38.8 | 33.7 | 30.1 | 34.3 | 41 | 35.8 |
| Percentage of Vacancies (FTEs) | 25.8% | 19.8% | 23.6% | 13.8% | 17.7% | 15.4% | 13.7% | 15.6% | 18.5% | 16.2% |
Despite the progress that has been made, the benefits of the NRRS have been offset, to some degree, by continuing turnover amongst the nurses. While Health Canada has been successful in hiring 116.4 FTE nurses (198 nurses in total, full-time and part-time) for its regular nursing staff and resource teams over the past three years, 93.3 FTE nurses have departed (157 nurses in total, full-time and part-time), resulting in a net increase of 23.1 FTEs. The staff turnover rate for the past three years has averaged 17.1 percent and amounted to 19.8 percent in 2016-17.
| Costs | 2014-15 | 2015-16 | 2016-17 |
|---|---|---|---|
| Number of Nurses Departing (FTEs) | 29.2 | 27.3 | 36.8 |
| Encumbered Nurses (FTEs) | 173.6 | 185.3 | 185.7 |
| Average FTE Nurse Turnover Rate | 16.8% | 14.7% | 19.8% |
In 2016-17, the level of hiring in terms of FTE positions (38.1), outlined in Table 5, was almost the same as the level of departure (36.8 FTEs) noted in Table 7.
Two factors were identified by key informants as possibly contributing to the increased staff turnover rate in 2016-17, relative to the previous year. Issues identified were associated with challenges experienced through the Phoenix Pay System and the movement towards hiring recent nursing graduates who may be more likely to only work in the communities for perhaps two to three years until they have enough experience to gain employment elsewhere.
Work stress, availability of other opportunities, the remote and isolated location of the communities, and working conditions are the primary contributors to continued staff turnover. Suggestions to reduce turnover focused mostly on increasing staffing levels, improving working conditions, and increasing efforts to recruit directly from First Nations communities and promoting careers in health professions to youth from those communities.
Over three-quarters of health professionals surveyed agreed that the level of turnover amongst clinical and client care nurses is high in the community or communities in which they work. The three contributing factors reported most often are work stress (87 percent), wages and benefits being better elsewhere (66 percent), and the remote and isolated nature of the community (54 percent).
| What are the major factors that contribute to the high rate of nurse turnover in this region or community? | N =92 | % |
|---|---|---|
| Work stress | 80 | 87 |
| Wages and benefits are better elsewhere | 61 | 66.3 |
| The location of the community (e.g., remote and isolated) | 50 | 54.3 |
| The opportunities available elsewhere | 37 | 40.2 |
| Family issues | 35 | 38 |
| Working conditions | 32 | 34.8 |
| Concerns about the scope of practice | 26 | 28.3 |
| Other | 20 | 21.8 |
Working conditions included concerns related to a variety of issues including facilities and accommodation, lack of support from management, harassment, vicarious trauma, and workplace conflict. "Other" challenges included issues such as staffing issues (e.g., understaffed centres), hours and workload, and issues with the Phoenix Pay System.
During the community visits, nurses often spoke about work stress and burnout. Contributing factors included long working hours including extended on-call hours (all five communities reported that they are understaffed relative to the demand for services); the stress associated with ensuring that urgent cases are transported out of the community in a timely manner; and being the target of verbal abuse and blame. According to program internal documents, general violence towards nurses, including verbal and physical threats, has been on the rise. This issue of violence against nurses is not unique for Health Canada nurses. A recent discussion paper published by Canadian Federation of Nurses Unions highlights the increase in rates of violence against nurses across Canada as well as globally.Footnote 39
To increase recruitment and retention, nurses suggested that staffing levels increase and that Health Canada and community leaders should work together to ensure that nurses are accepted, respected and have basic needs met while in the community (safety; appropriate accommodation with basic requirements met - like pots and pans for cooking)Footnote 40. Having strong management support and a supportive on-site team and flexible schedule were the factors most commonly noted as contributing to retention. Some stakeholders (e.g., regional health authorities and associations) suggested that increased emphasis should be placed on recruiting directly from the communities as well as reinforcing a positive message, through elementary schools and through summer camps, about the benefits of getting into health professions. The representatives from Saskatchewan noted that, while they continue to struggle with recruitment, turnover rates in that province have declined as a result of some communities successfully recruiting Indigenous nurses and offering a better wage package.
When asked about the promising practices regarding the recruitment and retention of nursing staff, BC FNHA representatives interviewed emphasized the investments they made in promoting health careers (particularly scholarships, bursaries and support for health and wellness education provided to recruit and retain First Nations and Indigenous individuals in the health system). Health Canada made similar investments through the Aboriginal Health Human Resources Initiative (AHHRI), which was established to support education and training activities related to health programs and services. When asked if they have made use of the Initiative, most regional representatives and about half of Health Directors reported being aware of it but very few have used it (e.g., amounts were too small; it was not applicable for their communities). A few respondents used the AHHRI for mental health and addiction workers, and health managers training. About three-quarters of health professionals surveyed were not familiar with the AHHRI.
Intermediate Outcome #2: Clinical and Client Care services (including hospitals) are responsive to the needs of First Nations in remote and isolated communities.
First Nations representatives participating in the surveys and interviews reported that the members of their communities are generally satisfied with the CCC services. Program responsiveness is linked to effective community engagement and continuity of care, which requires effective service integration across various programs and providers.
Nearly all community members interviewed as part of case studies reported that they are generally satisfied with the services received at the nursing stations. Where concerns were raised, they related largely to communication issues (e.g., inability to raise concerns about a specific nurse or treatment) or the limited access to other services (such as mental health services, physicians, pediatricians, and transportation to hospitals) which are largely beyond the scope of the CCC program itself. The health professionals surveyed were somewhat divided in their opinions as to whether community members are satisfied with the quality of clinical and client services (40 percent agreed with the statement that community members are satisfied, 29 percent neither agreed nor disagreed, and 20 percent disagreed).
The findings of the case studies, surveys and interviews point to two key factors as influencing responsiveness: having clear avenues available through which community members can engage and communicate their concerns; and providing continuity of care. Transferred communities may have some inherent advantages both with respect to communicating with the community and coordinating services. The health professionals who work only in First Nations managed nursing stations were more likely to report that community members are satisfied with the clinical and client care services than respondents who work only in Health Canada nursing stations. Seventy-four percent of health professionals who work only in First Nations managed communities agreed or somewhat agreed that community members are satisfied, as compared to 38 percent of those who work only in Health Canada operated nursing stations. These two factors are further discussed below:
- Clear avenues for community members to raise and communicate their concerns. Responsiveness requires an understanding of community needs and concerns. Some key informants (FNIHB regional representatives and health directors) highlighted the importance of a formal feedback mechanism and process through which the community can be meaningfully engaged in service improvement and can express their opinion and concerns (e.g., determining clinic hours, quantity of staff, security concerns, etc.). In the two transferred communities visited as part of the case studies, Health Directors serve as an avenue of communication between the clients and the clinic, and respond to client concerns. In the Health Canada managed communities which were visited, there were no formal avenues for raising issues and concerns with management (e.g., community members did not know where, how or to whom they would talk to about concerns related to treatment received at the nursing station). Recognizing the need to improve communication, FNIHB regions have developed a communication strategy for each community which identifies processes and tools in place to communicate services and engage community members. The evaluation was not able to verify to what extent these strategies have been implemented or their effectiveness. The BC FNHA review illustrates an alternative approach to improve communication and responsiveness; the FNHA has established eight Aboriginal Health Improvement Committees with the goal of identifying health care service issues in remote communities, creating resources specific to their communities, and working together towards finding solutions to these issues (e.g., developing local cultural resources, encouraging cultural safety in health care).
- Continuity of care. Continuity of care is impacted by the coordination of services across various service providers along the continuum. At the community level, a strong factor contributing to integrated and coordinated services is well respected and trusted nurse managers and health directors who serve as a catalyst for information sharing and collaboration. For example, in a transferred community in Quebec, the Band Council meets with the Health Director regularly, who in turns works very closely with the nurse-in-charge to communicate the needs and share the responsibilities. At the provincial level, an Indigenous advisor liaison position was created a few years ago to improve coordination of services between the province and the community. In some Health Canada managed communities, for example, nurses work very closely with community care workers to share information and discuss scheduled appointments, medication or follow-up care.
However, while there are examples of effective coordination, both key informants and health professionals expressed concerns regarding the level of coordination overall. Most key informants noted that coordination with provincial governments is limited, and some noted challenges related to siloed health programs delivered by various providers (e.g., lack of information sharing which creates difficulties related to case management). Similarly, only 19 percent of health professionals surveyed agreed that there is good coordination between the federal and the provincial government with respect to the delivery of clinical and client care services.
To help address these issues, some formal collaboration mechanisms have been established. Alberta established a Health Co-Management committee, which brings together FNIHB , provincial and First Nations partners. They worked together on developing a joint action health plan which allowed for a higher-level policy planning and service integration and coordination. Another example where effective collaboration is occurring at the national and regional levels is an initiative that brought together multiple partners (nursing associations, universities, unions) to support the recruitment of nurses through implementation of marketing strategies, development of programs for rural and remote practice, and training activities (e.g., Health Canada Sustainability Report 2016-17-Q3, notes that a training partnership has been pursued with the Department of National Defence). However, most key informants were not able to identify any formal collaboration mechanisms established to address interjurisdictional issues with respect to data sharing, privacy legislation, or expended access to care (access to mental health professionals).
Strong management capacity (particularly in terms of stable and experienced staff) and effective community engagement, were identified by health directors as key to building community capacity and supporting the processes for transferring the management of services (to date, 34 percent of the nursing stations and health centers with treatment have been transferred). A few health directors stated that institutional distrust of government and its intentions remains a barrier to community engagement, communication and ultimately the effective transfer of services. This mistrust continues to create barriers to effective data collection and information sharing.
Culturally safe clinical care is understood differently by various health providers. First Nations representatives emphasized the need to improve cultural safety and strengthen cultural competencies.
Health Canada's quality improvement policy defines cultural safety and cultural competencies as "integrating knowledge about First Nations individuals, families and communities into specific health program and services standards, policies, practices and attitudes." An on-site assessment completed by Health Canada in two nursing stations in 2016, assessed cultural competency based on two criteria: whether translators and cultural training were available. The assessments concluded that translators are available but that cultural training is provided inconsistently.
When asked about culturally safe services in this evaluation, most key informants also talked about the extent to which cultural training is provided to health professionals. A majority reported that some cultural training is provided as part of the orientation but is not provided consistently across communities. Seventy percent of health professionals surveyed agreed that the services are provided in a manner that is culturally safe to First Nations. However, some health professionals noted that all health staff should be more culturally sensitive and aware of consequences of colonialism, the impact of negative stereotypes on service provision, and the importance of relationship building and understanding traditional practices. Most health directors noted insufficient cultural sensitivity in the delivery of care (e.g., lack of understanding of First Nations history and culture, social determinants of health, stereotypes in diagnosis and care).
Interviews conducted with health professionals during the case studies illustrated that no common understanding exists regarding what are considered culturally safe services or practices. Examples ranged widely:
- Simply recognizing traditional medicine (e.g., encouraging clients to share any health concerns for which they may be using traditional medicine to ensure that the primary caregiver has a more complete picture of the health status of their patients).
- Providing advice regarding traditional medicine (e.g., advising patients who are diabetic about how to participate in the traditional activities or treatments such as fasting while not compromising their health).
- Making translators available (particularly for elderly residents and for after-hours care when community health workers are not available).
- Using culturally appropriate language (e.g., in one study, First Nation representatives talked about the difference in the traditional and western view of health and health care, noting the relative emphasis on wellness rather than curing the diseaseFootnote 41).
- Having appropriate physical spaces through which to deliver the services (e.g., having rooms that are spacious and able to accommodate large families, and in-patient rooms, which have space for family members to spend a night; the PEMH also has built a gazebo at the back of the hospital for family members to gather).
4.4.3 To what extent has the longer-term outcome been achieved?
Long Term Outcome: CCC programming contributes to the health status of First Nations in remote and isolated communities
By delivering essential primary care services, including "urgent and emergent care" after hours, the CCC programming contributes to the health status of First Nations individuals in R/I communities. However, improving health outcomes of First Nations communities will require a population health approach and better integration of various health programs which goes beyond the scope of this program.
Health professionals provided examples of different ways in which CCC services contribute to positive health outcomes including lives saved by stabilizing patients and transferring them to hospitals, increased immunization rates, and better management of chronic illnesses resulting in people living longer and having better quality of life. Some nurses noted that having dedicated resources for pre-natal programs improved the health of mothers and babies. Community members noted the positive impact of the services on their lives by not having to leave the community to receive essential care.
However, perceptions of key informants and health professionals regarding the impact of the CCC Program on the health status of First Nations in R/I communities are tempered by the continuing disparities in the health outcomes of the residents, relative to the Canadian population as well as by a lack of data on service outcomes. While over half of health professionals surveyed agreed that the CCC services have contributed to the health of First Nations individuals, this contribution is not necessarily reflected in improving health outcomes. A majority of key informants, about 15 percent of the nurses surveyed, and some provincial representatives reported that health outcomes of First Nations communities have not improved. Some key informants argued that on-reserve health has declined in recent years due to a high burden of diseases (e.g., obesity, diabetes, complex trauma issues, addictions). They attributed the limited improvement made with respect to health outcomes, to the continuing challenges in providing more coordinated and integrated health care across entire spectrum of programs, and the failure to address social determinants of health.
To improve outcomes, some key informants stressed the need to move further towards a population health approach that is more responsive to the unique characteristics of First Nations populations and find systemic solutions to addressing health care issues, rather than a series of initiatives that each focus on one aspect of health care. They noted that improving health outcomes will require rethinking the entire spectrum of health system interventions, from prevention and promotion to diagnosis, treatment, and management of care. Key informants also suggested increasing access to data on health outcomes for planning purposes, and assessing the impact of services on health outcomes. Furthermore, it was expressed that there is a need for a greater focus on health prevention. For example, most health directors and some nurses noted that services focus too heavily on treating the symptoms and not the causes of the health issues. Other suggestions brought forward by key informants for improving health outcomes included: being more responsive to mental health concerns, increasing the level of integration with the provincial system, increasing early access to diagnosis, and dealing more effectively with diseases which are increasing in incidence (e.g., diabetes, respiratory issues, obesity).
4.5 Performance: Issue #5 – Demonstration of Economy and Efficiency
From 2011-12 to 2016-17, CCC program expenditures increased by an average of 6.0 percent annually, rising from $139.7 million in 2011-12 to $187.3 million in 2016-17.
The table below summarizes annual expenditures by program component covering the period from 2011-12 (the year prior to the term on which the evaluation focuses) through 2016-17. Over the past five years, expenditures increased by $48 million, consisting largely of increases in direct nursing service delivery costs (accounting for about $26 million in increased expenditures) and increases in policy development and program oversight (increase of about $13 million).
| 2011-12 | 2012-13 | 2013-14 | 2014-15 | 2015-16 | 2016-17 | 2012-13–2016-17 | ||
|---|---|---|---|---|---|---|---|---|
| Nursing – Direct Service Delivery | $ | 87,686,023 | 96,394,587 | 101,045,102 | 104,667,904 | 108,165,671 | 113,304,080 | 523,577,344 |
| % | 63 | 65 | 64 | 58 | 60 | 61 | 61 | |
| Hospital Services | $ | 22,031,874 | 19,485,044 | 21,236,332 | 22,623,210 | 23,333,592 | 23,368,046 | 110,046,224 |
| % | 16 | 13 | 14 | 13 | 13 | 12 | 13 | |
| Other – Direct Service Delivery | $ | 12,038,111 | 12,887,465 | 12,333,730 | 20,460,727 | 17,028,370 | 16,623,942 | 79,334,234 |
| % | 9 | 9 | 8 | 11 | 9 | 9 | 9 | |
| Supplies and Equipment | $ | 10,555,960 | 10,890,530 | 11,286,970 | 11,018,462 | 10,859,805 | 12,285,431 | 56,341,198 |
| % | 8 | 7 | 7 | 6 | 6 | 7 | 7 | |
| Policy Development and Program Oversight | $ | 3,473,284 | 4,034,752 | 6,605,511 | 17,558,874 | 17,098,772 | 17,207,050 | 62,504,959 |
| % | 2 | 3 | 4 | 10 | 9 | 9 | 7 | |
| Professional Development | $ | 3,887,772 | 3,827,937 | 4,369,202 | 4,254,388 | 4,993,374 | 4,481,539 | 21,926,440 |
| % | 3 | 3 | 3 | 2 | 3 | 2 | 3 | |
| Total Expenditures | $ | 139,673,024 | 147,520,315 | 156,876,847 | 180,583,565 | 181,479,584 | 187,270,088 | 853,730,399 |
| % | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |
Nurses are the primary resource of the CCC program, accounting for 61 percent of total costsFootnote 42 over the five years. The direct service delivery costs for nursing consist almost entirely of salary costs, payments to agencies that supply nurses under contracts, and contribution agreements with transferred communities related to nursing costs. Other non-nursing expenses include hospital services (13 percent), direct service expenses not including nurses (nine percent) e.g., salaries and contribution agreements related to positions other than nurses which work in the nursing stations), supplies and equipment (seven percent), policy development and program oversight (six percent) and professional development (three percent).
Hospital expenditures include salaries (an average of 38 percent of total expenditures), operating costs (an average of 10 percent), and other contributions (an average of 62 percent). The financial information available does not provide further analysis of hospital contributions.
During the five-year period, nursing direct delivery expenditures grew at the rate of 5.3 percent while professional development costs grew at the rate of 2.9 percent. The increase in professional development costs reflects the increased emphasis placed on training (this includes training delivery costs as well as the cost of the wages for the nurses taking the training). All other costs grew at the rate of 4.5 percent.
The increase in policy development and program oversight expenditures is attributed primarily to a shift in accounting policy within FNIHB. Prior to 2014-15, corporate management salary expenditures were not allocated to specific programs (e.g., the CCC program) but rather were reported as a separate item. Beginning with 2014-15, these costs are now allocated proportionally across all FNIHB programs, including CCC.
Excluding policy development and program oversight, expenditures increased at the average rate of 4.3 percent annually (which is somewhat higher than the average increase in total healthcare expenditures in Canada of 2.8 percent, according to data compiled by the Canadian Institute for Health Information).Footnote 43 The increase in program expenditures was supported, in part, by additional time limited funding Health Canada received to address Primary Care nursing cost drivers, referred to as the Program Integrity Fund. The Program Integrity Fund has provided the program with $211.4 million over a five-year period (2013-14 to 2018-19) to simultaneously address key cost drivers while implementing a Treasury Board mandated cost control strategy for Primary Care nursing. This funding was intended to sustain the Program while it implements its long-term Strategy for Modern Sustainable High-Quality Health Services.
Program economy is determined primarily by the costs of nursing, which in turn are a function of the relative balance in expenditures between nurses working regular hours, nurses working overtime, and agency nurses. While some progress has been made with respect to containing nursing costs, expenditures on nursing direct service delivery have continued to grow.
Nursing costs consist of four main types of expenditures: salaries paid to regular nurses and resource team nurses; overtime paid to regular nurses and resource team nurses; payments to agencies for agency nurses; and contribution agreements with transferred communities related to nursing service delivery. Resource team nurses and agency nurses are both used primarily for short-term placements. For example, most of the assignments (88 percent) of agency nurses involve call-ups of 15 days or less, with only 2.4 percent involving call-ups of 30 or more days.
Overtime occurs mostly when clinic times go beyond the normal working hours, which could be between 7:00 am and 6:00 pm. Standby and call back are used during evenings, nights, and weekends as a measure to ensure access to urgent or emergent services outside normal working hours. Consequently, a significant contributor to costs related to overtime, callback, and standby work is the hours of operation of the clinic.
Overtime is most commonly paid at 1.5 times the regular wage while the cost of an agency is approximately twice the cost of a nurse working regular time. Health Canada implemented a cost containment strategy focused primarily on increasing the number of regular nurses and resource team nurses as a means to reduce the reliance on overtime, standby, callback and agency nurses to meet needs. As indicated below, the total nursing costs (excluding transferred communities) decreased from $63.7 million in 2012-13 to $59.8 million, in 2014-15, before increasing in each of the past two years, reaching $66.3 million in 2016-17. Of this amount in 2016-17, 34 percent consisted of regular time salary costs for nurses including resource team nurses, 21 percent consisted of overtime costs, and 45 percent consisted of payments to agency nurses.
| Costs | 2012-13 | 2013-14 | 2014-15 | 2015-16 | 2016-17 |
|---|---|---|---|---|---|
| Expenditures on Direct Nursing Service Delivery ($ millions) | |||||
| Regular salary | $20.8 | $19.4 | $23.2 | $23.6 | $22.8 |
| Overtime(OT/SB/CB) * | $11.8 | $12.8 | $13.8 | $13.7 | $13.9 |
| Sub-total, Health Canada staff | $32.6 | $32.2 | $37.0 | $37.3 | $36.7 |
| Agency nurses | $31.1 | $28.8 | $22.8 | $25.2 | $29.6 |
| Total | $63.7 | $61.0 | $59.8 | $62.5 | $66.3 |
| Percent of Expenditures on Direct Nursing Service Delivery | |||||
| Regular salary | 32.7% | 31.8% | 38.8% | 37.8% | 34.4% |
| Overtime(OT/SB/CB) | 18.5% | 21.0% | 23.1% | 21.9% | 21.0% |
| Sub-total, HC staff | 51.2% | 52.8% | 61.9% | 59.7% | 55.4% |
| Agency nurses | 48.8% | 47.2% | 38.1% | 40.3% | 44.6% |
| Total | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% |
| Number of FTE Nurses | |||||
| Number of FTEs | 216.5 | 216.5 | 216.5 | 219 | 221 |
|
Sources: Nursing Dashboards; Chief Financial Officer Branch |
|||||
Overtime costs have not been reducedFootnote 44. Overtime occurs mostly when clinic times go beyond the normal working hours (which could be between 7:00 am and 6:00pm). Standby and call back are used during evenings, nights and weekends as a measure to ensure access to urgent or emergent services outside normal working hours. Consequently, a significant contributor for costs related to overtime, call back and standby is the hours of operation of the clinic.
The financial data indicates that the program did make progress in reducing agency costs. Relative to the baseline of $31.1 million in annual expenditures in 2012-13, the program has achieved aggregate savings on agency nursing over the past four years totaling about $18 million. However, after declining in the two previous years, agency costs increased in each of the last two years. This appears somewhat inconsistent with the data presented earlier, which indicated that nursing staff vacancy rates have continued to decline in the past two years as a result of the increased hiring and further development of resource teams (which suggests there would be a reduced reliance on agency costs). According to program documents, a contributing factor to the rising costs last year was having to rely on agency vendors with higher hourly rates for nurses.
The total value of the contribution agreements with transferred communities for direct nursing costs totalled $33.8 million in 2012-13, increasing to $40.1 million in 2016-17 (equal to an average annual increase of 4.4 percent).
The evaluation was not able to assess the effectiveness of resource allocation or utilization for First Nations managed communities because they are not required by Health Canada to report on the program other than submitting annual Community Based Reporting Template reports. However, there is data available on the population of the transferred communities. The population in the transferred communities totals 42,164, which means the nursing expenditures were equal to about $950 per resident in 2016-17. In comparison, the population in the non-transferred communities totaled 70,426, which means the nursing expenditures of about $66.3 million, detailed in Table 11, would be equal to about $941 per resident in the same yearFootnote 45.
| Transferred | Non-transferred | Total | |
|---|---|---|---|
| 2016-17 Expenditures ($ millions)Footnote 46 | $40.1 | $66.3 | $106.4 |
| Population | 42,164 | 70,426 | 112,590 |
| Per Capita | $951 | $941 | $945 |
Source: INAC First Nations Profiles population data, Chief Financial Officer Branch |
|||
The allocation of nursing resources is based more on historical factors than an assessment of community needs. There are concerns as to whether existing nurse staffing levels are adequate.
The Auditor General report (2015) recommended that Health Canada should work with First Nations communities when allocating nursing staff levels and other supports. According to the key informants interviewed including national and regional FNIHB and some nurse managers, resources are generally allocated based on a combination of historical patterns, population, and comparability of services (e.g., establishing a baseline regarding FTEs per 1,000 persons). Some FNIHB representatives and health directors suggested that the allocation of resources is a matter of equity of health care provision for First Nations communities and should be based on the assessment of needs and priorities rather than, for example, comparable service levels.
INAC data (2016) reports 70,426 residents in the 52 communities with services managed by Health Canada, which means that there are 3.15 nurses per 1,000 residents The number of nurses per 1,000 residents varies by region, tending to be higher in Alberta and Quebec (which have fewer Health Canada managed stations) than in Manitoba or Ontario.
As noted earlier in the report, the survey of health professionals and case studies both identified concerns that nursing stations are understaffed which contribute to work stress, burnout and turnover. Most FNIHB regional representatives and health directors reported that the program makes effective use of the available resources, while noting that additional resources are required to deal with the increasing population, increasing demand for pre-natal programs, aging demographic, complexity of health issues and co-morbidity of diseases. In addition to nursing, areas identified where additional resources are needed included data collection and management, community health programs, mental health services and transportation infrastructure.
The CCC program is not making full use of available technology, particularly telehealth that could more cost-effectively deliver services.
According to the eHealth Infostructure Program Evaluation (2017), telehealth services are currently available in 93 percent of CCC nursing stations (a secure video and sound connection with enhanced capabilities of transferring real-time patient health data), helping to link patients to physicians and allied health professionals, allowing for consultations without arranging travel to and from communities. Literature shows that a remote presence technology such as robotics have a potential to increase access and quality of care, reduce stress for nurses and travel cost for transferring patients out of the community.Footnote 47,Footnote 48
Only about one-third of surveyed health professionals agreed that the program makes good use of available technology. While a majority of the key informants indicated that use of technology (videoconferencing/telehealth services for physician/specialist consults) has somewhat improved, it was noted that challenges still exist in training staff with respect to using the software and incentivizing physicians to consult through the service (e.g., in some regions, fee for service arrangements for physicians exclude services delivered via telehealth). Only two of the five communities, which were visited, used telehealth regularly.
When asked about constraints in leveraging technology for the delivery of services, the health professionals reported limited connectivity/bandwidth in some communities, insufficient staffing levels and support, challenges in remuneration for physicians consulting via telehealth, cultural differences (e.g., telehealth services seen as impersonal), lack of clarity regarding jurisdiction (e.g., clear allocation of responsibilities for funding technology infrastructure, network security and adhering to privacy legislation), budgetary/funding limitations, and lack of education and awareness of how to use telehealth services (both for staff working on-site and community members).
These finding are consistent with a more global assessment of Health Canada's telehealth services through the eHealth evaluation, in which approximately half of survey respondents indicated efforts have not been successful in developing eHealth skills and knowledge in First Nations and Inuit communities. The eHealth evaluation also found there is a "lack of cooperation from physicians who are not inclined to participate in telehealth due to remuneration concerns".Footnote 49
While the CCC program has significantly improved data collection and reporting structures to monitor performance across the regions, further improvements are needed with respect to data collected on service utilization.
The FNIHB introduction of templates such as quarterly dashboard reports and the Sustainability Report has helped to significantly improve reporting. The data collected through these reports provide analysis by region and some comments on factors contributing to changes in results (although the rationale provided often does not change from report to report). Further documentation of reasons for the changes in, for example, level of training or increase use of agency nurses, may be useful.
The Nursing Station Reporting Templates were developed to roll up information on the number of unique clients accessing services, number of CCC urgent versus non-urgent visits during regular hours and after hours, and collaborative service delivery agreements. One area of performance measurement where the program has not been able to make much progress is collecting data on service utilization. This is mostly due to the lack of electronic data systems or effective systems across communities to collect data on a number of unique persons using services, types of health concerns being addressed, the number and reasons for medivaced patients.
5. Conclusions
5.1 Relevance Conclusions
For First Nations living in remote and isolated communities serviced by the CCC program, there are no local alternative options for essential primary, urgent, and emergent health care services. As such, the provision of these services is consistent with the tenets of equal access outlined in the Canada Health Act (1984) and the need to improve Indigenous health outcomes, as articulated by the Indian Health Policy (1979).
The evaluation also found evidence of the program's alignment with overarching roles, responsibilities, and priorities of both the federal government and Health Canada's First Nations and Inuit Health Branch. However, the extent to which the CCC program is responsive to the priorities of the communities it serves is difficult to determine due to the nature of the program (e.g., largely reactive to emergent and urgent needs), limited community engagement in primary care, and little reliable data on utilization of services.
Irrespective of government mandate or priorities, the continued need for CCC programming is evident when considering the significantly poorer health outcomes experienced by First Nations compared to non-First Nations individuals. This is exacerbated by the complexity and high rates of chronic disease, as well as the significant presentation of First Nations individuals living with more than one health condition.
5.2 Performance Conclusions
Overall, communities are generally satisfied with the CCC services and hospital care they receive. The program has effectively improved clients' access to, and receipt of, quality care. By exploring interdisciplinary models of care, the program has facilitated greater access to a range of health care professionals, including nurse practitioners. Albeit, challenges still vary across regions related to accessibility of physicians; and progress in hiring more nurse practitioners has not reached all communities. The program's expanded use of interdisciplinary models of care have allowed CCC sites to mitigate challenges raised by the 2015 Office of the Auditor General audit that found nurses were providing care that was beyond their legislated scope of practice.
The main challenges raised by key informants in regards to accessibility of CCC services were often outside of the scope of the program (e.g., the condition and capacity of facilities, medical transportation, and road access); thus, further highlighting the need for communication and collaboration across portfolio areas.
Key informants also identified limitations in equipment and diagnostic tools, staffing shortages, and limitations in the effective use of telehealth and other service based technologies as barriers to access.
Cost-effective alternatives/complementary approaches to delivering care have, to a certain extent been resourced in communities, yet barriers still exist in fully maximizing their use. Currently, 93 percent of sites with CCC programming are equipped to offer telehealth services. Key informants were clear in saying the technology is available but challenges still exist concerning sufficient bandwidth, connectivity, staff's awareness and comfort level in operating the equipment, and a lack of clarity surrounding remuneration arrangements for physicians providing care through telehealth. Ultimately, making full use of available technology could contribute to further efficiencies and potential cost savings in service delivery, while also providing greater opportunity to offer staff training at a distance.
In terms of ensuring staff are equipped to provide quality care, compliance with mandatory training has markedly improved. Staff completion rates increased from 27 percent in June 2015 to 60 percent in March 2017. However, they vary significantly across regions, affected by factors such as: timing and availability of course instructors; access to nurses to replace nursing staff requiring re-certification; as well as staff turnover. Furthermore, the evaluation found evidence that staff did not always feel properly prepared to work in the setting of a remote and isolated First Nation community due to limited awareness of the culture.
Although the program is aware that staff do not intend to commit to a CCC nursing position for the length of their career and there is a certain degree of understanding that turnover is a natural state for the program, there continues to be higher than expected turnover rates. For example, in 2015-16 alone, the program hired 65 nurses, while facing 60 departures in that same year. Primary contributors to staff turnover identified through the evaluation included: work stress, availability of other opportunities, the remote and isolated location of the communities, and overall working conditions.
On the whole, since the implementation of the Nursing Recruitment and Retention Strategy in 2012-13, nurse vacancy rates have decreased from 40 percent to 16.2 percent, as of March 2017. While there is still reliance on agency nurses a cumulative cost savings of $18 million has been realized, far exceeding the intended cost savings of $2 million by 2016-17. This reduction in costs has been made possible due to fewer agency nurse hours, but as a result of increased agency rates, continues to be a cost driver irrespective of the fewer shifts filled by temporary staffing agencies. In addition, the program continues to have significant expenditures related to extended hours (overtime, callback, and standby), but has since begun discussions to restructure parameters around extended work hours in an attempt to establish overtime guidelines that are more consistent with the structure of nursing station/health centre work.
By delivering essential services, including urgent and emergent care after hours, the CCC program positively contributes to the health status of First Nation individuals in remote and isolated communities. However, achieving significant improvements in residents' health outcomes requires a multi-faceted approach where CCC is just one of many programs integrated into a service delivery landscape that captures the broad continuum of community-based programs for First Nations. At this point in time, there continues to be limited integration with provincial health services; as well as communication and collaboration between primary, home care, and other community-based programming such as mental wellness. In effect, the siloed program structure, as well as the multitude of programs and service providers, makes it challenging to ensure an integrated approach to both the planning and delivery of health care services.
6. Recommendations
The findings from this evaluation have led to the following four recommendations:
Recommendation 1:
Contribute to greater continuity of care by enhancing data collection, communication and sharing of information across health care providers in different jurisdictions.
To achieve greater integration of services and a stronger continuum of care, the degree of communication and collaboration among federal health programming for First Nations (e.g., Home and Community Care, Mental Wellness), and across health providers in different jurisdictions (including First Nations communities) should be strengthened. Areas for consideration include: enhanced data collection/reliability, and sharing of information to help better inform planning and decision making.
Recommendation 2:
Make more effective use of technology in the delivery of care and for training purposes.
Telehealth and other technologies available in most communities are currently not being used to their full potential. Action is required to address factors that can constrain the use of technology including connectivity issues (limited bandwidth), a lack of training and technical support, maintenance issues, and limited buy-in from service providers. In addition, there is opportunity to maximize the use of technology in delivering training for frontline CCC staff.
Recommendation 3:
Strengthen nurse recruitment and retention strategies, including efforts to address conditions that contribute to high rates of turnover amongst nurses.
There is a particular need to address conditions that contribute to nurse turnover. This involves addressing some of the root causes related to: scope of practice; security and safety; management and operation of nursing stations; and, overtime. Research including data mining, a labour market analysis, and a survey of existing and former Health Canada nurses would enable the Department to better understand the drivers of turnover such that more effective retention strategies could be developed.
Recommendation 4:
Ensure that formal cultural training is available and completed by all nurses employed in remote and isolated First Nations communities.
In order to provide responsive health services, it is important that CCC staff have a certain degree of cultural understanding. In recognition of the diversity First Nations communities, it is also important that training offered be tailored to reflect the communities each CCC site serves. As it stands, cultural training is currently provided as part of the orientation for new nurses, but the quality, structure, and consistency with which training is offered often varies. Ensuring that all nurses, both new and longer-term employees, have formal cultural training may help positively contribute to the quality of care provided, and ease staff concerns related to their preparedness for providing health services in remote and isolated First Nations communities.Appendix 1 – Logic Model
Logic Model for Clinical and Client Care Program
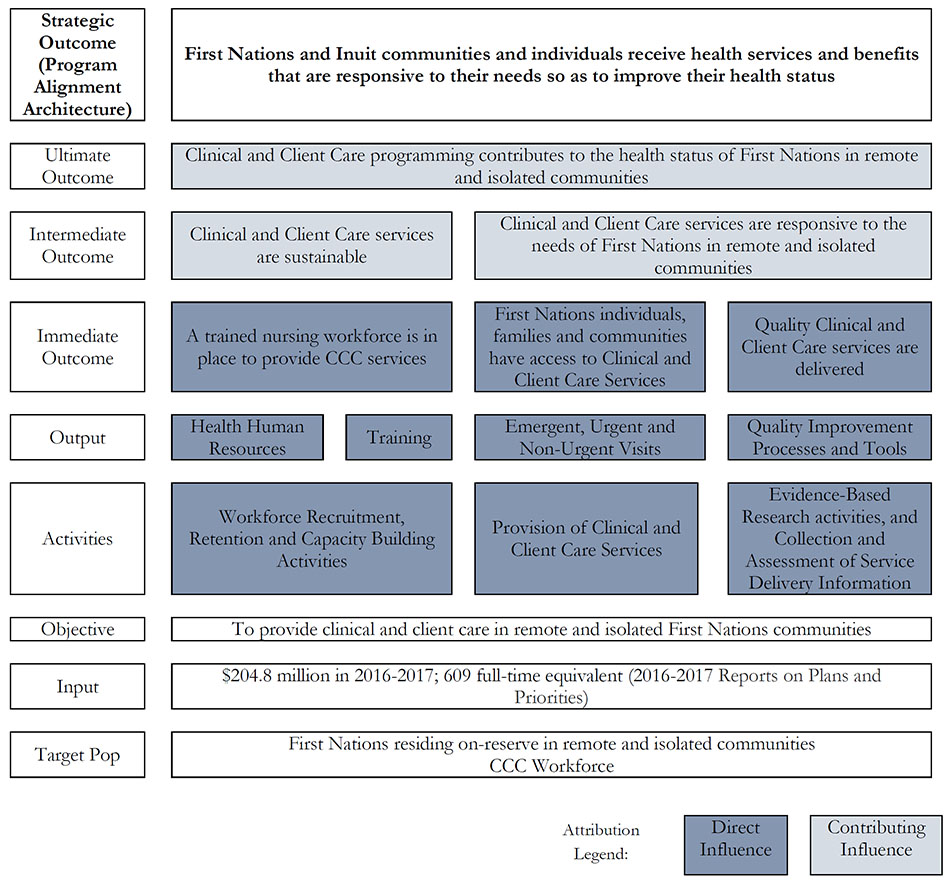
Description of Logic Model for Clinical and Client Care Program
The main target population of the program is First Nations people residing on-reserve in remote and isolated communities. Based on the 2016-2017 Reports on Plans and Priorities, the input of the program is to administer $204.8 million in 2016-2017 as well as 609 full-time equivalent. As a main objective, the Clinical and Client Care Program is to provide care services in remote and isolated First Nations communities.
The first activity: Workforce recruitment, retention and capacity building activities connects with the first program output: Health human resources, and the second program output: Training.
The second activity: Provision of clinical and client care services links with the third program output: Emergent, urgent, and non-urgent visits.
The third activity: Evidence-based research activities, and collection and assessment of services delivery information connects with the forth program output: Quality clinic and client care services are delivered.
The first and second outputs: Health human resources and training will generate the first immediate outcome: A trained nursing workforce is in place to provide CCC services.
The third output: Emergent, Urgent, and non-urgent visits will produce the second immediate outcome: First Nations individuals, families, and communities have access to clinical and client care services.
The fourth output: Quality improvement processes and tools will generate the third immediate outcome: Quality clinical and client care services are delivered.
The first immediate outcome: A trained nursing workforce is in place to provide CCC services links with the first intermediate outcome: Clinical and client care services are sustainable.
The second and third immediate outcomes: First nation individuals, families, and communities have access to clinical and client care services; and, Quality clinical and client care are delivered link with the second intermediate outcome: Clinical and client care services are responsive to the needs of First Nations in remote and isolated communities.
The first intermediate outcome: Clinical and client care services are sustainable; and the second intermediate outcome: Clinical and client care services are responsive to the needs of First Nations in remote and isolated communities. The both generate the ultimate outcome: Clinical and Client Care programming contributes to the health status of First Nations in remote and isolated communities.
It is important to note that the activities, outputs, and the immediate outcomes are direct influences. The intermediate outcomes and the ultimate outcome are contributing influences.
The ultimate outcome: Clinical and Client Care programming contributes to the health status of First Nations in remote and isolated communities will generate the strategic outcome of the program which is: First nations and Inuit communities and individuals receive health services and benefits that are responsive to their needs so as to improve their health status.
Appendix 2 – Evaluation Description
Evaluation Scope
The objective of the evaluation is to assess the relevance and performance (effectiveness, efficiency and economy) of the CCC program. It will provide the Deputy Minister of Health Canada as well as senior management with information to support decision-making regarding the contribution of the CCC program to the health and safety of First Nations.
The period covered by the evaluation includes activities from April 2012 to March 2017. However, information and data (assessments, performance reports and previous evaluations of related programs) prior to April 1, 2012, may be used to provide context or used to inform trend analysis. The evaluation will build on previous evaluation conducted in 2012, and will also examine other evaluation reports, including their accompanying Management Response and Action Plans and associated progress reports, as well as any previous relevant reports of the Office of the Auditor General and any internal Health Canada audit reports.
The evaluation is to address the core issues and provide answers to the evaluation issues and questions presented in the following table.
| Evaluation Core Issues | Proposed Lines of Questioning |
|---|---|
| Relevance | |
1. Continued Need for Program Assessment of the extent to which the program continues to address a demonstrable need and is responsive to the needs of Canadians. |
1.1 What is the current and projected need for clinical and client care services in remote and isolated First Nations communities? |
2. Alignment with Government and First Nations Priorities Assessment of the linkages between the program objectives and (i) federal government priorities; (ii) departmental strategic outcomes; and (iii) First Nations priorities. |
2.1 Is the Clinical and Client Care Program aligned with federal government priorities? 2.2 Is the Clinical and Client Care Program aligned with departmental strategic outcomes? 2.3 Is the Clinical and Client Care Program aligned with First Nations' priorities? |
3. Alignment with Federal Roles and Responsibilities Assessment of the role and responsibilities for the federal government in delivering the program. |
3.1 Is the Clinical and Client Care Program aligned with federal roles and responsibilities? 3.2 Does the Clinical and Client Care Program duplicate, complement or overlap with other programs and services within Health Canada, other federal government departments, and/or provincial governments? 3.3 Are the clinical services provided in remote and isolated health facilities well integrated and consistent with the standard of care in the provincial jurisdiction? |
| Performance | |
4. Achievement of Expected Outcomes Assessment of progress toward expected outcomes (incl. immediate, intermediate and ultimate outcomes) with reference to performance targets and program reach, program design, including the linkage and contribution of outputs to outcomes |
To what extent has the Clinical and Client Care Program made progress towards the achievement of its outcomes? Immediate: 4.1 First Nations individuals, families and communities have access to clinical and client care services. 4.2 A trained workforce is in place to provide CCC Services. 4.3 Quality Clinical and Client Care services are delivered. Intermediate: 4.4 Clinical and client care services are sustainable Long Term 4.5 Clinical and client care services are responsive to the needs of First Nations in remote and isolated communities. Long Term 4.6 CCC programming contributes to the health status of First Nations in remote and isolated communities. |
5. Demonstration of Efficiency and Economy Economy Assessment of resource utilization in relation to the production of outputs and progress toward expected outcomes. |
5.1 Is the program using its existing resources optimally? 5.2 Has the program produced its outputs and achieved its outcomes in the most economical manner 5.3 Are there opportunities to enhance the coordination of program and services among federal and provincial jurisdictions? 5.4 To what extent has the program leveraged technology or other innovative approaches to service delivery? |
Data Collection and Analysis Methods
Sources of information used in this evaluation included literature review, document review, surveys, key informant interviews, and case studies. Data were analyzed by triangulating information gathered from the different sources and methods described below.
- Document, File and Data Review. A number of FNIHB internal documents and files, reviews, policies, manuals and other relevant documents were reviewed. These include but are not limited to: Nursing Station Reporting Templates, Nursing Dashboards, including agency nursing costs, training dashboards, sustainability reports, Nursing Stations Inventories, Essential Services dashboards, and other regional documents, files and data related to federal hospitals.
- Literature Review was limited to gray and other reports related to the health care needs, design and delivery of similar programs in remote and isolated communities, and past evaluations.
- Interviews with 46 Key Informants, including FNIHB Headquarters program staff (five), FNIHB regional offices representatives (nine), other Health Canada programs representatives (two), provincial governments (five), health directors (13), regional health authorities (nine), health associations (three). Out of 13 health directors interviewed, seven were from transferred communities.
- Survey of 118 health professionals working in communities, which health services managed by Health Canada or a First Nation. Most of the health professionals were RNs and Nurse Practitioners (61 percent), Nurse-in-Charge or Nurse Manager (31 percent), health directors (six percent), Program managers or directors (four percent), and other (doctor, paramedic, two percent). Of total number of health professionals surveyed, 14 percent worked for the Band Operated communities only, 58 percent worked for Health Canada managed services only, and 22 percent worked for both Health Canada and bands (five percent did not indicate).
To conduct the surveys, a list of Health Canada employed nurses-in charge or nurse managers was obtained. This list was updated and expanded on by regional FNIHB office to include all full-time and part-time RNs and nurse practitioners. The contact list of health professionals working in the First Nation managed communities is not normally maintained by Health Canada. To reach this population (12 communities in Saskatchewan, and nine in Quebec, and four in Ontario), an open link survey was created and sent to the nurse-in-charge or nurse managers in each of these communities. Nurse managers then forwarded the link to other health professionals working in their respective communities.
The survey response rate was approximately 32 percent. Since an open link was sent to nurses in Saskatchewan and Quebec transferred communities, it is not possible to calculate the response rate for these communities.
| Region | Survey Frame |
Bounced email /no phone |
Total Reached |
Completed | Response Rate |
|---|---|---|---|---|---|
| Alberta | 33 | 2 | 31 | 9 | 29% |
| Saskatchewan | 14 | 0 | 13 | 11 | n/a |
| Manitoba | 206 | 25 | 182 | 63 | 35% |
| Ontario | 201 | 76 | 126 | 26 | 21% |
| Quebec | 19 | 7 | 14 | 9 | n/a |
| Total | 476 | 110 | 366 | 118 | 32% |
- In total, seven case studies were conducted which included visits to five remote and isolated communities (one in each five regions) and one federal hospital in Manitoba. One case study involved a review of BC FNHA nursing services to identify potential best practices. In total, 73 one-on-one or group interviews were conducted as part of the community case studies and a Percy E. Moore Hospital visits in Manitoba. Of five community case studies, two were conducted in First Nation managed communities and three in communities with health services managed by Health Canada. The following table provides a detailed breakdown of interviews completed by type of community.
| Type of Case Study | Description |
|---|---|
| Communities with health services managed by First Nations (two) | A total of 33 representatives were interviewed, including:
|
| Communities with health services managed by Health Canada (three) | A total of 25 representativeswere interviewed, including:
|
| Percy E. Moore Hospital, Manitoba | A total of 15 representatives were interviewed, including:
|
In addition, the evaluators toured the facilities, and reviewed health plans for all communities, except Fox Lake, Alberta; and reviewed various documents provided by the hospital.
The BC FNHA case study included a review of publicly available documents, and phone interviews with seven representatives of BC FNHA and British Columbia provincial government.